|
Renal medical emergencies Nephrology (Kidney Disease) |
|
Nephrologist
Urinary system
Anatomy of the Urinary System
Human kidney anatomy, physiology, and biochemistry
|
What are the components of the human urinary system? Can you name the components of the human urinary system? 2 kidneys 2 ureters 1 urinary bladder 1 urethra 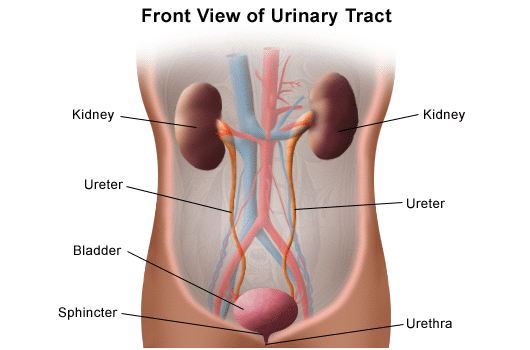 What are the components of the human kidney? Can you name the components of the human kidney? Renal capsule Renal cortex Renal medulla Renal pelvis Calyx: major calyx and minor calyx Nephron Medullary pyramids Ureter Renal arteries Renal veins 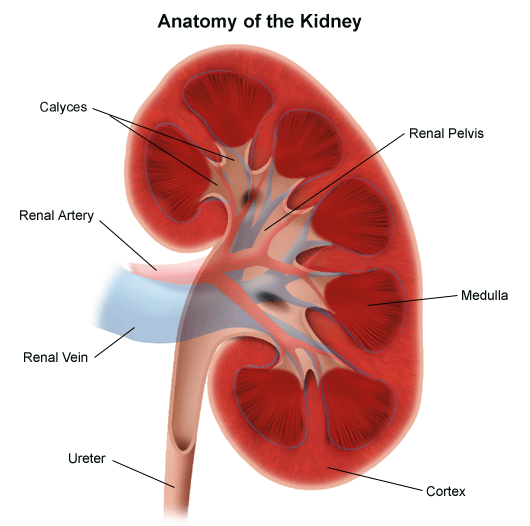 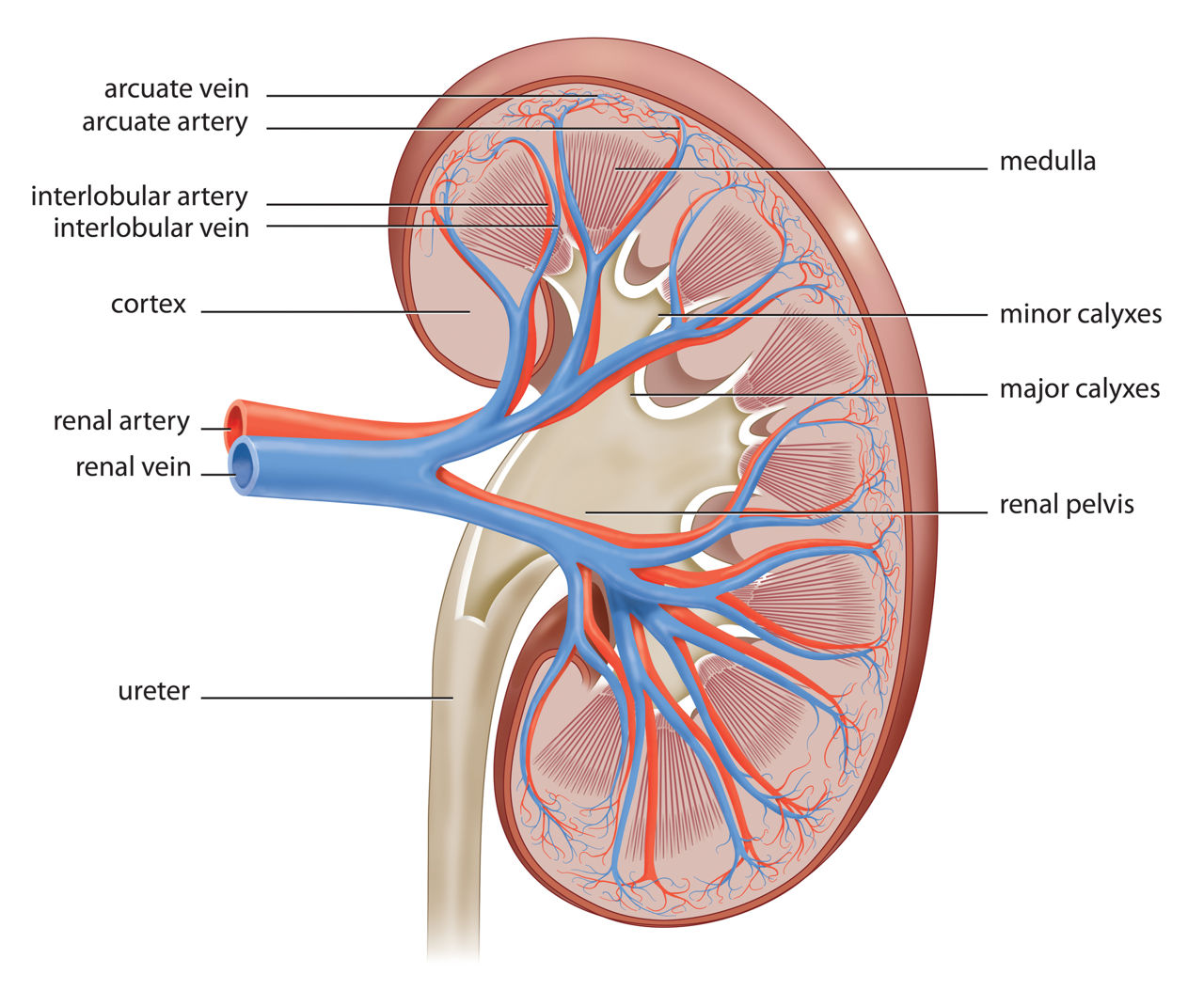 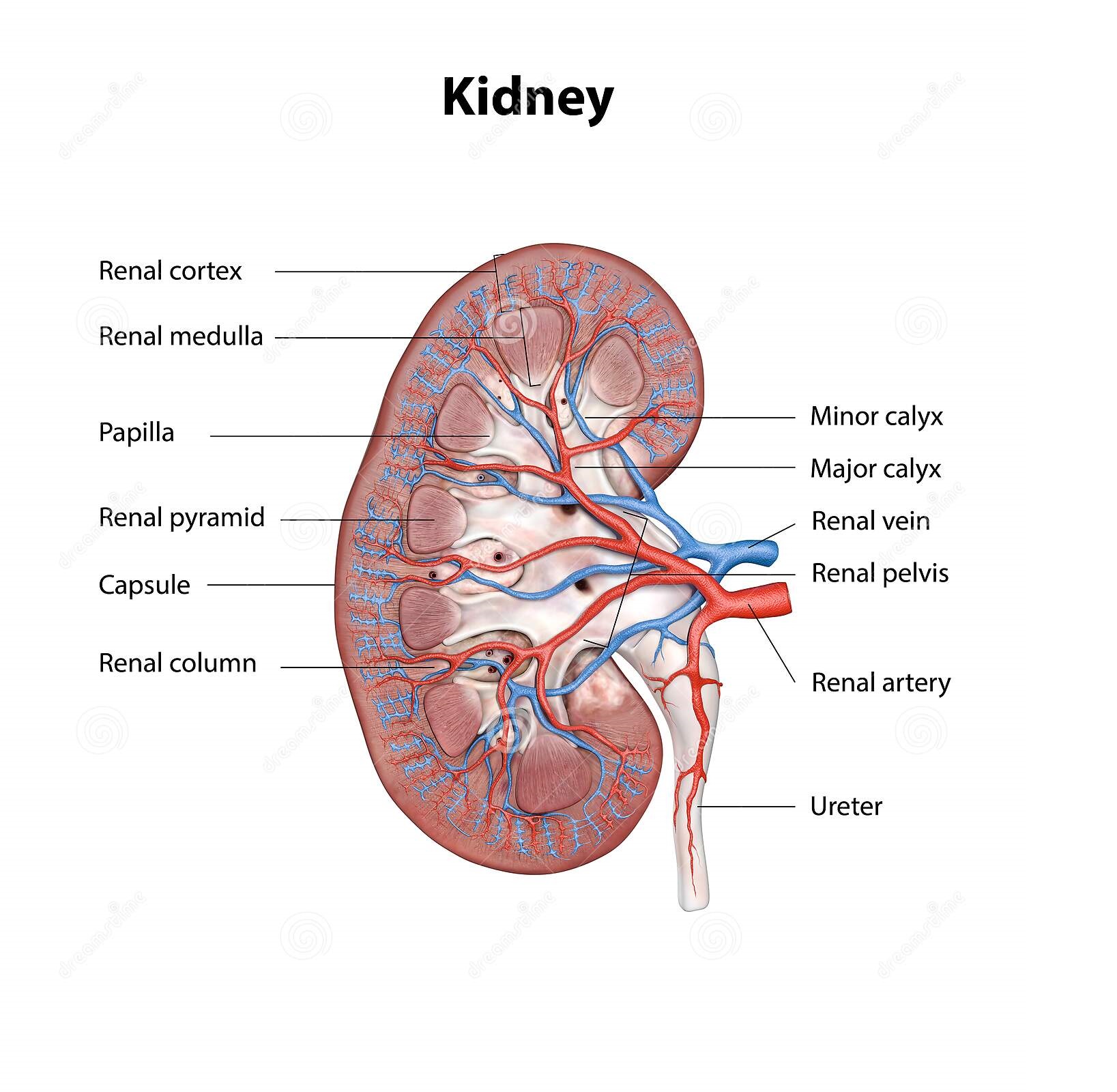
How does the urinary system work? The urinary system's function is to filter blood and create urine as a waste by-product. The organs of the urinary system include the kidneys, renal pelvis, ureters, bladder and urethra. Here are further guidelines. |
Urinary System Emergencies
Assessment and Evaluation of the Renal Patient
Evaluation of the Renal Patient
How should you do a quick assessment, diagnosis, and treatment of a person reported as a renal medical emergency?
