| Admissions | Ambassadors | Accreditation | A to Z Degree Fields | Books | Catalog | Colleges | Contact Us | Continents/States | Construction | Contracts | Distance Education | Emergency | Emergency Medicine | Examinations | English Editing Service | Forms | Faculty | Governor | Grants | Hostels | Honorary Doctorate degree | Human Services | Human Resources | Internet | Investment | Instructors | Internship | Login | Lecture | Librarians | Languages | Manufacturing | Membership | Observers | Publication | Professional Examinations | Programs | Professions | Progress Report | Recommendations | Ration food and supplies | Research Grants | Researchers | Students login | School | Search | Software | Seminar | Study Center/Centre | Sponsorship | Tutoring | Thesis | Universities | Work counseling |
|
Coma is an emergency medical condition. If you are with a person who develops signs and symptoms of coma, call 911 or your local emergency number immediately. When you arrive at the hospital, emergency room staff will urgently need as much information as possible about what happened before the coma. On the way to the hospital, try to pull together answers to the following questions: Did the coma start abruptly or gradually? Were there problems with vision, dizziness or numbness beforehand? Does the affected person have any history of diabetes, seizures or strokes? Did you notice any changes in the person's health in the time leading up to the coma, such as a fever or worsening headache? Did you notice any changes in the person's ability to function in the time leading up to the coma, such as frequent falls or confusion? What prescription or nonprescription drugs did the affected person use? What is the Glasgow Coma Scale? The Glasgow Coma Scale was developed to provide health-caregivers a simple way of measuring the depth of coma based upon observations of eye opening, speech, and movement. Patients in the deepest level of coma: * do not respond with any body movement to pain, * do not have any speech, and * do not open their eyes. Those in lighter comas may offer some response, to the point they may even seem wake, yet meet the criteria of coma because they do not respond to their environment. The scale is used as part of the initial evaluation of a patient, but does not assist in making the diagnosis as to the cause of coma. Since it "scores" the level of coma, the Glasgow Coma Scale can be used as a standard method for any health-caregiver to assess change in patient status. The best use of the Glasgow Coma Scale is to allow caregivers of different clinical skills and training to consistently assess a patient over longer periods of time in order to determine whether the patient is improving, deteriorating, or remaining the same. In the initial care of a comatose patient, there may be first responders, EMTs, paramedics, emergency physicians, neurologists, neurosurgeons, and nurses evaluating the patient. The Glasgow Coma Scale allows a standard assessment that can be shared. Glasgow Coma Scale Eye Opening Spontaneous 4 To loud voice 3 To pain 2 None 1 Verbal Response Oriented 5 Confused, Disoriented 4 Inappropriate words 3 Incomprehensible words 2 None 1 Motor Response Obeys commands 6 Localizes pain 5 Withdraws from pain 4 Abnormal flexion posturing 3 Extensor posturing 2 None 1 A fully awake patient has a Glasgow Coma Score of 15. A person who has deceased has a Glasgow Coma Scale of 3 (there is no lower score). What are the causes of Coma? Generally, coma is commonly a result of trauma, bleeding and/or swelling affecting the brain. Inadequate oxygen or blood sugar (glucose) and various poisons can also directly injure the brain to cause coma. Brain inflammation and infection are also causes of altered mental status and coma. To understand unconsciousness, it is important to understand why a person is awake. The brain is a large organ with many parts. There are two main portions when separated down the middle (right and left cerebral hemispheres) containing the frontal, parietal, temporal and occipital lobes where movement, sensation, speech and thought are processed. The cerebellum sits under the cerebral hemispheres and is where balance and coordination are processed. The brain stem processes automatic, unconscious controls of the body including heart rate, blood pressure, and breathing. The reticular activating system (RAS) is located within the brain stem, and is the important "on/off" switch consciousness and sleep. * To be awake, the reticular activating system (RAS) must be functioning, as well as at least one cerebral hemisphere. * If a person loses consciousness, either the RAS has stopped working, or both cerebral hemispheres have shut down. The reticular activating system stops working in two situations: 1. Brain stem stroke: cells in that area of the brain stem have lost their blood supply, oxygen, and glucose that it delivers. This shuts off the reticular activating system. This event is either ischemic (blood supply is lost), or hemorrhagic (bleeding occurs and damages the reticular activating system). 