| Admissions | Accreditation | Booksellers | Catalog | Colleges | Contact Us | Continents/States/Districts | Contracts | Examinations | Forms | Grants | Hostels | Honorary Doctorate degree | Instructors | Lecture | Librarians | Membership | Professional Examinations | Programs | Recommendations | Research Grants | Researchers | Students login | Schools | Search | Seminar | Study Center/Centre | Thesis | Universities | Work counseling |
|
Hearing impairment What is the difference between deafness, hearing impairment, and hearing loss? What are types of hearing impairment? How should children be tested for any hearing impairment? How do you quantify hearing impairment? What causes hearing impairment? How is hearing impairment diagnosed? How is hearing impairment treated? What is cochlear implant surgery? A statement from a medical college from Srinagar, Kashmir, on May 14, 2011, declares that the procedure can be performed successfully on a child 2–3 years old. Can you diagnose deafness in a 2-3-year-old? A child may have delayed developmental milestones. Does that mean he or she is deaf? Inability to hear (deaf) and inability to speak (dumb) are two different diagnoses. What cases need auditory and speech rehabilitation? How is deafness diagnosed? How is deafness treated? Here are further guidelines. Ear, Nose and Throat Topics 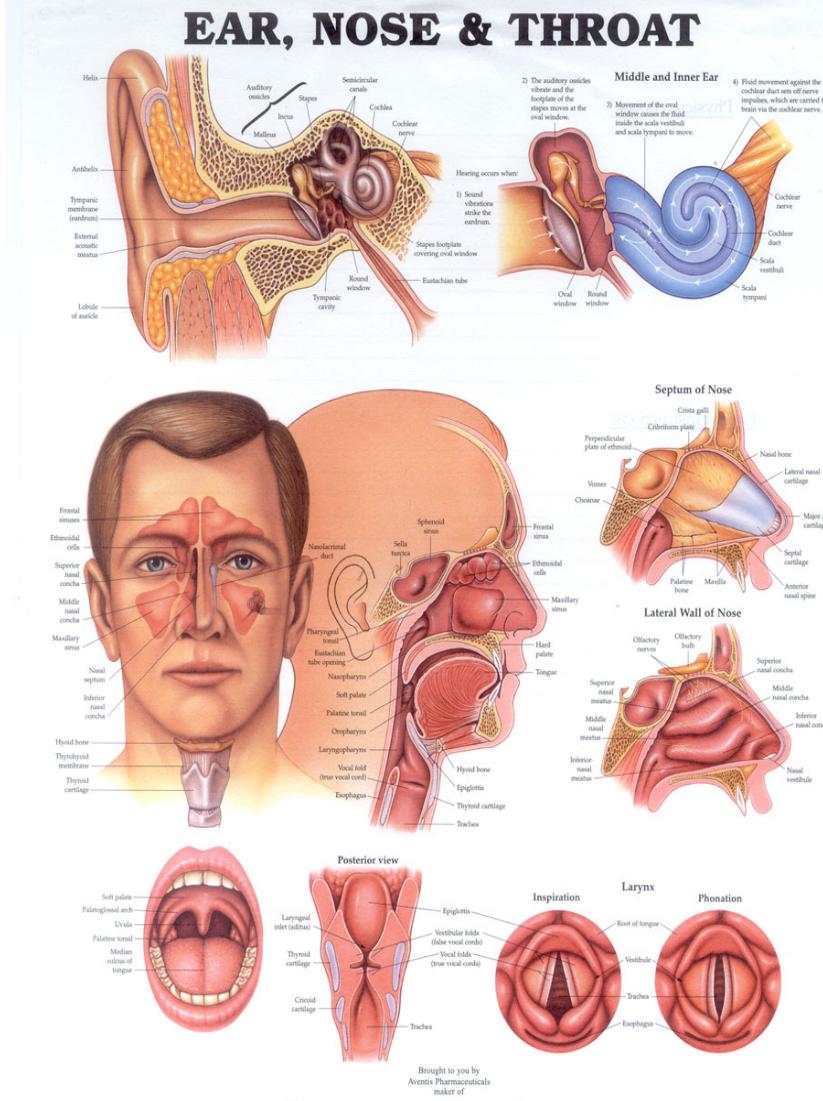 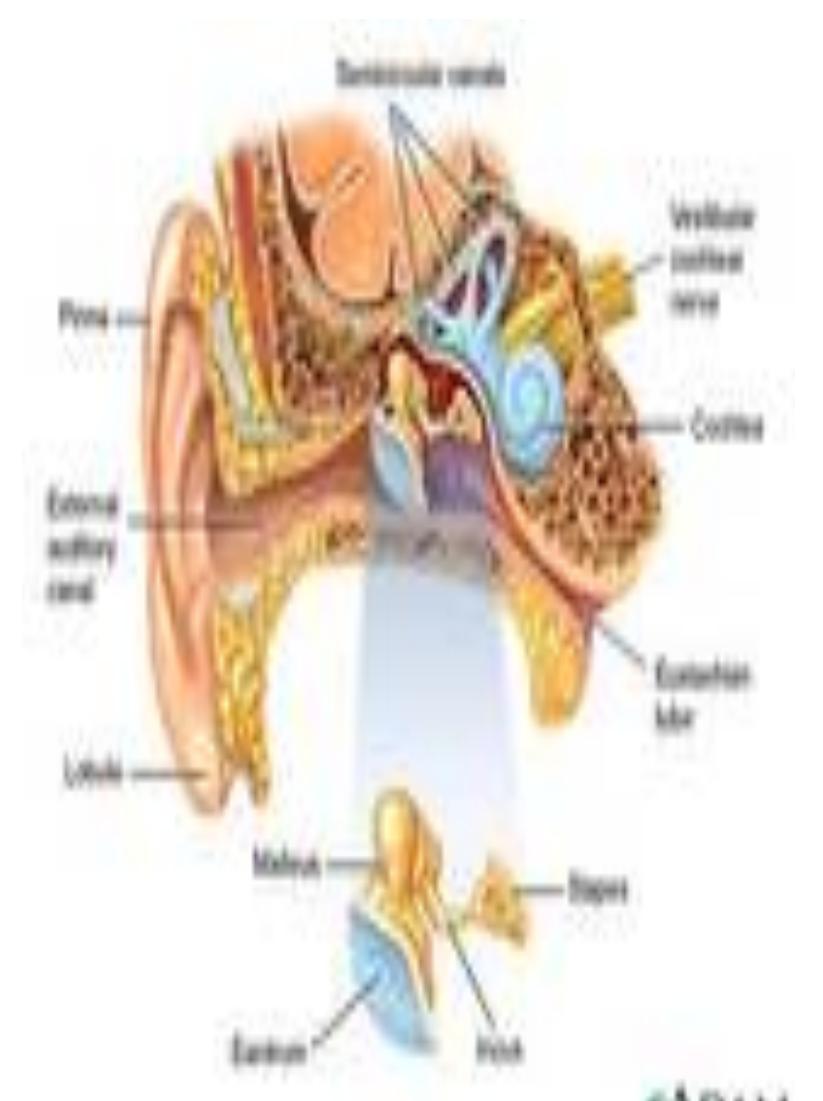 What Is an ENT Specialist? Otolaryngology or ENT (ear, nose, and throat) is the branch of medicine and surgery that specializes in the diagnosis and treatment of ear, nose, throat, and head and neck disorders. The full name of the specialty is otolaryngology–head and neck surgery. Practitioners are called otolaryngologists–head and neck surgeons, or sometimes otorhinolaryngologists (ORL). * A/B Otic * Acetasol * Acetasol HC * acetic acid (otic) * acetic acid and aluminum acetate otic * acetic acid and hydrocortisone (otic) * antipyrine and benzocaine otic * Auraphene-B * Auro Ear Drops * Aurodex * benzocaine otic * Bullous Myringitis * carbamide peroxide (otic) * Cerumen * Cerumenex * Cetraxal * chloroxylenol and pramoxine otic * Cipro HC * Ciprodex * ciprofloxacin and dexamethasone otic * ciprofloxacin and hydrocortisone otic * ciprofloxacin otic * Debrox * Domeboro Otic * Ear Ache * Ear Infection * Ear Infection * Ear Infections - Source: Healthwise * Ear Infections: Antibiotics Often Not Needed * Ear Tubes * Ear Wax * Ear Wax Removal * Ear, Patella, Short Stature Syndrome - Source: Healthwise * Ear, Perforated * Earache * Eardrum, Perforated * Earwax * Earwax - Source: Healthwise Floxin Otic * Hearing Loss * Hearing Loss Is High, but Hearing Aid Use Is Low * Impacted Earwax * Infection, Ear * Meniere Disease * Mollifene * Murine Ear Drops * Myringitis * Myringotomy * ofloxacin otic * Oticaine * Otitis Externa * Otitis Media * Outer Ear Infection * Pain in the Ear * Perforated Eardrum * Picture of Ear Anatomy * Pramotic * Punctured Eardrum * Roller-Coaster Ride Could Affect Your Ears * Rx-Otic * Slideshow Anatomy of an Ear Infection * Slideshow Pictures Tinnitus Ringing Ears * Star-Otic * Strep Throat - Source: Healthwise * Strep Throat * Streptococcus, Group B - Source: Healthwise * Swimmer's Ear * Throat, Strep * Tinnitus * triethanolamine polypeptide oleate (otic) * Tympanostomy Tubes * Uni-Otic Ear Drops * Vestibular Neuritis - Source: Healthwise * Wax, Ear * Wilderness: Ear Infection * Achalasia see Esophagus Disorders * Acoustic Neuroma * Adenoidectomy see Tonsils and Adenoids * Adenoids see Tonsils and Adenoids * Ageusia see Taste and Smell Disorders * Allergy * Anaphylaxis see Allergy * Anatomy * Anosmia see Taste and Smell Disorders * Aphthous Ulcers see Mouth Disorders * Auditory Tumor see Acoustic Neuroma * Balance Disorders see Dizziness and Vertigo * Barrett's Esophagus see Esophagus Disorders * Basedow's Disease see Thyroid Diseases * Canker Sore see Mouth Disorders * Cardiospasm see Esophagus Disorders * Cochlear Implants * Cold, Common see Common Cold * Common Cold * Cough * Craniofacial Injuries see Facial Injuries and Disorders * Croup see Throat Disorders * Deafness see Hearing Disorders and Deafness * Diphtheria * Dizziness and Vertigo * Dysgeusia see Taste and Smell Disorders * Dysosmia see Taste and Smell Disorders * Ear Disorders * Ear Infections * Esophageal Cancer * Esophagus Disorders * Facial Injuries and Disorders * Goiter see Thyroid Diseases * Graves' Disease see Thyroid Diseases * Hashimoto's Disease see Thyroid Diseases * Hay Fever * Head and Neck Cancer * Hearing Aids * Hearing Disorders and Deafness * Hearing Problems in Children * Hypersensitivity see Allergy * Hyperthyroidism see Thyroid Diseases * Hypothyroidism see Thyroid Diseases * Laryngitis see Throat Disorders * Larynx Cancer see Head and Neck Cancer * Meniere's Disease * Mouth Disorders * Nasal Cancer * Nasal Disorders see Nose Disorders * Neuroma, Acoustic see Acoustic Neuroma * Noise * Nose Disorders * Nosebleed see Nose Disorders * Otitis Media see Ear Infections * Overactive Thyroid see Thyroid Diseases * Paranasal Sinus Cancer see Nasal Cancer * Pharyngitis see Sore Throat * Pharynx Cancer see Head and Neck Cancer * Pharynx Disorders see Throat Disorders * Presbycusis see Hearing Disorders and Deafness * Rheumatic Fever see Streptococcal Infections * Scarlet Fever see Streptococcal Infections * Sinus Infection see Sinusitis * Sinusitis * Smelling Disorders see Taste and Smell Disorders * Snoring * Sore Throat * Strep Throat see Streptococcal Infections * Streptococcal Infections * Swimmer's Ear see Ear Infections * Taste and Smell Disorders * Throat Cancer see Head and Neck Cancer * Throat Disorders * Thyroid Cancer * Thyroid Diseases * Tinnitus * Tonsillectomy see Tonsils and Adenoids * Tonsillitis see Tonsils and Adenoids * Tonsils and Adenoids * Underactive Thyroid see Thyroid Diseases * Usher Syndrome * Vertigo see Dizziness and Vertigo * Vestibular Diseases see Dizziness and Vertigo; Meniere's Disease * Vestibular Schwannoma see Acoustic Neuroma * Voicebox Disorders see Throat