Or
Fating blood sugar less than 110 mg/dl
70 to 110 mg/dl
After eating 110 to 140 mg/dl

|
 Or Fating blood sugar less than 110 mg/dl 70 to 110 mg/dl After eating 110 to 140 mg/dl |
|
What medical emergencies can occur due to this medical condition? Diabetic ketoacidosis Hyperosmolar hyperglycemia. What is glucose? Glucose is a simple sugar (monosaccharide) and an important carbohydrate in biology. Blood Glucose Monitoring Devices Do you have a blood glucose monitoring device? What are the types of blood glucose monitoring devices? How do blood glucose monitoring devicee work? What are the features of the blood glucose monitoring device you recommend? How is human blood glucose measured? What is the role of insulin and glycogen in blood glucose regulation? What are the uses of glucose to the human body? What should you elaborate about a human organ? What is the gross anatomy of this human organ? What are the attachments of this human organ? What is the arterial, venous supply to this human organ? What is the nerve supply to this human organ? What is the lymphatic supply to this human organ? What are the functions of this human organ? What medical conditions are associated with any problems with this human organ? What is the function of the human pancreas? What medical conditions are associated with any problem with the human pancreas? Do you have a blood glucose monitoring device that you can use yourself at home? There is an automated a blood glucose monitoring device that you can use yourself at home. Before coming out of bed in the morning, check your blood pressure and blood glucose. Forward the results via e-mail, fax, telephone, or postal mail. Do you have diabetes? Do you know anyone who has diabetes? These questions are for the patient or his/her caretaker. How do you regularly measure your blood sugar? What blood glucose monitoring device or machine do you utilize for blood sugar measurement? Do you have any health-related problem as of November 23, 2011? Do you have any problem as of November 23, 2011? Is this a new problem or recurrence of a previous problem? When and where was your last blood sugar test done? Was the blood sugar test done fasting, after a meal, or randomly? What blood glucose monitoring device or machine was utilized for blood sugar measurement? What was the result of your last blood sugar test? Have you taken any medication up to now for this particular medical condition? Questions will remain the same. In certain situations, answers need to be modified. What is endocrinology? What is the endocrine system? What do endocrinologists do? What is an endocrinologist? |
| Questions To Ask Your Doctor About Diabetes |
|
Glycolysis & Gluconeogenesis Glycogen/Starch, Pentose Phosphate Pathway Membrane Transport Facilitated Glucose Transport Mitochondrial Carriers Energy Metabolism Citric Acid Cycle Oxidative Phosphorylation Lipid Metabolism Fatty Acid Metabolism Phospholipids and Membrane Biosynthesis Glycolipids and Glycoproteins Cholesterol, Bile Acids, and Steroid Hormones Nitrogen Metabolism Nitrogen Fixation and Urea Cycle Amino Acid Metabolism Neurotransmitters Nucleic Acid Metabolism Nitric oxide |
|
Definition
What is diabetes? Diabetes mellitus, often simply referred to as diabetes, is a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or because cells do not respond to the insulin that is produced. This high blood sugar produces the classical symptoms of polyuria (frequent urination), polydipsia (increased thirst) and polyphagia (increased hunger). Causes What are the causes of a temporary increase in blood sugar? Stress Dehydration Not exercising enough Intake of food, especially high carbohydrate diet. What causes diabetes? The cause of diabetes depends on the type. Type 1 diabetes is partly inherited and then triggered by certain infections, with some evidence pointing at Coxsackie B4 virus. There is a genetic element in individual susceptibility to some of these triggers which has been traced to particular HLA genotypes (i.e., the genetic "self" identifiers relied upon by the immune system). However, even in those who have inherited the susceptibility, type 1 diabetes mellitus seems to require an environmental trigger. Type 2 diabetes is due primarily to lifestyle factors and genetics.