| Admissions | Accreditation | Booksellers | Catalog | Colleges | Contact Us | Continents/States/Districts | Contracts | Examinations | Forms | Grants | Hostels | Honorary Doctorate degree | Instructors | Lecture | Librarians | Membership | Professional Examinations | Programs | Recommendations | Research Grants | Researchers | Students login | Schools | Search | Seminar | Study Center/Centre | Thesis | Universities | Work counseling |
Cardiac arrest is the sudden, abrupt loss of heart function. The victim may or may not have diagnosed heart disease. It's also called sudden cardiac arrest or unexpected cardiac arrest. Sudden death (also called sudden cardiac death) occurs within minutes after symptoms appear.
What causes cardiac arrest?
The most common underlying reason for patients to die suddenly from cardiac arrest is coronary heart disease. Most cardiac arrests that lead to sudden death occur when the electrical impulses in the diseased heart become rapid (ventricular tachycardia) or chaotic (ventricular fibrillation) or both. This irregular heart rhythm (arrhythmia) causes the heart to suddenly stop beating. Some cardiac arrests are due to extreme slowing of the heart. This is called bradycardia.
Other factors besides heart disease and heart attack can cause cardiac arrest. They include respiratory arrest, electrocution, drowning, choking and trauma. Cardiac arrest can also occur without any known cause.
Differential Diagnosis
Why did arrest occur?
Are there any other factors?
Can we reverse the cause(s)?
7 H's and 6 T's: pnemonic for mechanisms
* hypoxia
* hypovolemia
* hyperkalemia
* hypokalemia
* hypoglycemia
* hypothermia
* hydrogen ions (acidosis)
* thrombosis (MI)
* tension pneumothorax
* tamponade
* toxins/therapeutics
* thromboembolism
* trauma
Heart conditions that can lead to sudden cardiac arrest
More often, a life-threatening arrhythmia develops in a person with a pre-existing heart condition, such as:
* Coronary artery disease. Most cases of sudden cardiac arrest occur in people who have coronary artery disease. In coronary artery disease, your arteries become clogged with cholesterol and other deposits, reducing blood flow to your heart. This can make it harder for your heart to conduct electrical impulses smoothly.
* Heart attack. If a heart attack occurs, often as a result of severe coronary artery disease, it can trigger ventricular fibrillation and sudden cardiac arrest. In addition, a heart attack can leave behind areas of scar tissue. Electrical short circuits around the scar tissue can lead to abnormalities in your heart rhythm.
* Enlarged heart (cardiomyopathy). This occurs primarily when your heart's muscular walls stretch and enlarge or thicken. In both cases, your heart's muscle is abnormal, a condition that often leads to heart tissue damage and potential arrhythmias.
* Valvular heart disease. Leaking or narrowing of your heart valves can lead to stretching or thickening of your heart muscle, or both. When the chambers become enlarged or weakened because of stress caused by a tight or leaking valve, there's an increased risk of developing arrhythmia.
* Congenital heart disease. When sudden cardiac arrest occurs in children or adolescents, it may be due to a heart condition that was present at birth (congenital heart disease). Even adults who've had corrective surgery for a congenital heart defect still have a higher risk of sudden cardiac arrest.
* Electrical problems in the heart. In some people, the problem is in the heart's electrical system itself, instead of a problem with the heart muscle or valves. These are called primary heart rhythm abnormalities and include conditions such as Brugada's syndrome and long QT syndrome.
Can cardiac arrest be reversed?
Brain death and permanent death start to occur in just 4 to 6 minutes after someone experiences cardiac arrest. Cardiac arrest can be reversed if it's treated within a few minutes with an electric shock to the heart to restore a normal heartbeat. This process is called defibrillation. A victim's chances of survival are reduced by 7 to 10 percent with every minute that passes without CPR and defibrillation. Few attempts at resuscitation succeed after 10 minutes.
How many people survive cardiac arrest?
No statistics are available for the exact number of cardiac arrests that occur each year. It's estimated that more than 95 percent of cardiac arrest victims die before reaching the hospital. In cities where defibrillation is provided within 5 to 7 minutes, the survival rate from sudden cardiac arrest is as high as 30–45 percent.
What can be done to increase the survival rate?
Early CPR and rapid defibrillation combined with early advanced care can result in high long-term survival rates for witnessed cardiac arrest. For instance, in June 1999, automated external defibrillators (AEDs) were mounted 1 minute apart in plain view at Chicago's O'Hare and Midway airports. In the first 10 months, 14 cardiac arrests occurred, with 12 of the 14 victims in ventricular fibrillation. Nine of the 14 victims (64 percent) were revived with an AED and had no brain damage.
If bystander CPR was initiated more consistently, if AEDs were more widely available, and if every community could achieve a 20 percent cardiac arrest survival rate, an estimated 40,000 more lives could be saved each year. Death from sudden cardiac arrest is not inevitable. If more people react quickly by calling 9-1-1 and performing CPR, more lives can be saved.
Cardiopulmonary Resuscitation (CPR)
What is CPR?
Cardiopulmonary resuscitation (CPR) is a combination of rescue breathing and chest compressions delivered to victims thought to be in cardiac arrest. When cardiac arrest occurs, the heart stops pumping blood. CPR can support a small amount of blood flow to the heart and brain to “buy time” until normal heart function is restored.
Cardiac arrest is often caused by an abnormal heart rhythm called ventricular fibrillation (VF). When VF develops, the heart quivers and doesn't pump blood. The victim in VF cardiac arrest needs CPR and delivery of a shock to the heart, called defibrillation. Defibrillation eliminates the abnormal VF heart rhythm and allows the normal rhythm to resume. Defibrillation is not effective for all forms of cardiac arrest but it is effective to treat VF, the most common cause of sudden cardiac arrest.