Disorders * Achalasia see Esophagus Disorders * Acoustic Neuroma * Adenoidectomy see Tonsils and Adenoids * Adenoids see Tonsils and Adenoids * Ageusia see Taste and Smell Disorders * Allergy * Anaphylaxis see Allergy * Anatomy * Anosmia see Taste and Smell Disorders * Auditory Tumor see Acoustic Neuroma * Balance Disorders see Dizziness and Vertigo * Barrett's Esophagus see Esophagus Disorders * Basedow's Disease see Thyroid Diseases * Canker Sore see Mouth Disorders * Cardiospasm see Esophagus Disorders * Cochlear Implants * Cold, Common see Common Cold * Common Cold * Cough * Craniofacial Injuries see Facial Injuries and Disorders * Croup see Throat Disorders * Deafness see Hearing Disorders and Deafness * Diphtheria * Dizziness and Vertigo * Dysgeusia see Taste and Smell Disorders * Dysosmia see Taste and Smell Disorders * Ear Disorders * Ear Infections * Esophageal Cancer * Esophagus Disorders * Facial Injuries and Disorders * Goiter see Thyroid Diseases * Graves' Disease see Thyroid Diseases * Hashimoto's Disease see Thyroid Diseases * Hay Fever * Head and Neck Cancer * Hearing Aids * Hearing Disorders and Deafness * Hearing Problems in Children * Hypersensitivity see Allergy * Hyperthyroidism see Thyroid Diseases * Hypothyroidism see Thyroid Diseases * Laryngitis see Throat Disorders * Larynx Cancer see Head and Neck Cancer * Meniere's Disease * Mouth Disorders * Nasal Cancer * Nasal Disorders see Nose Disorders * Neuroma, Acoustic see Acoustic Neuroma * Noise * Nose Disorders * Otitis Media see Ear Infections * Paranasal Sinus Cancer see Nasal Cancer * Pharyngitis see Sore Throat * Pharynx Cancer see Head and Neck Cancer * Pharynx Disorders see Throat Disorders * Presbycusis see Hearing Disorders and Deafness * Rehumatic Fever see Streptococcal Infections * Scarlet Fever see Streptococcal Infections * Sinusitis * Smelling Disorders see Taste and Smell Disorders * Snoring * Sore Throat * Strep Throat see Streptococcal Infections * Streptococcal Infections * Swimmer's Ear see Ear Infections * Taste and Smell Disorders * Throat Cancer see Head and Neck Cancer * Throat Disorders * Thyroid Cancer * Thyroid Diseases * Tinnitus * Tonsillectomy see Tonsils and Adenoids * Tonsillitis see Tonsils and Adenoids * Tonsils and Adenoids * Usher Syndrome * Vertigo see Dizziness and Vertigo * Vestibular Diseases see Dizziness and Vertigo; Meniere's Disease * Vestibular Schwannoma see Acoustic Neuroma * Voicebox Disorders see Throat Disorders http://www.nlm.nih.gov/medlineplus/earnoseandthroat.html http://www.netdoctor.co.uk/ate/health/ear_nose_throat/600229.shtml General ENT questions * Can I buy a CPAP machine? * Dizziness, nausea and hearing problems * Echinacea for my daughter's colds? * How can I deal with travel sickness? * I can't yawn * I get an upset stomach every time I get a cold * I have a rare brain disorder * I wake at night unable to breathe * I'm pregnant and feel like I have a permanent heavy cold * Is my cough related to my allergy? * Is my office making me sick? * Is Parkinson's making my cold worse? * Is this glandular fever? * I've lost my voice * My family all suffer from dry and swollen mucous membranes * My head fizzes when I fly * Ramsey Hunt Syndrome * Side-effect of 'flu jab? * What are good treatments for hay fever? * What hay fever remedies can be used with asthma drugs? * What is geographical tongue? * What is Lemierre's disease? * When I travel I get severe headaches during the aircraft's descent * Why is my eye bloodshot? Ear * A sensitivity to noise * Adult glue - ear * Are there any advances in hearing aids? * Aural airtravel trouble * Blocked ears - risks when flying? * Can earplugs be harmful? * Can I do anything for labyrinthitis * Catarrh behind the eardrum * Clicky ears * Crackling ears * Flying causes tremendous pain in my ears * Grommets have left my head feeling 'full' * Hopi ear candles * I get earache from using the telephone * I have otits media. Can I fly to Argentina? * I have punctured my eardrum * I wear earplugs because of my partner’s snoring. Will this damage my ears? * I’ve perforated my eardrum. How serious is this? * Irritating ears * Is dark brown earwax a potential problem? * Is loud music damaging my hearing? * Is my ear problem due to the flu? * Is my telephone job sending me deaf? * Is there a cure for tinnitus? * Is there a link between labyrinthitis and MS? * Labyrinthitis - what are the options? * My daughter has had a grommet insertion * My ears stick out * My tinnitus is getting worse * Perforated eardrum * Poor hearing * Should I be worried about my bleeding ears? * Sticking out ears * Tinnitus and hearing * Treatment for labyrinthitis * Vertigo treatment * What is a collapsed eardrum? * What is barotrauma? * What is the procedure for a perforated ear drum? * What's the best way of cleaning out my ears? * What's the best way to get rid of ear wax? * Why do I get ear ache * Why won't my ears go pop? * Worried about my hearing Nose * Cosmetic surgery for crooked nose * Heightened sense of smell * Help for red nose * How can I prevent recurrences of sinusitis? * I need my sinuses drained * I received a blow to the nose and now have problems breathing * I want my sense of smell back! * Infected sinuses * Inflamed nose * My daughter has a discharge from her nose * My daughter has a persistent discharge from her nose * My daughter has no sense of smell * My mother can't smell * My nose is growing bigger * My nostril drips constantly * My snoring is jeopardising our relationship * My son has a non-stop runny nose * My son keeps having nose bleeds * Nasal bleeding * Nasal surgery * Post nasal drip * Snoring nightmare * There's a hole in my septum. * What causes nosebleeds? * What could be causing my cracked, swollen nose? * What's causing my nosebleeds? * Why do I constantly have a runny nose? * Will my sense of smell come back? * Will the smell from the sewage works do me any harm? * Will using Nasonex every day cause any long-term problems? Throat * Can I avoid a sore throat? * Constant bad breath * Difficulty swallowing - how will I be