[18] Following is a comprehensive list of other causes of diabetes:[19] * Genetic defects of β-cell Function o Maturity onset diabetes of the young (MODY) o Mitochondrial DNA mutations * Genetic defects in insulin processing or insulin action o Defects in proinsulin conversion o Insulin gene mutations o Insulin receptor mutations * Exocrine Pancreatic Defects o Chronic pancreatitis o Pancreatectomy o Pancreatic neoplasia o Cystic fibrosis o Hemochromatosis o Fibrocalculous pancreatopathy * Endocrinopathies o Growth hormone excess (acromegaly) o Cushing syndrome o Hyperthyroidism o Pheochromocytoma o Glucagonoma * Infections o Cytomegalovirus infection o Coxsackievirus B * Drugs o Glucocorticoids o Thyroid hormone o β-adrenergic agonists Types What are the different types of diabetes? There are three main types of diabetes: * Type 1 diabetes: results from the body's failure to produce insulin, and presently requires the person to inject insulin. (Also referred to as insulin-dependent diabetes mellitus, IDDM for short, and juvenile diabetes.) * Type 2 diabetes: results from insulin resistance, a condition in which cells fail to use insulin properly, sometimes combined with an absolute insulin deficiency. (Formerly referred to as non-insulin-dependent diabetes mellitus, NIDDM for short, and adult-onset diabetes.) * Gestational diabetes: is when pregnant women, who have never had diabetes before, have a high blood glucose level during pregnancy. It may precede development of type 2 DM. Other forms of diabetes mellitus include congenital diabetes, which is due to genetic defects of insulin secretion, cystic fibrosis-related diabetes, steroid diabetes induced by high doses of glucocorticoids, and several forms of monogenic diabetes. All forms of diabetes have been treatable since insulin became available in 1921, and type 2 diabetes may be controlled with medications. Both type 1 and 2 are chronic conditions that usually cannot be cured. Pancreas transplants have been tried with limited success in type 1 DM; gastric bypass surgery has been successful in many with morbid obesity and type 2 DM. Gestational diabetes usually resolves after delivery. Diabetes without proper treatments can cause many complications. Acute complications include hypoglycemia, diabetic ketoacidosis, or nonketotic hyperosmolar coma. Serious long-term complications include cardiovascular disease, chronic renal failure, retinal damage. Adequate treatment of diabetes is thus important, as well as blood pressure control and lifestyle factors such as smoking cessation and maintaining a healthy body weight. As of 2000 at least 171 million people worldwide have diabetes, or 2.8% of the population.[2] Most cases of diabetes mellitus fall into three broad categories: type 1, type 2, and gestational diabetes. A few other types are described. The term diabetes, without qualification, usually refers to diabetes mellitus. The rare disease diabetes insipidus has similar symptoms as diabetes mellitus, but without disturbances in the sugar metabolism (insipidus meaning "without taste" in Latin). The term "type 1 diabetes" has replaced several former terms, including childhood-onset diabetes, juvenile diabetes, and insulin-dependent diabetes mellitus (IDDM). Likewise, the term "type 2 diabetes" has replaced several former terms, including adult-onset diabetes, obesity-related diabetes, and non-insulin-dependent diabetes mellitus (NIDDM). Beyond these two types, there is no agreed-upon standard nomenclature. Various sources have defined "type 3 diabetes" as: gestational diabetes,[6] insulin-resistant type 1 diabetes (or "double diabetes"), type 2 diabetes which has progressed to require injected insulin, and latent autoimmune diabetes of adults (or LADA or "type 1.5" diabetes). Type 1 diabetes Type 1 diabetes mellitus is characterized by loss of the insulin-producing beta cells of the islets of Langerhans in the pancreas leading to insulin deficiency. This type of diabetes can be further classified as immune-mediated or idiopathic. The majority of type 1 diabetes is of the immune-mediated nature, where beta cell loss is a T-cell mediated autoimmune attack.