|
Clinical Procedures for Safer Patient Care
Initial and Emergency Assessment First, analyze Glasgow Coma scale, then analyze vital signs including consciousness. When was the patient normal? ____________________________________ Can the patient open both eyes spontaneously? ____________________________________ Can the patient talk or make noise relevant to age? ____________________________________ Can the patient walk or move extremities relevant to age? ____________________________________ If yes, Glasgow Coma scale is 15. Glasgow Coma scale of 15 means the patient is not in a coma. vv The patient can have less serious medical issues. v Go ahead with vital signs, including consciousness. Level of consciousness Pulse rate: Respiratory rate: Blood pressure: Temperature: What is the oxygen saturation by pulse oximetry? A – Airway B – Breathing C – Circulation C – Consciousness S – Safety A – Airway Is the patient’s airway compromised? Does the patient’s position need to be changed? If patient is choking on thick secretions, consider oral suctioning (check suction equipment). B – Breathing •Assess rate and ease of breathing. •Assess the effectiveness of the oxygen delivery Oxygen supplementation Is the oxygen flow connection intact? Is the rate, flow, and percentage as ordered? Based on your assessment, consider the need for potential oxygen supplementation. C – Circulation •Assess for the presence of a radial pulse. •Assess skin colour, moisture, and temperature for signs of decreased tissue perfusion (pale, dusky, cool, or clammy skin). Note whether the pulse is too fast, too slow, or absent. If a radial pulse is not detectable, check for a carotid pulse. If no pulse is present, call for help and start CPR. C – Consciousness •Check the patient’s level of consciousness (LOC). Is the patient alert, drowsy, disoriented, restless, agitated, unconscious? Note if there is a change from the patient’s normal or previously noted LOC. S – Safety •Ensure the patient is safe and free from risk of harm or injury at all times. Check for name band and allergy band. Check oxygen saturation level. Check that suction is working. Check brakes on the bed, bedrail position (up, if required), bed is at the appropriate level, and call bell is within reach. Are there any fall risk indicators? |
|
Assessment of Non-emergency Case
History and Physical Examination 1. Person Profile 2. Chief Complaint 3. History of Present illness 4. Past Medical History 5. Social History: 6. Review of systems: 1. Person Profile Where is the patient now? ____________________________________ What seems to be the issue or issues? ____________________________________ What assessment type does the patient need at this point? ____________________________________ Name Age Date Height Weight Date of Birth Chief Complaint What is the main reason for your visit today? (Describe the problem in detail) What was your recent blood pressure? History of Present illness Please circle the appropriate response Do you get up at night to urine? ; Yes; No If yes how often Does your urine come out freely? ; Yes; No Do you have to strain to urine? ; Yes; No When you get the urge to urinate, can you hold it? ; Yes; No Do you have burning with urination? ; Yes; No Have you noticed blood in your urine? ; Yes; No Have you had a urinary tract infection? ; Yes; No Have you had a kidney stone? ; Yes; No Physician use only: (Comments/Notes) Past Medical History Please circle the appropriate response Take a look at this. Do you have or have ever had: Diabetes ; Yes; No If yes, do you take insulin? ; Yes; No High blood pressure ; Yes; No Heart problems ; Yes; No Any other medical problems ; Yes; No If yes, please list them all: List any surgeries you have had Are you on any medications? ; Yes; No If yes, please list all of them: Do you have any allergies to any medications? ; Yes; No If yes, please list v Do you take Aspirin or any other blood thinners? ; Yes; No Do you have a Family History of?