2. A pre-death event: increased swelling in the brain pushes down on the brain stem and causes it to fail. For both cerebral hemispheres to fail at once, there must be loss of function of the whole brain. This is often due to lack of blood flow, for example when there is a rhythm disturbance of the heart such as ventricular fibrillation or if the heart stops beating. Also, severely decreased levels of oxygen in the blood due to lung failure can cause brain damage. Poisoning or inflammation of the brain can cause coma with loss of function from both cerebral hemispheres. Trauma Minor head injuries can cause brief loss of consciousness, but the brain is able to turn itself back on. Similarly, patients with seizures become unconscious - but gradually waken relatively quickly as the brain recovers from the seizure's "electrical storm." Those people who cannot respond after head injury usually have had significant force applied to their head and brain. The skull is a rigid box that protects the brain. Unfortunately, if the brain is injured and begins to swell (edema), there is no room for the additional fluid. Increased pressure within the brain (increased intracranial pressure) causes compression of the brain tissue against the skull bones. This swelling within the skull can cross the midline of the brain, and affect the undamaged hemisphere. If the intracranial pressure continues to increase without being treated, the brain will continue to swell until it pushes down through the opening at base of the skull, damaging the brain stem where the reticular activating system is located. This affects the ability of the brain to stimulate breathing and control blood pressure. The effect of trauma on the brain is not predictable. It may or may not cause significant injury. If the brain is shaken, shear injury may occur, whereby the nerve connections within the brain are damaged. Coma may occur even with a normal CT scan in this situation. Similarly, head trauma may cause swelling of the brain without any bleeding, and coma may be the result. Head trauma can cause different types of brain injury. The injury can occur to the brain tissue itself or may cause bleeding to occur between the brain and the skull. Computerized Tomography (CT) of the head can identify most bleeding from trauma. Bleeding (Hemorrhage) Bleeding within the brain (intracerebral hemorrhage) may be small, but can be associated swelling that may cause damage to the brain and result in coma. Epidural, subdural, and subarachnoid hemorrhages The lining of the brain has multiple layers, and these layers can act as potential spaces where bleeding can occur. Bleeding on the outside of the brain and under the brain lining, and subdural bleeding may not cause coma immediately, but as the bleeding continues, it compresses the injured side of the brain and shifts it to the unaffected side. Now both cerebral hemispheres are affected and loss of consciousness or coma may occur; the more swelling, the deeper the coma. Subarachnoid hemorrhage (bleeding beneath the arachnoid layer) occurs in the layer of the brain lining where cerebrospinal fluid (CSF) is located. CSF is the nutrient fluid that bathes the brain and spinal cord. Bleeding here may be without symptoms or it may cause significant problems, such as paralysis. Bleeding is often associated with a significant headache and neck stiffness. Bleeding can occur within the skull or brain without trauma. Some medical causes include: * Hypertension (high blood pressure): when blood pressure is too high, and not controlled, blood vessels in the brain may not be able to tolerate the high pressure and may leak blood. * Cerebral aneurysm, or an area in a blood vessel that is congenitally weak and ruptures. Some people are born with blood vessels that have a weak wall that can gradually balloon, like a weak spot in an inner tube. At some time in their life, or perhaps never, the weak spot gives way and blood is spilled into the brain. * Arteriovenous malformations (AVMs) are abnormal blood vessels where arteries connect to veins and cause potential weak spots that can leak blood. Normally, arteries branch into smaller and smaller vessels until they form the smallest set of vessels called capillaries. Capillaries form meshes where chemicals, nutrients, oxygen and carbon dioxide are exchanged from the blood stream to individual cells. The capillaries then merge to form larger blood vessels, the veins. In AVMs, this relationship of artery to capillary to vein is abnormal and is at risk for bleeding. * Tumors, either benign or malignant, can be very vascular (composed of many veins and capillaries) and have significant bleeding potential. 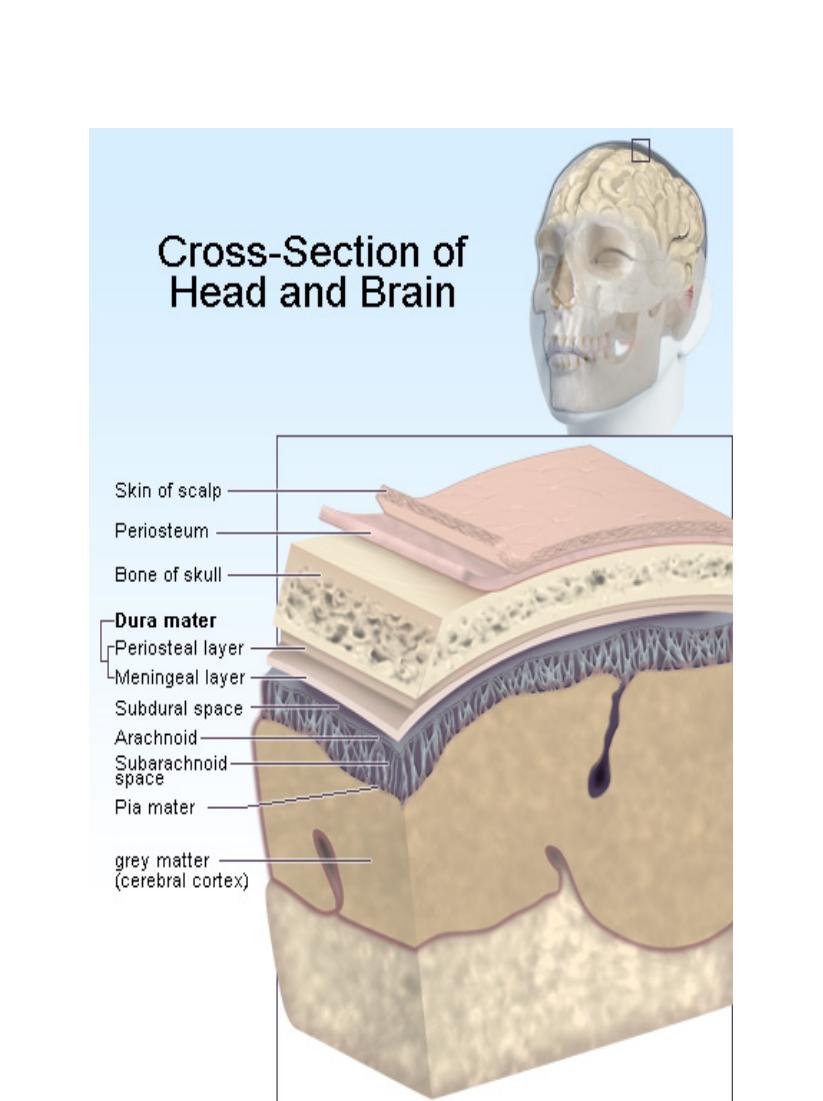