treated? * Help for lost voice * How can I get rid of a furry tongue? * How can I reassure my daughter who is about to have a tonsillectomy? * How can I soothe my tonsillitis? * I am a singer – how can I protect my voice? * I have a polyp on my vocal cords * I keep getting tonsillitis * I'm a teacher but I can't shout! * Is my medication causing a dry throat? * Is there an over-the-counter treatment for mouth ulcers? * I've got bad breath * Mucous in the throat * My daughter has bad breath and a coated tongue * My throat hurts every time I swallow * My voice hasn't broken yet. * No smell or taste - what's happening? * Papillomas on the vocal chords * Recurrent tonsillitis and sore skin * Sore throat and feeling ill * Sore throat because of tonsillitis * Swollen tonsils * Throat complaint * What can I do about my recurring tonsillitis? * What is a quinsy? * What is nutcracker oesophagus? * What is strep throat? * What is wrong with my tonsils? * Will a tonsillectomy make me more prone to infections? * Will a tonsillectomy stop me singing? * Will I ever be able to sing again? http://www.pamf.org/ENT/faqs.html Ears, Nose and Throat (ENT) Frequently Asked Questions * Decrease Font Size * Increase Font Size * Send to a Friend * Share o Share / Blog o Digg This o del.icio.us o Newsvine o Facebook o Reddit o Furl It o !Y My Web o Google * Print * What are common causes of nasal obstruction? * What causes sinusitis and how is it treated? * At what point would my child benefit from a tonsillectomy and adenoidectomy? * What causes my hoarseness? * What can be done about my snoring? What are common causes of nasal obstruction? Common causes of nasal obstruction include a deviated nasal septum, nasal turbinate enlargement, and nasal polyps (benign growths.) Deviated nasal septum: The midline of the nose consists of a cartilage and bony nasal septum that separates the two sides of the nasal cavity. A deviation or bend in this structure can be present at birth or can occur following a nasal fracture. The obstruction caused by such a deviation can be corrected by surgically straightening the septum, called a septoplasty. A septoplasty is a commonly performed outpatient surgery done through incisions within the nasal cavity, removing the obstructing portion of bone and cartilage. Nasal turbinate enlargement: The nasal turbinates are three bony and soft-tissue structures lining the sides of the nasal cavity. As part of the normal nasal cycle, the turbinates alternately swell and enlarge. In some persons, the turbinates can be excessively large, resulting in significant nasal obstruction. Allergy treatment, typically with nasal steroid sprays, may help to decrease this swelling. When allergy management does sufficiently relieve nasal obstruction, the inferior turbinates can be surgically reduced. In many cases this can be done as an office procedure. Nasal polyps: Nasal polyps are a type of inflammatory tissue that can grow in the nasal cavity and sinuses. They occur more frequently in persons with allergies and/or asthma. Nasal obstruction is the most common symptom. The sinus drainage tracts may also be blocked, resulting in chronic sinus disease. Nasal polyps are controlled with steroid sprays as well as removal by endoscopic surgery. Persons whose polyps arise from asthma may have serious allergic reactions to aspirin. Back to top What causes sinusitis and how is it treated? Infection of the sinus cavities often occurs due to inflammation and obstruction of the sinus drainage pathways. Typical symptoms of a sinus infection include facial pain and pressure, nasal obstruction, yellow or green nasal drainage, fatigue and fever. Treatment of a sinus infection may include nasal decongestants and antibiotics. People with chronic sinus drainage may benefit from endoscopic sinus surgery. Back to top At what point would my child benefit from a tonsillectomy and adenoidectomy? Surgical removal of the tonsils and adenoids in children is performed for two primary reasons: recurrent tonsil/adenoid infections and snoring with associated sleep apnea. Tonsil infections: As a general guideline, a tonsillectomy is recommended in patients with seven or more tonsil infections in one year, five infections a year for two years, or three infections for three or more years. Sleep apnea: Enlargement of tonsil and adenoid tissue in children can obstruct airways during sleep. Children with sleep apnea typically are mouth breathers who snore loudly and can be heard to stop breathing or make gasping noises during sleep. Sleep apnea results in fragmented sleep that can lead to daytime fatigue or hyperactivity, failure to thrive, difficulties in concentrating, and occasional problems with bedwetting. Surgical procedure: Tonsils and adenoids are removed through the mouth with no external scars. In most children, this is outpatient surgery. Back to top What causes my hoarseness? Hoarseness, due to irritation of the larynx, is commonly caused by upper respiratory infections, reflux of stomach acid, and/or postnasal drip. Upper respiratory infections: People frequently develop a persistent cough following a common cold. A cycle may develop in which episodic coughing results in throat irritation, which causes more coughing and more irritation. The larynx then becomes even more susceptible to other irritants such as acid reflux and posterior drainage from the nose. It is important to break the coughing cycle by maintaining adequate hydration, taking throat lozenges, and avoiding throat clearing. Gastrointestinal Reflux Disease (GERD): Acid from the stomach can reflux up through the esophagus to the larynx. The resulting acid exposure can cause a multitude of symptoms, including hoarseness, throat discomfort, swallowing problems and a feeling of a foreign body caught in the throat. Acid reflux may occur at night, so that sleeping patients do not notice symptoms of heartburn. Treatment of GERD includes antacids, elevating the head of the bed, changing the diet, and avoiding caffeine and alcohol. Postnasal drainage: Mucous drainage from the