(Example: MOTHER, FATHER, SISTER, BROTHER Etc) Diabetes ; Yes; No High blood pressure ; Yes; No Heart disease ; Yes; No Cancer; Yes; No If yes, in whom? Social History: Relationship status ; Yes; No Children ; Yes; No Do you currently smoke? ; Yes; No If yes, how much? Have you smoked in the past? ; Yes; No Stopped when? Do you drink alcohol? ; Yes; No If yes, how much? What type of work do you do? ; Yes; No If not currently working, what type of work did you do in the past? Review of systems: Do you now or have ever had any problems related to the following systems? Tick Yes or No General Vision Head and Neck (H&N) Pulmonary Cardiovascular (C/V) Gastrointestinal Genito-Urinary Hematology/Oncology Male / Female Ob/Gyn/Breast Neurological Endocrine Infectious Diseases Musculoskeletal Mental Health Skin and Hair Constitutional Symptoms Fever ; Yes; No Chills ; Yes; No Other Integumentary Skin rash ; Yes; No Peristent itch ; Yes; No Other Eyes Blurred vision ; Yes; No Double vision ; Yes; No Other Ear/Nose/Throat/Mouth Hearing lost ; Yes; No Sinus problems ; Yes; No Other Neurological Seizures ; Yes; No Strokes ; Yes; No Other Endocrine Excessive thirst ; Yes; No Too hot/cold ; Yes; No Other Cardiovascular Chest pain ; Yes; No Palpitations ; Yes; No Varicose veins ; Yes; No Other Respiratory Shortness of breath ; Yes; No Wheezing ; Yes; No Frequent cough ; Yes; No Other Gastrointestinal Constipation ; Yes; No Diarrhea ; Yes; No Ulcer/reflux disease ; Yes; No Other Hematologic Easy bruising ; Yes; No Blood clotting problems ; Yes; No Physician use only Post Void residual : Catheter Ultrasound Radiologic studies : Impression: Plan The evaluation of the patient with kidney disease begins with a thorough history and physical examination. The clinician should identify early on whether the renal disease is an acute or chronic condition. If previous medical records are available for the patient, this can be determined by quickly reviewing prior laboratory testing, with particular attention given to serum creatinine, blood urea nitrogen, and urinalyses. Patients who present on admission with AKI should be questioned about recent symptoms (eg, vomiting, diarrhea, edema, difficulty voiding, decreased appetite, weight changes) and events (eg, changes in oral intake, new medications, history of nonsteroidal anti-inflammatory drug [NSAID] use, administration of intravenous contrast, recent colonoscopy) that may help narrow the differential diagnosis of AKI. The presence of symptoms such as fever, rashes, arthralgias, epistaxis, and hemoptysis may be suggestive of an underlying systemic disease process such as vasculitis or other inflammatory conditions. For patients who develop AKI during their hospitalization, a thorough review of the most recent hospital eventsâ€â€Âincluding episodes of hypotension, recent diagnostic and therapeutic procedures, and initiation of new medicationsâ€â€Âshould be performed. All patients presenting with acute or CKD should be questioned about symptoms associated with uremia, including fatigue, nausea, vomiting, pruritus, metallic taste, lethargy, and confusion, since the presence of these symptoms may indicate the need for dialysis. A past medical history should be elicited to identify a prior history of kidney disease or other systemic diseases that could be relevant to the current presentation. In patients with CKD, who may or may not be presenting with an acute kidney-related problem, the clinician should establish the underlying cause, chronicity, and severity of the kidney disease. If the patient has end-stage renal disease (ESRD), information about the patient's nephrologist, outpatient dialysis unit, and regular consultation. |
Genitourinary emergencies.