Tumors Just as blood takes up space within the skull and can cause coma, so may brain tumors. Brain tumors may be associated with localized swelling edema, inflammation and bleeding. Seizures, stroke-like symptoms, decreased mental status, and change in behavior may be the initial symptom. Swelling While trauma can make the brain swell, other types of injury or insult can cause brain swelling (cerebral edema). Whether the insult is lack of oxygen, abnormal electrolytes, or hormones, it may ultimately result in edema of the brain tissue. As with bleeding, the skull limits the space available for brain swelling to occur. As a result, the brain tissue is damaged and its function decreases the more it is compressed against the bones of the skull. Infection Infection and inflammation, such as encephalitis and meningitis of the brain and surrounding tissues may be associated with coma. Encephalitis is an infection of the brain tissue itself, while meningitis is an infection of the linings surrounding the brain. Infections may also be associated with abscesses or collections of pus within the brain. Lack of oxygen The brain requires oxygen to function; and without it the brain shuts down. There is a very short time to get oxygen back to brain tissue before there is permanent damage. Most research suggests that the time window is four to six minutes. The body provides oxygen to the brain through the lungs. The lungs extract oxygen from the air, hemoglobin in red blood cells pick up the oxygen, and the heart pumps blood through normal blood vessels to cells in the body. If any part of the system fails, the oxygen supply to the brain can be interrupted. The most common failure occurs with heart rhythm disturbances. The coordinated electrical beat of the heart is lost and the heart muscle doesn't squeeze blood adequately; no blood is pumped to the brain and it stops functioning almost immediately. Lungs can also fail; examples include pneumonia, emphysema, or asthma. In each case, inflammation in the lung tubes (bronchi or bronchioles) or lung tissue makes it difficult for oxygen to get into the lungs and transferred into the blood stream. Hemoglobin also takes carbon dioxide, the waste product of metabolism, and returns it to the lungs to be exhaled. Elevated levels of carbon dioxide in the blood can affect brain function to cause coma. Anemia, or low red blood cell count, can cause the brain to fail directly, or more likely it causes other organs like the heart to fail. The heart, like any other muscle requires oxygen to function. Anemia can occur chronically or it can be due to an acute blood loss (examples include trauma, bleeding from the stomach). If the blood loss is slow, the body is better able to adapt and tolerate low hemoglobin levels; if the bleeding occurs quickly, the body may be unable to compensate, the result being inadequate oxygen supply to tissues such as the brain. Hypoglycemic coma All cells in the body need glucose and oxygen to perform their functions by aerobic (oxygen requiring). While other parts of the body can continue for short periods of time without oxygen (anaerobically), the brain cannot. Without glucose, brain function stops. Hypoglycemia (low blood sugar) most often occurs in people with diabetes who have given themselves too much insulin or have not taken in enough food. In normal physiology, the pancreas makes insulin and balances the amount it produces with the amount of glucose in the blood stream. Diabetics need to inject insulin into their body, or take medication to stimulate the pancreas to make insulin. Monitoring blood sugars is critical to avoid hypoglycemic coma. Poisons There are two sources of poisons that can affect the brain, those that we take in (through ingestion or inhaling), and those that the body generates and cannot dispose of in some way. If the body can be considered a factory, it needs to have the ability to get rid of the waste products that are made when the body generates