nose can cause throat irritation and hoarseness. Nasal steroid sprays and nonsedating antihistamines may help reduce the amount of drainage. Less common causes of hoarseness and voice change include decreased thyroid function, vocal cord paralysis, vocal cord nodules or polyps, and tumors of the larynx. Hoarseness lasting more than four-six weeks should be evaluated by a physician. Otolaryngologists can visualize the both mirrors and flexible fiberoptic telescopes. Back to top What can be done about my snoring? Snoring is a common problem that may occur alone or in combination with obstructive sleep apnea. Primary snoring: Snoring typically is caused by vibration of tissues within the oral pharynx (the uvula and palate). Nasal obstruction can be another cause. In mild snoring, these measures may help: losing weight, sleeping on your side rather than your back, avoiding sedatives and alcohol. Surgery can reduce the size of the soft tissue of uvula and palate, and also relieve nasal obstruction. The PAMF Department of Otolaryngology uses a carbon dioxide laser to remove excess uvular and palatal soft tissue, an office procedure using local anesthesia. Office turbinate surgery may also help snoring by improving nasal breathing. Obstructive Sleep Apnea: Obstructive apnea is a cessation of breathing that last ten seconds or more. Repeated episodes can significantly disrupt sleep. Manifestations of sleep apnea include snoring, restless sleep, and daytime fatigue. Many advances have been made in treatment of sleep apnea. http://quiz.md/ent/questions Please wait cardiology dermatology emergency medicine ENT gastroenterology general surgery gynecology infectious disease nephrology neurology obstetrics ophthalmology orthopedics pediatrics plastic surgery rheumatology urology Email Password Sign up Forgot my password Enter your email address Temporary login information will be sent to you. Email address Cancel Supporters Partners Questions tagged ENT 1 2 3 0 acclamations 0 comments 2 responses 100% correct responses Created on October 18 by Caroline Xu The tongue is derived from all of the following pharyngeal arches except: 1. V 100% 2. II 0% 3. I 0% 4. IV 0% 5. III 0% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 2 responses 50% correct responses Created on October 18 by Caroline Xu The first branch of the external carotid artery is: 1. internal maxillary artery 50% 2. superior thyroid artery 50% 3. transverse facial artery 0% 4. facial artery 0% 5. occipital artery 0% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 0 responses n/a correct responses Created on October 18 by Caroline Xu Which of the following is not a direct branch of the external carotid artery 1. superficial temporal artery 2. inferior thyroid artery 3. ascending pharyngeal artery 4. lingual artery 5. superior thyroid artery Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 3 responses 0% correct responses Created on October 18 by Caroline Xu The inferior thyroid artery is a branch of: 1. costocervical trunk 0% 2. vertebral artery 0% 3. common carotid artery 0% 4. subclavian artery 100% 5. thyrocervical trunk 0% Topics: ENT, general surgery Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 1 responses 100% correct responses Created on October 18 by Caroline Xu Which of the following arteries is the first branch of the subclavian artery 1. internal thoracic artery 0% 2. dorsal scapular artery 0% 3. costocervical trunk 0% 4. thyrocervical trunk 0% 5. vertebral artery 100% Topics: ENT, general surgery Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 2 comments 3 responses 66% correct responses Created on October 11 by Caroline Xu A mother brings her 6-yr old son into your office complaining of recurrent croup since the age of 2. There is no history of prior intubation for any of these episodes. Which of the following is not a possible explaination for the child's symptoms 1. laryngomalacia 66% 2. laryngopharyngeal reflux 0% 3. subglottic stenosis 0% 4. subglottic cyst 0% 5. subglottic hemangioma 33% Topics: ENT, pediatrics Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on January 24 by Kevin V. Plumley Laryngomalacia - Very Common. Typically not life-threatening obstruction resultant to infolding of the immature infantile or elderly cartilage of the larynx. Inspiratory stridor intensified while supine Surgery is only necessary with significant obstruction and or comorbidities (e.g. GERD) posted on January 24 by Kevin V. Plumley Laryngomalacia is the most common cause of congenital stridor. Laryngomalacia usually appears within the first several days to weeks after birth. It is characterized by high-pitched inspiratory stridor, alleviated by prone position, and a normal cry. It is a self-limited condition that rarely requires surgical management unless there is inability to feed orally, life-threatening airway obstruction, FTT or cor pulmonale. Vocal cord paralysis patients have a weak cry. Subglottic stenosis typically presents with a biphasic stridor and a hoarse cry. http://www.emedicine.com/ped/topic2624.htm 0 acclamations 0 comments 0 responses n/a correct responses Created on October 11 by Caroline Xu A 65-year old man comes to your office complaining of 3 month history of progressive hoarsness. He denies any dysphagia or dyspnea. He has a 35-pack year history of smoking and is on a PPI for GERD. Flexible laryngoscopy shows a small ulcerating nodular lesion on his left true vocal cord. In addition, there is some subtle fullness of the left false vocal fold. Your presumptive diagnosis and plan is: 1. laryngopharyngeal reflux - increase dose of PPI 2. glottic cancer - urgent referral to head and neck surgeon 3. vocal cord nodule - encourage voice rest 4. laryngeal papilloma - send for laser excision 5. benign vocal cord lipoma - reassurance Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 3 responses 66% correct responses Created on October 11 by Caroline Xu Which of the following is not a typical feature of allergic rhinitis? 