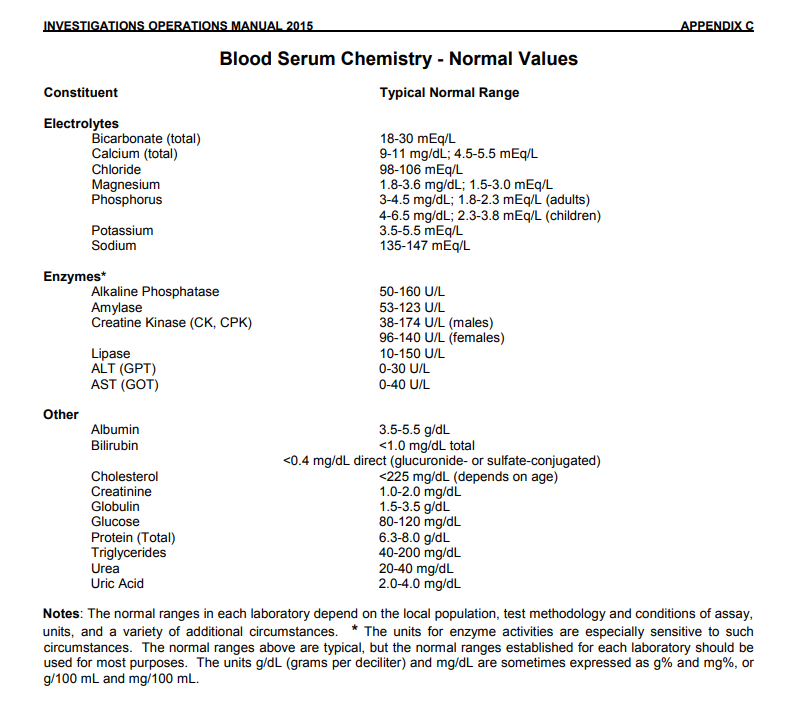
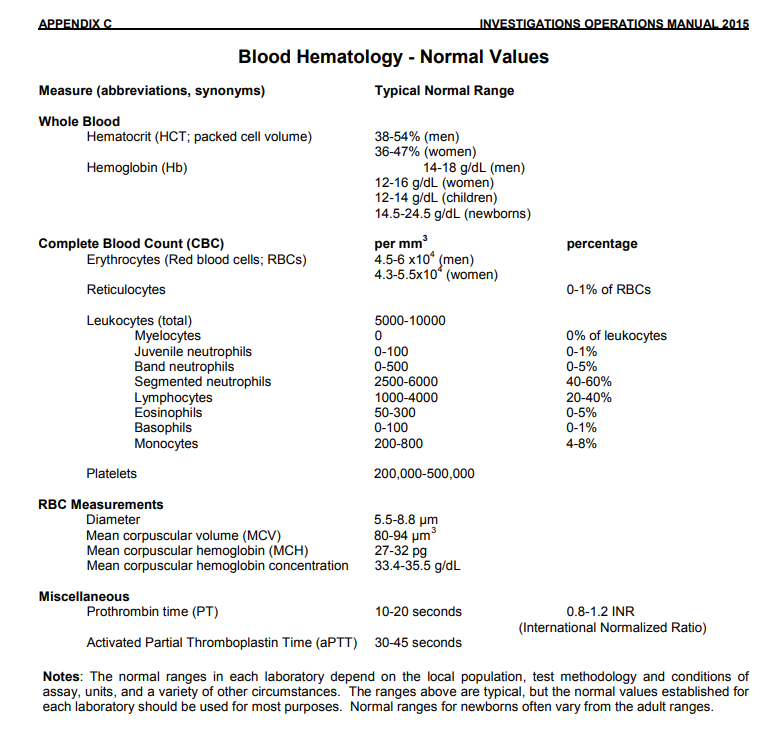
| Laboratory Tests |
Debate questions for existing medical doctors (MDs)
Acute Kidney Injury (AKI) / Acute Kidney Failure
|
What advice does Doctor Asif Qureshi provide for specific physicians diagnosing and treating such issues? 1. Do not make a diagnosis of acute renal failure if prerenal azotemia or similar causes exist. Fix the underlying cause. 2. Take these factors into consideration before diagnosing and treating chronic kidney disease (CKD): A. Symptoms B. Signs C. Urea, creatinine, and hemoglobin values (compared with FDA normal values). If these values are normal compared to FDA normal values, do not make a CKD diagnosis. D. In some regions, the computerized glomerular filtration rate or eGFR is wrong due to incorrect comparison values. First check for normal urea, creatinine, and hemoglobin values according to the FDA. Correlate the patient’s urea and creatinine values with the hemoglobin value and relevant symptoms. What is azotemia? Azotemia is an elevation of blood urea nitrogen (BUN) and serum creatinine levels. Prerenal Prerenal azotemia occurs when fluid isn’t flowing enough through the kidneys. This low flow of fluid creates high-level concentrations of serum creatinine and urea. This type of azotemia is the most common and can usually be reversed. Types There are three types of azotemia: prerenal intrinsic postrenal Intrinsic Intrinsic azotemia usually occurs from infection, sepsis, or disease. The most common cause of intrinsic azotemia is acute tubular necrosis. Postrenal A urinary tract obstruction causes postrenal azotemia. Postrenal azotemia can also occur with prerenal azotemia. These types of azotemia may have somewhat different treatments, causes, and outcomes. However, they each can lead to acute kidney injury and failure if it’s left untreated or if it’s not discovered early. What is the pathophysiology of prerenal azotemia? Prerenal azotemia refers to elevations in BUN and creatinine levels resulting from problems in the systemic circulation that decrease flow to the kidneys. The decreased renal flow stimulates salt and water retention to restore volume and pressure. When blood volume or pressure is decreased, the baroreceptor reflexes located in the aortic arch and carotid sinuses are activated. This leads to sympathetic nerve activation, resulting in renal afferent arteriolar vasoconstriction and renin secretion through ß1 receptors. Constriction of the afferent arterioles causes a decrease in intraglomerular pressure, which reduces the GFR proportionally. Reduction in renal blood flow results in the generation of renin, which converts angiotensinogen to angiotensin I. Angiotensin-converting enzyme then converts angiotensin I to angiotensin II, which, in turn, stimulates aldosterone release. The increase in aldosterone levels results in salt and water absorption in the distal collecting tubule. A decrease in volume or pressure is a nonosmotic stimulus for hypothalamic production of antidiuretic hormone, which exerts its effect in the medullary collecting duct for water reabsorption. Through unknown mechanisms, activation of the sympathetic nervous system leads to enhanced proximal tubular reabsorption of salt