[8] There is no known preventive measure against type 1 diabetes, which causes approximately 10% of diabetes mellitus cases in North America and Europe. Most affected people are otherwise healthy and of a healthy weight when onset occurs. Sensitivity and responsiveness to insulin are usually normal, especially in the early stages. Type 1 diabetes can affect children or adults but was traditionally termed "juvenile diabetes" because it represents a majority of the diabetes cases in children. "Brittle" diabetes, also known as unstable diabetes or labile diabetes, is a term that was traditionally used to describe to dramatic and recurrent swings in glucose levels, often occurring for no apparent reason in insulin-dependent diabetes. This term, however, has no biologic basis and should not be used.[9] There are many different reasons for type 1 diabetes to be accompanied by irregular and unpredictable hyperglycemias, frequently with ketosis, and sometimes serious hypoglycemias, including an impaired counterregulatory response to hypoglycemia, occult infection, gastroparesis (which leads to erratic absorption of dietary carbohydrates), and endocrinopathies (eg, Addison's disease). These phenomena are believed to occur no more frequently than in 1% to 2% of persons with type 1 diabetes. Type 2 diabetes Type 2 diabetes mellitus is characterized by insulin resistance which may be combined with relatively reduced insulin secretion. The defective responsiveness of body tissues to insulin is believed to involve the insulin receptor. However, the specific defects are not known. Diabetes mellitus due to a known defect are classified separately. Type 2 diabetes is the most common type. In the early stage of type 2 diabetes, the predominant abnormality is reduced insulin sensitivity. At this stage hyperglycemia can be reversed by a variety of measures and medications that improve insulin sensitivity or reduce glucose production by the liver. Gestational diabetes Gestational diabetes mellitus (GDM) resembles type 2 diabetes in several respects, involving a combination of relatively inadequate insulin secretion and responsiveness. It occurs in about 2%–5% of all pregnancies and may improve or disappear after delivery. Gestational diabetes is fully treatable but requires careful medical supervision throughout the pregnancy. About 20%–50% of affected women develop type 2 diabetes later in life. Even though it may be transient, untreated gestational diabetes can damage the health of the fetus or mother. Risks to the baby include macrosomia (high birth weight), congenital cardiac and central nervous system anomalies, and skeletal muscle malformations. Increased fetal insulin may inhibit fetal surfactant production and cause respiratory distress syndrome. Hyperbilirubinemia may result from red blood cell destruction. In severe cases, perinatal death may occur, most commonly as a result of poor placental perfusion due to vascular impairment. Labor induction may be indicated with decreased placental function. A cesarean section may be performed if there is marked fetal distress or an increased risk of injury associated with macrosomia, such as shoulder dystocia. A 2008 study completed in the U.S. found that the number of American women entering pregnancy with preexisting diabetes is increasing. In fact the rate of diabetes in expectant mothers has more than doubled in the past 6 years.[12] This is particularly problematic as diabetes raises the risk of complications during pregnancy, as well as increasing the potential that the children of diabetic mothers will also become diabetic in the future. Other types Pre-diabetes indicates a condition that occurs when a person's blood glucose levels are higher than normal but not high enough for a diagnosis of type 2 diabetes. Many people destined to develop type 2 diabetes spend many years in a state of pre-diabetes which has been termed "America's largest healthcare epidemic."[13]:10–11 Latent autoimmune diabetes of adults is a condition in which Type 1 diabetes develops in adults. Adults with LADA are frequently initially misdiagnosed as having Type 2 diabetes, based on age rather than etiology. Some cases of diabetes are caused by the body's tissue receptors not responding to insulin (even when insulin levels are normal, which is what separates it from type 2 diabetes); this form is very uncommon. Genetic mutations (autosomal or mitochondrial) can lead to defects in beta cell function. Abnormal insulin action may also have been genetically determined in some cases. Any disease that causes extensive damage to the pancreas may lead to