1. Exacerbated by seasonal allergens (pollens, etc.) 0% 2. Type II allergy mediated by IgG and IgM 66% 3. Symptoms of clear rhinorrhea, congestion, postnasal drip, itching eyes 0% 4. Increases one's risk for acute and chronic rhinosinusitis 33% 5. On exam, turbinate congestion and bogginess and allergic shiners 0% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 2 responses 50% correct responses Created on October 11 by Caroline Xu A complication of deep neck space infection infection involving the danger space is: 1. mediastinitis 50% 2. discitis 0% 3. thrombophlebitis 0% 4. tracheitis 0% 5. cavernous sinus thrombosis 50% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 1 comment 2 responses 50% correct responses Created on October 11 by Caroline Xu A 65 yr-old lady comes into your office complaining of 6-month history of pulsatile tinnitus in her right ear and an associated progressive hearing loss. She is relatively healthy except for hypercholesterolemia and hypertension. On exam, a pulsatile redish-blue mass can be seen behind the right tympanic membrane. You are most concerned about: 1. cholesteatoma 0% 2. serous otitis media 0% 3. glomus tympanicum 50% 4. acoustic neuroma 50% 5. tympanic membrane perforation 0% Topics: ENT Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on January 24 by Kevin V. Plumley glomus jugulare tumor (or glomus body)-collection of highly vascular paraganglionic tissue, originating from the chief cells. Typically benign, rare, encapsulated, and slow-growing with a female predominance (~4:1, 5th & 6th decades). Locally invasive, commonly via temporal air cells, lumina, foramina etc. Some produce catecholamines and non-producers show a familial inheritance. Most common symptoms - conductive hearing loss and pulsatile tinnitus ---ear fullness, otorrhea, hemorrhage, bruit, middle ear mass. ---ear pain is uncommon ---inner ear involvement may present with vertigo and sensorineural hearing loss Possible CN 9-11 involvement Surgery is typical for symptomatic pts. 0 acclamations 0 comments 2 responses 100% correct responses Created on October 11 by Caroline Xu Which of the following anatomic factors does not usually contribute to pediatric sleep-disordered breathing? 1. mandibular hypoplasia 0% 2. adenotonsillar hypertrophy 0% 3. cleft plate or submucous cleft 0% 4. macroglossia 0% 5. eustachian tube dysfunction 100% Topics: ENT, pediatrics Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 1 responses 0% correct responses Created on October 11 by Caroline Xu Pediatric sleep-disordered breathing is a spectrum of disorders that includes all of the following except 1. obstructive sleep apnea syndrome 0% 2. obstructive hypopnea syndrome 0% 3. upper airway resistance syndrome 100% 4. primary snoring 0% 5. primary hypersomnia 0% Topics: ENT, pediatrics Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 1 comment 1 responses 0% correct responses Created on October 11 by Caroline Xu Which of the following is not a direct branch of the external carotid artery? 1. Superior thyroid artery 0% 2. Superficial temporal artery 0% 3. Submental artery 0% 4. Facial artery 100% 5. Ascending pharyngeal artery 0% Topics: ENT Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on January 24 by Kevin V. Plumley The submental artery is a branch of the facial 0 acclamations 0 comments 0 responses n/a correct responses Created on October 11 by Caroline Xu Which of the following is not a typical head and neck manifestation of Wegener's Granulomatosis 1. laryngomalacia 2. mucosal ulcerations 3. Septal perforation 4. Otitis media and conductive hearing loss 5. Chronic sinusistis Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 1 responses 100% correct responses Created on October 11 by Caroline Xu Which of the following is not a typical feature of allergic fungal sinusitis 1. asthma 0% 2. orbital invasion 100% 3. elevated serum IgE 0% 4. allergic rhinitis 0% 5. family or personal history of atopy 0% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 1 comment 15 responses 40% correct responses Created on August 16 by Gary Galante A 10 y/o child presents to you with a 3 year history of tinnitus, and unsteadiness and dizziness while walking, which has slowly progressed over the same period. No other symptoms were elicited on review of systems. Examination reveals the following: Rinne – Air Conduction > Bone Conduction bilaterally Weber – Right lateralization The remainder of the cranial nerve examination is unremarkable, including Romberg and Dix-Hallpike testing. You send the child for audiometry, which confirms unilateral sensorineural hearing loss. MRI with gadolinium contrast confirms the presence of an intracranial mass What is the most likely diagnosis, and what neurocutaneous syndrome should you inquire about on family history? 1. Left acoustic neuroma, Neurofibromatosis – 2 40% 2. Left acoustic neuroma, Tuberous Sclerosis 6% 3. Right meningioma, Tuberous Sclerosis 0% 4. Left meningioma, Neurofibromatosis – 1 13% 5. Right acoustic neuroma, Neurofibromatosis – 1 26% 6. Right acoustic neuroma, Neurofibromatosis -2 13% Topics: neurology, ENT Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on August 16 by Gary Galante The child presents with history and physical findings best in keeping with an acoustic neuroma. It is otherwise known as a vestibular schwannoma, arising from the vestibular portion of cranial nerve VIII. It is a slow growing tumor, and as it grows, it can compress/damage other cranial nerves in the cerebellopontine angle, e.g. CN V/VII, and eventually compress the brainstem and cerebellum. Presentation is based on cranial nerve involvement. Involvement of the cochlear component of CN VIII usually leads to complaints of tinnitus, and hearing loss. Because of the chronicity in development of hearing loss due to slow tumor growth, some people, especially children, may be unaware of this hearing loss. Involvement of the vestibular component leads to sensations of unsteadiness while walking, with severity that fluctuates over time and is generally progressive. An important thing to note here is that true central vertigo is