and water, as well as BUN, creatinine, calcium, uric acid, and bicarbonate. The net result of these 4 mechanisms of salt and water retention is decreased output and decreased urinary excretion of sodium (< 20 mEq/L). What is the pathophysiology of intrarenal azotemia? Intrarenal azotemia, also known as acute kidney injury (AKI), renal-renal azotemia, and (in the past) acute renal failure (ARF), refers to elevations in BUN and creatinine resulting from problems in the kidney itself. There are several definitions, including a rise in serum creatinine levels of about 30% from baseline or a sudden decline in output below 500 mL/day. If output is preserved, AKI is nonoliguric; if output falls below 500 mL/day, AKI is oliguric. Any form of AKI may be so severe that it virtually stops formation; this condition is called anuria (< 100 mL/day). The most common causes of nonoliguric AKI are acute tubular necrosis (ATN), aminoglycoside nephrotoxicity, lithium toxicity, and cisplatin nephrotoxicity. Tubular damage is less severe than it is in oliguric AKI. Normal output in nonoliguric AKI does not reflect a normal GFR. Patients may still make 1440 mL/day of urine even when the GFR falls to about 1 mL/min because of decreased tubular reabsorption. Some studies indicate that nonoliguric forms of AKI are associated with less morbidity and mortality than is oliguric AKI. Uncontrolled studies also suggest that volume expansion, potent diuretic agents, and renal vasodilators can convert oliguric AKI to nonoliguric AKI if administered early. The pathophysiology of acute oliguric or nonoliguric AKI depends on the anatomic location of the injury. In ATN, epithelial damage leads to functional decline in the ability of the tubules to reabsorb salt, water, and other electrolytes. Excretion of acid and potassium is also impaired. In more severe ATN, the tubular lumen is filled with epithelial casts, causing intraluminal obstruction and resulting in a declining GFR. What is acute kidney injury (AKI)? Acute kidney injury (AKI)â€â€Âor acute renal failure (ARF), as it was previously termedâ€â€Âis defined as an abrupt or rapid decline in renal filtration function. This condition is usually marked by a rise in serum creatinine concentration or by azotemia (a rise in blood urea nitrogen [BUN] concentration). However, immediately after a kidney injury, BUN or creatinine levels may be normal, and the only sign of a kidney injury may be decreased urine production. (See History.) A rise in the creatinine level can result from medications (eg, cimetidine, trimethoprim) that inhibit the kidney’s tubular secretion, while a rise in the BUN level can also occur without renal injury, resulting instead from such sources as gastrointestinal (GI) or mucosal bleeding, steroid use, or protein loading. Therefore, a careful inventory must be taken before concluding that a kidney injury is present How is acute kidney injury (AKI) defined? Acute kidney injury (AKI) is defined as an abrupt or rapid decline in renal filtration function. When should treatment of kidney injury (AKI) be initiated? Measures to correct underlying causes of acute kidney injury (AKI) should begin at the earliest indication of renal dysfunction. |
What are the different types of kidney diseases?