diabetes (for example, chronic pancreatitis and cystic fibrosis). Diseases associated with excessive secretion of insulin-antagonistic hormones can cause diabetes (which is typically resolved once the hormone excess is removed). Many drugs impair insulin secretion and some toxins damage pancreatic beta cells. The ICD-10 (1992) diagnostic entity, malnutrition-related diabetes mellitus (MRDM or MMDM, ICD-10 code E12), was deprecated by the World Health Organization when the current taxonomy was introduced in 1999. Prevention Why shouldn't a medical doctor advise a patient with high blood sugar to take different diet? Every person needs specific daily calories based on his or her age, sex, weight, height, and level of activity. These daily calories should have consumable proteins, carbohydrates, fats, etc. Experience and research have proved people who take different diet or take fewer calories can get emaciated, and have their body mass index reduced. That is not recommended. What measures should be taken to prevent this medical condition? Exercise every day. |
|
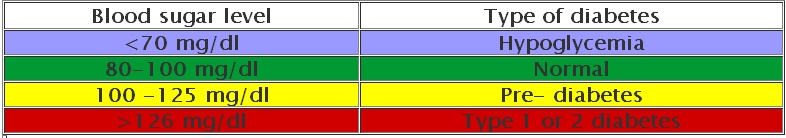
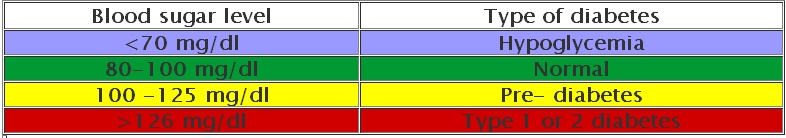
Diabetes: What can the various complications be? Acute emergency like diabetic ketoacidosis and hyperosmolar coma Chronic complications of diabetes Diabetic eye disease Diabetic foot Gum disease Diabetic heart disease Diabetic kidney disease Diabetic nerve problems (diabetic neuropathy) Diabetic sexual and bladder problems Diabetic skin conditions Other How does this interfere with your daily routine? Indicate if this interferes with activities of your daily routine. How should you interpret human blood glucose levels? Blood sugar level Type of diabetes Less than 70 mg/dl Hypoglycemia 80-100 mg/dl Normal 100-125 mg/dl Pre-diabetes More than 126 mg/dl Type 1 or 2 diabetes This is the norm in various regions. Normal Blood Sugar Fasting blood sugar less than 110 mg/dl 70 to 110 mg/dl After eating 110 to 140 mg/dl What have statistics revealed? Before January 1, 2022, this disease killed 1.5 million people worldwide every year. What has recent research revealed? Genes are implicated in many diabetes patients. What must you try before relying on medication? If lifestyle changes such as losing weight, eating healthy foods, and regularly engaging in moderate physical activity aren’t managing your blood glucose levels, you may need medication to help reduce your glucose levels and your risk for heart disease and stroke. What is the first line of medication? People newly diagnosed with Type 2 diabetes are prescribed metformin as a first line of therapy, in addition to lifestyle changes. Metformin decreases the amount of glucose made in your liver. If this does not control your blood sugar, a healthcare professional can add a GLP-1 receptor agonist or SGLT-2 inhibitor to your regimen. Insulin can be prescribed for both types of diabetes to regulate your blood sugar. Insulin by syringe, insulin pen, and insulin pump What are the types of insulin? 1. Inhaled insulin according to the American Heart Association 2. Rapid-acting insulin 3. Regular or short-acting insulin 4. Intermediate-acting insulin 5. Long-acting insulin 6. Ultra-long-acting insulin reaches the bloodstream in six hours, does not peak, and lasts 36 hours or more. What are the complications of this medication? Hypoglycemia. How can the complications of this medication be prevented? 1. Try your best with lifestyle changes first, such as losing weight. 2. Eat healthy foods 3. Regularly engage in moderate physical activity This can control your blood sugar. 4. Take medication under the advice and close supervision of specific physicians and medical team to prevent complications. Before January 1, 2022, at least 1.5 million people died every year due to diabetes. No one knows how many died each year due to complications from diabetes medication before January 1, 2022. Further research is required. As of January 31, 2022, the University of California San Francisco (UCSF) Diabetes Center at 513 Parnassus Avenue, San Francisco, CA 94143 https://diabetes.ucsf.edu/, had not elaborated in on the required questions and answers. You are encouraged to circulate these questions and answers from Dr. Asif Qureshi, who can guide 69 types of specific physicians, as evidenced at www.qureshiuniversity.com/physicians.html. |