uncommon, because slow-growing acoustic neuromas cause gradual asymmetry in vestibular function, and the central vestibular system often compensates for this gradual loss of input from one side. Rarely, CN V (facial numbness, hypesthesia, pain) and CN VII (facial paresis, taste disturbances) can be involved leading to symptoms of corresponding nerve dysfunction. These are usually late symptoms, however. On physical examination, hearing tests are typically abnormal. The Rinne and Weber tests should be used to characterize the location and type of hearing loss. As well, a full cranial nerve exam should be done although usually normal. Romberg and other common office balance tests are also typically normal. For the Rinne test – a 512 Hz tuning fork is struck, then held to the mastoid process and once the patient can no longer hear the sound, then placed near the ear. Normally (also if sensorineural hearing loss), the person should hear the sound after the fork is placed by the ear ie. Air conduction > Bone conduction. In the case of conductive hearing loss, the person will not hear the sound ie. BC > AC. For the Weber test – a 512 Hz tuning fork is struck, and placed on the patient’s midline forehead. If there is unilateral conductive hearing loss, the patient will lateralize (hear the sound loudest) to the affected ear’s side. If there is unilateral sensorineural hearing loss (SNHL), the patient will lateralize to the opposite side. In this example, the child has AC>BC and lateralizes to the right side, thus likely exhibits Left SNHL. Audiometry is the best initial screening laboratory test for the diagnosis of vestibular schwannoma; 5 percent of patients will have a normal test. Results typically show asymmetric sensorineural hearing loss. With a history, physical, and audiometry that suggest asymmetric SNHL, your working diagnosis should be “acoustic neuroma until proven otherwise.” The differential diagnosis includes (cerebellopontine angle) meningioma, which may present similarly, and accounts for 4-10% of such cases of unilateral SNHL, but is obviously lower on the DDx. So in this case, Left acoustic neuroma is the most likely diagnosis, and should be confirmed by MRI with gadolinium contrast. Acoustic neuromas are rare in children, except for those with Neurofibromatosis type 2. This is a rather obscure question of me to ask, as NF-2 is far less common than NF-1 with a prevalence of 1/50 000 (10% of all NF cases). Its diagnostic criteria are fulfillment of 1 or 2: (1) bilateral acoustic neuromas, or (2)(a)1st degree relative with NF-2 PLUS either (b) or (c) -(b)Unilateral acoustic neuroma, or (c)Any 2 of: meningioma, glioma, neurofibroma, schwannoma, or juvenile posterior subcapsular lenticular opacities. The classic skin findings seen in NF-1 are far less commonly seen in NF-2. Neurofibromatosis type 1, on the other hand, has many associations, but in terms of neurological neoplasms, the most common ones found i such patients are neurofibromas, and astrocytomas (especially optic gliomas). As Neurofibromatosis is an autosomal dominant disorder, and because in cases of unilateral acoustic neuromas, a family history in a 1st degree relative in necessary to make the diagnosis of NF-2, this question must be asked after the diagnosis is made, especially in children. It should be noted, however, that most cases of NF-2 are sporadic mutations, and thus a family history will not have any yield. 0 acclamations 1 comment 4 responses 25% correct responses Created on July 4 by Caroline Xu 45 yr old man develops severe pain and swelling in the submandibular region. He had a dental extraction 5 days ago. On exam, he also has trismus and stridor. Your diagnosis and management is: 1. Reactive lymphadenopathy - IV antibiotics 25% 2. Submandibular abscess - irrigation and drainage 25% 3. Bach's cellulitis - IV antibiotics 0% 4. Ludwig's angina - IV antibiotics and fluids 25% 5. Ludwig's angina - fiberoptic laryngoscopy +/- intubation 25% Topics: ENT Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on January 25 by Kevin V. Plumley Ludwig's angina is characterized as a rapidly progressive gangrenous cellulitis of the soft tissues of the neck and floor of the mouth.[52] With progressive swelling of the soft tissues and elevation and posterior displacement of the tongue, the most life-threatening complication of Ludwig's angina is airway obstruction. http://www.medscape.com/viewarticle/551650_4 0 acclamations 0 comments 5 responses 60% correct responses Created on July 4 by Caroline Xu A 65 yr old man complains of frontotemporal facial pain for the last 2 weeks and also jaw pain. He feels unwell and is worried about sinusitis. What do you need to rule out? 1. Temporal arteritis 60% 2. TMJ pathology 20% 3. Ocular myositis 0% 4. Rhinosinusitis 0% 5. Trigeminal neuralgia 20% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 5 responses 60% correct responses Created on July 4 by Caroline Xu Mr S is post-op day 1 from a middle ear surgery of your choice and is complaining of altered taste. Which nerve did the surgeon get a bit too close to? 1. Glossopharyngeal nerve 40% 2. Cochlear nerve 0% 3. Nerve to stapedius 0% 4. Lingual nerve 0% 5. Chorda tympani 60% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 0 responses n/a correct responses Created on July 4 by Caroline Xu Which of the following is not part of the strap (infrahyoid) muscles? 1. Sternothyroid 2. Thyrohyoid 3. Stylohyoid 4. Omohyoid 5. Sternohyoid 20 yr old male is complaining of globus and dysphonia. He drinks 3 - 6 beers every second night. Indirect laryngoscopy shows inflamed subglottic structures. Your impression and plans are: 1. Unilateral vocal cord paralysis - medialization laryngoplasty 0% 2. Globus hystericus - psych consult 50% 3. Laryngoesophageal reflux - start PPI 0% 4. Vocal cord nodules - voice hygiene 50% 5. Laryngeal malignancy - biopsy 0% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 4 responses 0% correct responses Created on July 4 by Caroline Xu What structure divides level IIa from level IIb nodes in the neck? 1. Stylohyoid muscle 25% 2. Posterior belly of digastric 50% 3. Spinal accesory nerve 0% 4. Glossopharyngeal nerve 25% 5. Omohyoid muscle 0% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 2 responses 100% correct responses Created on July 4 by Caroline Xu An elderly man complains of chronic otorrhea with otalgia and hearing loss. On exam, purulent foul-smelling discharge is present and a retracted tympanic membrane is present. You suspect chronic suppurative otitis media. What organisms should you worry about (the most)? 