Cardiac arrest refers to the loss of heart function. In many cases, it is an expected outcome to a serious illness. Cardiac arrest often results in death.
* Sudden cardiac arrest refers to the heart unexpectedly stopping activity due to a potentially reversible cause. Brain death occurs within a few minutes if the situation is not reversed.
o Sudden cardiac arrest may be caused by many different conditions. It does not necessarily mean that the person has had a heart attack.
* Sudden cardiac death refers to an unexpected, heart-related death within 1 hour from the start of symptoms.
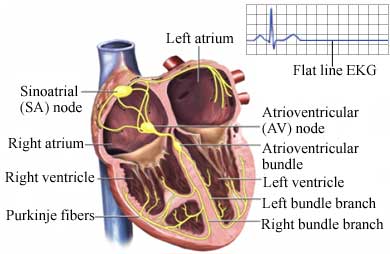
Electrical System of the Heart
Causes
Causes of cardiac arrest include:
* Ventricular fibrillation —a rapid, irregular heart rhythm preventing any circulation of blood (most common cause of sudden cardiac arrest)
* Ventricular tachycardia —a rapid but regular heart rhythm that, if sustained, may turn into ventricular fibrillation
* Dramatic slowing of heart rate due to failure of its pacemaker or severe heart block (interference with electrical conduction)
* Respiratory arrest
* Choking or drowning
* Electrocution
* Hypothermia
* Sudden loss of blood pressure
* Unknown causes
Risk Factors
A risk factor is something that increases your chance of getting a disease or condition.
Risk factors for cardiac arrest include:
* Coronary artery disease
* Heart attack
* Cardiomyopathy
* Enlarged heart
* Congenital heart disease
* Improperly functioning heart valves
* Conditions affecting the heart's electrical system
* Severe meta2bolic imbalances
* Adverse drug effects, such as from drugs to treat abnormal heart rhythms
* Lung conditions
* Trauma to the chest
* Extensive blood loss
* Excessive overexertion in people with heart disorders
* Use of illicit substances (eg, cocaine )
Symptoms
Symptoms include:
* Loss of consciousness
* No breathing
* No pulse
Prior to cardiac arrest, some patients report the following symptoms or warning signs in the weeks before the event:
* Chest pain
* Weakness
* Pounding in the chest
* Feeling faint
Diagnosis
The first person to respond to a cardiac arrest should check if the person is responsive. If the person does not respond, call 911 right away or have someone else call. If there is an automated external defibrillator (AED) available, you or someone else should get it and follow the steps on the machine.
After calling 911, CPR will be started if the person is not breathing normally. If no AED is available or while you are waiting for it, begin doing CPR by giving chest compressions. Push in the chest at least two inches at a fast rate of at least 100 compressions per minute. If you are trained in CPR, after 30 compressions, open the person's airway and give two rescue breaths. Then, continue with the chest compressions. If you feel more comfortable, you can give the compressions without the breaths until the ambulance arrives.
Treatment
Prompt treatment improves the chance of survival. The four steps in the cardiac chain of survival are:
Call 911
Immediately call for emergency medical support. Call 911 as soon as you notice cardiac warning signs or suspect a cardiac arrest has occurred.
Defibrillation
Defibrillation sends an electrical shock through the chest. The surge of electricity aims to stop the ineffective, irregular heart rhythm. This may allow the heart to resume a more normal electrical pattern. AEDs check the heart rhythm before instructing the rescuer to give the shock.
Start CPR
CPR helps keep blood and oxygen flowing to the heart and brain until other treatment can be given. The heart and brain are very susceptible to low oxygen levels. Permanent damage can occur, even with successful resuscitation.
Advanced Medical Care
Paramedics at the scene and doctors at the hospital provide essential medical care and intensive monitoring. They will give drugs, insert a tube to maintain an open airway, and manage emergency care. Epinephrine is often given early to make the heart more receptive to electrical impulses and improve blood flow to the heart and brain. The patient will receive oxygen. Even if an effective heart rhythm is restored, low oxygen levels may cause serious complications, including damage to the heart, brain, and other vital organs. The emergency medical personnel may perform an electrocardiogram (ECG, EKG)—a test that records the heart's activity by measuring electrical currents through the heart muscle.
Doctors will attempt to find and correct the underlying cause of the cardiac arrest. At the hospital, the doctor will ask about symptoms prior to the collapse and the patient's medical and drug history.
If the patient survives, the doctor will:
* Assess the electrocardiogram.
* Perform a physical exam.
* Confirm a cardiac arrest has occurred.
* Look for the cause.
* Evaluate the effects of pre-hospital care.
* Order additional blood and diagnostic tests to help determine the cause of the arrest.
A telemetry machine will continually monitor the heart's electrical activity.
Prevention
Become aware of heart disease warning signs and promptly seek treatment for any that develop. If you do not have a heart condition, follow the rules of primary prevention of heart disease. If you have a heart condition or may be at high risk for one, ask your doctor about how to reduce your risk of sudden cardiac arrest. You might be a right candidate for certain medications that prevent heart arrhythmias or implantation of an implantable cardioverter defibrillator (ICD) device.
Also, if you are known to be at high risk, you may consider purchasing an automatic external defibrillator (AED) for home use. Discuss it with your doctor.
http://www.americanheart.org/presenter.jhtml?identifier=4481
http://www.aurorahealthcare.org/yourhealth/healthgate/getcontent.asp?URLhealthgate=11981.html