Components of the Urinary System
Chronic kidney disease (CKD)
End Stage Renal Disease (ESRD)
|
|
What is anemia? When you have too few red blood cells in your bloodstream, less oxygen is being delivered to your heart, muscles, brain and other organs in your body. This makes you anemic with less energy and more fatigue. Anemia is commonly associated with reduced kidney function. What is uremia? Uremia (uremic syndrome) is a serious complication of both acute kidney injury and chronic kidney disease. It occurs when urea and other waste products buildup in the body because the kidneys are not able to eliminate them. These substances can become poisonous (toxic) to the body if they reach high levels. Prolonged or severe fluid buildup may make the uremic syndrome worse and can cause: •Nausea, vomiting and weight loss •Changes in mental status, such as confusion, reduced awareness, agitation, psychosis, seizures and coma •Abnormal bleeding, such as bleeding spontaneously or profusely from a very minor injury •Heart problems, such as an irregular heartbeat, inflammation in the sac that surrounds the heart (pericarditis), and increased pressure on the heart •Shortness of breath from fluid buildup •Kidney dialysis is usually needed to relieve the symptoms of uremic syndrome until normal kidney function can be restored. |
Prevention of problems and diseases of related to nephrology
|
What can you do to keep your kidneys healthy? What can you do to prevent kidney disease? 1. Manage your blood pressure High blood pressure can increase your risk for heart disease as well as kidney failure. 2. Manage your blood sugar Diabetes increases your risk for heart disease and kidney failure. That’s just one reason to manage your blood sugar. 3. Maintain a healthy weight Obesity can increase your risk for conditions associated with kidney failure, such as diabetes and high blood pressure. 4. Eat a heart-healthy diet A heart-healthy diet  one low in sugar and cholesterol and high in fiber, whole grains, and fruits and vegetables  helps prevent weight gain. 5. Reduce salt intake Eating too much salt is associated with high blood pressure. 6. Drink enough water Dehydration reduces blood flow to your kidneys, which can damage them. 7. Limit alcohol Alcohol increases your blood pressure. The extra calories in it can make you gain weight, too. 8. Don’t smoke Smoking reduces blood flow to your kidneys. It damages kidney function in people with or without kidney disease. 9. Limit over-the-counter pain medication In high doses, nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen, reduce the amount of blood flow to your kidneys, which can harm them. 10. Reduce stress Reducing stress and anxiety can lower your blood pressure, which is good for your kidneys. 11. Exercise regularly Exercise, such as swimming, walking, and running, can help reduce stress, manage diabetes and high blood pressure, and maintain a healthy weight. |
Acid Base Balance in the Human Body
Acid-base and potassium disorders
|
How should you answer these questions? This depends on the type of question. Answer should be a number, one word, or a list of words or terms. Answers like this have accuracy. After a number, one word or a list of words or terms, you can elaborate further. Here are various examples. What is the average pH in human blood? 7.4 What is the pH ranges of human blood? 7.35 to 7.45. What are examples of various human acid-based disorders? Metabolic acidosis Metabolic alkalosis Respiratory acidosis Respiratory alkalosis Mixed acid-based disorders What is Measured in an ABG? There are six key components to an ABG. They include, pH - This measures the balance of acids and bases in your blood. Partial pressure of oxygen (PaO2) - This measures the pressure of oxygen dissolved in your blood. Partial pressure of carbon dioxide (PaCO2) - This measures the amount of carbon dioxide in your blood and how well carbon dioxide can move out of your body. Bicarbonate (HCO3) - This is calculated using the measured values of pH and PaCO2 to determine the amount of the basic compound made from carbon dioxide (CO2.) Oxygen saturation (O2 Sat) - This measures how much hemoglobin in your blood is carrying oxygen. Oxygen content (O2CT) - This measures the amount of oxygen in your blood. Hemoglobin - This measures the amount of hemoglobin in your blood. The aforementioned components all have different normal values and represent different aspects of the blood gas. According to the National Institute of Health, typical normal values are: pH: 7.35-7.45 Partial pressure of oxygen (PaO2): 75 to 100 mmHg Partial pressure of carbon dioxide (PaCO2): 35-45 mmHg Bicarbonate (HCO3): 22-26 mEq/L Oxygen saturation (O2 Sat): 94-100% In detail, arterial blood sampling allows to measure: the pH of the blood; partial pressure of arterial oxygen; the partial pressure of carbon dioxide; oxygen saturation; blood levels of bicarbonate (HCO3). How do you interpret arterial blood gases? Rules for rapid clinical interpretation of ABG Look at pH – < 7.40 – Acidosis; > 7.40 – Alkalosis. If pH indicates acidosis, then look at paCO2and HCO3- If paCO2is ↑, then it is primary respiratory acidosis. If paCO2↓ and HCO3- is also ↓→ primary metabolic acidosis. If HCO3-is ↓, then AG should be examined. What are the recommended steps in evaluating ABG values? Analysis and interpretation of basic ABG values can be determined by the following steps. Examine the pH level. If pH falls below normal (less than 7.35) the patient is acidotic; if it rises above normal (more than 7.45) the patient is alkalotic. Examine the PaCO2 level. Examine the HCO3 and PaO2 levels. > Why is an ABG Done? ABGs are drawn for a variety of reasons. These may include concerns for: Lung Failure Acute respiratory distress syndrome (ARDS) Sepsis Diabetic ketoacidosis (DKA) Cystic fibrosis Pneumonia Emphysema Hypovolemic shock Acute heart failure Cardiac arrest Renal tubular acidosis (RTA) Kidney Failure Septic Shock Trauma Chronic vomiting Uncontrolled diabetes Asthma Chronic Obstructive Pulmonary Disease (COPD) Hemorrhage Drug Overdose Metabolic Disease Chemical Poisoning To check if lung condition treatments are working |
Human kidney transplant: Guidelines from Doctor Asif Qureshi
Doctor Asif Qureshi et al.'s kidney transplant research team
|
Kidney transplant research team: Who will be on the list of Doctor Asif Qureshi et al.’s kidney transplant research team? You must be able to communicate in English Language. You must have experience of specific physician. On or before October 29, 2020 in America techniques of renal transplant are entirely different than those in Asia research has revealed circulates Doctor Asif Qureshi. On or before October 29, 2020 Africa, Australia and Latin resources are not displaying their advances in renal transplant at least on or before October 29, 2020. Why was there need to mention kidney transplant research team compared to Kidney transplant team or center? On or before October 29, 2020 in the last 50 years various different techniques have be practised. Some have very good outcome for the patient. Due to various new techniques in kidney transplant we need to go on researching until best solutions for the patient is there so that life of patient is prolonged with enhanced well being. |
|
What is on the list of pharmacology relevant to nephrology? What medicines are required in this situation? 1. Antihypertensive medications 2. Urinary tract stone medications 3. Medicine to treat high levels of phosphate in patients with chronic renal failure 4. Drug class: dialysis solutions 5. Other medications Antihypertensive medications: What are various examples? Diuretics (water pills) hydrochlorothiazide ACE inhibitors Beta blockers Potassium binders Hydrochlorothiazide (Oral Route) What is the first choice of medicine for hypertension in adults in this situation? Hydrochlorothiazide (oral route) 12.5 mg. Take one tablet by mouth one time daily. What is hydrochlorothiazide? Hydrochlorothiazide is a thiazide diuretic (water pill) that helps prevent your body from absorbing too much salt, which can cause fluid retention. Hydrochlorothiazide is used to treat high blood pressure (hypertension). Hydrochlorothiazide is also used to treat fluid retention (edema) in people with congestive heart failure, cirrhosis of the liver, or kidney disorders, or edema caused by taking steroids or estrogen. What is the maximum oral dose of hydrochlorothiazide per day? The dose is usually not more than 50 mg per day. What are examples of diuretics? Aldactone (spironolactone) Bumex (bumetanide) Demadex (torsemide) Esidrix (hydrochlorothiazide) Lasix (furosemide) Zaroxolyn (metolazone) What must manufacturers know about the requirements of 12.5 mg of hydrochlorothiazide (oral route) in America? On or after April 16, 2022, at least 37 million Americans had chronic kidney disease with hypertension. At least as many will require 12.5 mg of hydrochlorothiazide (oral route) every day in the future in America. Hydrochlorothiazide: What must a specific physician know? Description and brand names Before using Proper use Precautions Side effects What are some US brand name for hydrochlorothiazide? Aquazide H Hydrocot Microzide Zide In what format is this medicine dosage available? Capsule Tablet What are the functions of the human kidney? 1. Removal of urea, creatinine, and other metabolites 2. Hemoglobin or blood formation 3. Acid-base balance 4. Drug metabolism How do you maintain your kidney functions? An excess of anything is bad or harmful. 1. Intake of salt, sugar, and similar consumable items in required quantities 2. Blood pressure control 3. For diabetics, blood sugar control 4. Water intake according to requirements 5. Avoid over-the-counter medications 6. Drink tea, coffee, and similar beverages in the required quantities Do not diagnose chronic kidney disease (CKD) without publicly deliberating on the issues. What food is good for human kidneys? Fish Kale Spinach Sweet Potatoes Specific vitamins that are good for kidneys Here are further guidelines. |