1. Mycobacterium tuberculosis 0% 2. Aspergillus 0% 3. Bacteroides and Peptostreptococcus 0% 4. Mycoplasma pneumoniae 0% 5. Pseudomonas and S. aureus 100% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 4 responses 25% correct responses Created on July 4 by Caroline Xu A 35 yr old woman complains of slow, progressive hearing loss that is bilateral. She denies vertigo but complains of occasional tinnitus. Her father also experienced a similar type of hearing loss at the age of 40. What is most likely in your differential? 1. Connexin 26 mutation 25% 2. Exostosis 0% 3. Otosclerosis 25% 4. Otitis media 0% 5. Meniere's 50% Topics: ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 1 comment 12 responses 16% correct responses Created on November 23 by Brandon Ball A patient comes to you complaining of decreased air entry to the nose, and difficulty breathing. Which part of the nose has the greatest impact on airway resistance? 1. Internal nasal valve 41% 2. Inferior turbinate 16% 3. Nasal septum 16% 4. External nasal valve 25% Topics: plastic surgery, Head and Neck, ENT Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on November 23 by Brandon Ball The inferior turbinate provides up to 2/3rds the total airway resistance. The internal nasal valve provides up to half of the total airway resistance. 0 acclamations 0 comments 10 responses 30% correct responses Created on November 23 by Brandon Ball A patient sees you complaining of decreased air entry to the nose, and difficulty breathing. You decide to perform nasal endoscopy, and upon looking in the nose, you ponder whether this patient has a narrowed internal nasal valve. What is the normal angle formed by the internal nasal valve? 1. 10-15 degrees 30% 2. 15-20 degrees 40% 3. 5-10 degrees 10% 4. 20-25 degrees 20% Topics: ENT, plastic surgery, Head and Neck Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 11 responses 9% correct responses Created on November 23 by Brandon Ball The dorsal nasal artery is a branch of which artery? 1. Opthalmic 9% 2. Lateral nasal 0% 3. Transverse facial 27% 4. Facial 63% Topics: Head and Neck, plastic surgery, ENT Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 1 comment 16 responses 43% correct responses Created on March 3 by Nawaaz Nathoo There are a number of parts to the lacrimal system. In what order does a tear encounter these, on its passage from the eye to the nose? 1. punctum -> cannaliculus -> naso-lacrimal duct -> naso-lacrimal sac -> nose 37% 2. punctum -> cannaliculus -> naso-lacrimal sac -> naso-lacrimal duct -> nose 43% 3. cannaliculus -> punctum -> naso-lacrimal sac -> naso-lacrimal duct -> nose 12% 4. punctum -> naso-lacrimal sac -> naso-lacrimal duct -> cannaliculus -> nose 6% Topics: ophthalmology, ENT, Anatomy & Eye Exam Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on September 23 by Nawaaz Nathoo Picture of the anatomy: http://c1-preview.prosites.com/31502/wy/images/DCR/Lacrimal%20diagram.jpg 0 acclamations 0 comments 30 responses 90% correct responses Created on March 3 by Nawaaz Nathoo Which cranial nerve is responsible for movement of the medial rectus, inferior rectus, superior rectus, and inferior oblique? 1. CN 7 0% 2. CN 6 0% 3. CN 4 10% 4. CN 3 90% Topics: ENT, neurology, ophthalmology, Anatomy & Eye Exam Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 30 responses 76% correct responses Created on March 3 by Nawaaz Nathoo Which cranial nerve is responsible for closure of the eyelids? 1. CN 7 76% 2. CN 4 3% 3. CN 6 0% 4. CN 3 20% Topics: ENT, ophthalmology, neurology, Anatomy & Eye Exam Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 0 comments 32 responses 75% correct responses Created on March 3 by Nawaaz Nathoo Which cranial nerve is responsible for opening of the eyelids? 1. CN 6 0% 2. CN 4 0% 3. CN 7 25% 4. CN 3 75% Topics: neurology, ENT, ophthalmology, ophthalmology, Anatomy & Eye Exam Acclaim this question | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question 0 acclamations 1 comment 20 responses 30% correct responses Created on November 5 by Daniel Kozan During a neck dissection you identify a large nerve coursing anteriorly between the internal jugular and internal carotid arteries. What nerve is this likely to be? 1. vagus nerve 55% 2. phrenic nerve 0% 3. spinal accessory nerve 15% 4. ansa cervacalis 0% 5. hypoglossal nerve 30% Topics: ENT, anatomy, plastic surgery Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on November 5 by Daniel Kozan The hypoglossal nerve supplies the muscles of the tongue (except the palatoglossus muscle which is supplied by the accessory nerve). 0 acclamations 1 comment 18 responses 50% correct responses Created on November 5 by Daniel Kozan Which of the following is not an effective way to identify the facial nerve within the parotid gland intraoperatively? 1. using the styloid and mastoid processes as landmarks 27% 2. tracing backwards from a branch 11% 3. following the retromandibular vein 11% 4. probing with a nerve stimulator 50% Topics: ENT, plastic surgery Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on November 5 by Daniel Kozan The facial nerve emerges from the stylomastoid foramen, so you may use the styloid and mastoid processes as landmarks. The facial nerve crosses over the retromandibular vein, so you may locate the nerve by following the vein. Tracing backwards from a branch works. Probing at random locations throughout the parotid with a nerve stimulator is not an effective way to locate the facial nerve. 0 acclamations 1 comment 21 responses 4% correct responses Created on November 5 by Daniel Kozan You are assisting in a neck dissection when your preceptor asks you to identify a nerve coursing superficially across the sternocleidomastoid. What nerve is this? 1. vagus nerve 23% 2. ansa cervacalis 23% 3. spinal accessory nerve 33% 4. phrenic nerve 14% 5. greater auricular nerve 4% Topics: ENT, plastic surgery Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on November 5 by Daniel Kozan Of the nerves listed the greater auricular nerve is the most superficial. It courses anterosuperiorly across the sternocleidomastoid. 0 acclamations 1 comment 57 responses 77% correct responses Created on July 23 by Lauren Kitney Which of the following is not a complication of acute otitis media? 1. all of the above are complications of acute otitis media 77% 2. tympanic membrane perforation 3% 3. brain abscess 8% 4. conductive hearing loss 7% 5. meningitis 3% 6. mastoiditis 0% Topics: ENT, infectious disease, pediatrics, general pediatrics Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on July 23 by Lauren Kitney All of the above are potential complications of acute otitis media 1 acclamation 1 comment 56 responses 73% correct responses Created on July 23 by Lauren Kitney Which of the following organisms does NOT commonly cause acute otitis media in otherwise healthy children? 1. Staphylococcus aureus 73% 2. Moraxella catarrhalis 8% 3. Haemophilus influenzae 7% 4. Streptococcus pneumoniae 10% Topics: infectious disease, ENT, pediatrics, general pediatrics Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on July 23 by Lauren Kitney S. pneumoniae, H. influenzae and M. catarrhalis are all common bacterial causes of acute otitis media. Acute otitis media can also be caused by viruses. S. aureus and P. aeruginosa are common causes of otitis externa. 1 acclamation 1 comment 141 responses 60% correct responses Created on February 14 by Daniel Kozan A 25-year old male presents with a greatly swollen left face around the orbit and his left eye appear lower than the right. Which bone is likely fractured? 1. ethmoid 14% 2. zygomatic 24% 3. maxilla 60% 4. frontal 0% Topics: neuroanatomy, ophthalmology, ENT, plastic surgery Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on March 14 by Madhav Sarda Doesn't both the maxilla and zygomatic bones make up the inferior wall of the orbit? (I thought this was an inferior wall blow-out fracture) 1 acclamation 2 comments 105 responses 91% correct responses Created on February 14 by Daniel Kozan Which of the following walls of the orbit is mismatched? 1. floor - maxilla and zygomatic 4% 2. roof - maxilla 91% 3. lateral wall - zygomatic 1% 4. medical wall - ethmoid 1% Topics: gross anatomy, ENT Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on March 14 by Jon H Is the medical wall the one in 6-28 we all lean on between lectures? posted on March 14 by Madhav Sarda Nah, it's the one that the surgeons spray graffiti on. 1 acclamation 4 comments 113 responses 68% correct responses Created on February 14 by Daniel Kozan Where is the most common location for an orbit fracture? 1. ethmoid bone 68% 2. maxilla 20% 3. zygomatic bone 8% 4. frontal bone 2% Topics: gross anatomy, ENT Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on March 13 by Daisy Hartmann According to our notes (and I looked it up online), though ethmoid fractures are most likely to occur in blunt trauma, the definition of a "blow out" fracture is when the orbital floor is fractured... posted on March 13 by Sheena Sikora That's what I thought too Daisy, although we were also taught that the ethmoid bone is the thinnest and weakest, so that might have been what Dan was testing. I'm not sure what the correct answer here would be. posted on March 14 by Daisy Hartmann Well, if the question was something like "what is the most common location for an orbit fracture" then ethmoid would be correct, but if you are asking specifically about a "blow out fracture", then I would think the question is testing whether we know that it has to do with orbital floor fractures, in which the maxilla would be the best answer... posted on March 14 by Daniel Kozan Thanks guys, I changed it as Daisy suggested. 0 acclamations 1 comment 98 responses 77% correct responses Created on April 14 by Peter Gill Which of the following is NOT an absolute indication for a tonsillectomy? 1. Malignancy 7% 2. Hemorrhagic tonsillitis 7% 3. Severe obstructive sleep apnea 8% 4. Cardiac valve abnormality 77% A mother brings in her 4-6 week old infant reporting a breathing abnormality over the past week. On observation, you note a high-pitched inspiratory stridor that is worse when supine and with crying. There is no indication of respiratory distress and the physical exam is unremarkable. The mother reports that there is no trouble with feeding and no known history of foreign body aspiration. What is the most likely diagnosis? 1. Subglottic stenosis 26% 2. Vocal cord paralysis 4% 3. Laryngomalacia 66% 4. Hemangiomas 1% Topics: pediatrics, pediatric ENT, ENT, respirology, general pediatrics Acclaim this question | View discussion Hide discussion | Post comment Post a comment An email notification will be sent to the author(s) of this question. Cancel This comment is private to the author of this question posted on April 14 by Peter Gill Laryngomalacia is the most common cause of congenital stridor. Laryngomalacia usually appears within the first several days to weeks after birth. It is characterized by high-pitched inspiratory stridor, alleviated by prone position, and a normal cry. It is a self-limited condition that rarely requires surgical management unless there is inability to feed orally, life-threatening airway obstruction, FTT or cor pulmonale. Vocal cord paralysis patients have a weak cry. Subglottic stenosis typically presents with a biphasic stridor and a hoarse cry. http://www.emedicine.com/ped/topic2624.htm http://www.emedicinehealth.com/script/main/alphaidx.asp?p=b_140 http://www.entnet.org/ http://www.nlm.nih.gov/medlineplus/earnoseandthroat.html http://www.pediatric-ent.com/ |