energy. These waste products can cause different organs in the body to fail, including the brain. The liver performs many functions including glucose and protein manufacturing. It also breaks down and metabolizes chemicals in the body. When the liver fails different chemicals like ammonia can accumulate and can cause brain cells to stop functioning. Hepatic encephalopathy (hepatic=liver + encephalo=brain + pathy=disease) or hepatic coma occurs when the liver fails because of an acute or chronic injury. The most common cause is cirrhosis due to alcoholism. The kidneys filter blood to rid the body of waste products. When the kidneys fail, a variety of waste products can accumulate in the bloodstream and cause direct or indirect damage to the brain. An example of indirect causes would be an elevated potassium level affecting heart electrical activity. Direct causes include uremia, where blood urea levels rise and are directly toxic to brain cells. Common causes of kidney failure include poorly controlled diabetes and high blood pressure. The thyroid acts as the thermostat for the body and regulates the speed at which the body functions. If thyroid levels gradually drop too low over a period of time myxedema coma can occur because of profound hypothyroidism. Ingestions can cause the brain to slow down, speed up or alter its perception of the world. Some ingestions may cause coma in an indirect way. Acetaminophen overdose has a delayed effect. It is directly toxic to the liver, but takes a few days before liver failure occurs, leading to hepatic coma and potentially death. Alcohol is probably the most common cause of ingested poison or toxin, leading to altered mental status and coma. In acute alcohol intoxication, the brain is directly poisoned. Blood alcohol levels fall when the alcohol is metabolized by the liver, but depth of intoxication can be so great it shuts off many of the involuntary brain activities that control breathing and maintain muscle function. Opiates like pain pills or heroin can cause similar slowing of brain function. Cocaine and amphetamines are the common "uppers" or brain stimulants. These brain stimulants cause an adrenaline-like body response, thus blood pressure and heart rate spiral out of control and the risk of heart attack, heart rhythm disturbances, or bleeding in the brain are increased. How is coma assessed? When a patient presents in coma, diagnosis and treatment begin simultaneously. Initial treatment is aimed at addressing immediate life-threatening issues: * Are the ABCs intact? Is the patient's airway open? Are they breathing? Do they have good circulation (a heartbeat and blood pressure)? * Is the patient hypoglycemic? The blood sugar can be checked by a quick fingerstick bedside test and if it is low, glucose can be administered under the tongue or intravenously. Patients with diabetes may also have a Glucagon injection kit that can be administered to treat low blood sugar. * Did the patient ingest a narcotic? Naloxone (Narcan) may be given intravenously to reverse an overdose situation. History remains the important key to the diagnosis. Since the patient cannot be the source of information, questions are asked of family, friends, bystanders, and rescue personnel. For example, imagine a person sitting at a bar who falls down, hits his head and is in a coma. While it might be easy to jump to the conclusion that he was intoxicated, fell, and bled in his brain, other scenarios need to be considered. Did he have a heart attack, did he suffer a stroke, or was this perhaps a diabetic medication reaction and the blood sugar was low. Once the patient has been stabilized with acceptable vital signs, physical examination will include a complete neurologic assessment. From head to toe, this may include examination of the eyes, pupils, face movements to assess cranial nerves including facial movement and gag reflex, extremity movement and reaction to stimulation, tendon reflexes and other testing of spinal cord function. There is special attention paid to symmetry in the neurology exam, since lack of movement or response on one side of the body may be caused by bleeding inside the skull or by stroke. General examination surveys the skin for cuts, scrapes, wounds, etc. The Glasgow Coma Scale score will be documented; the deeper the coma, the lower the score. Please appreciate that a person with a "normal" Glasgow Coma Scale of 15 still can be in coma. Once the initial screening physical examination complete, a more detailed exam will likely occur to include the lungs, the heart, and the abdomen. Repeated neurologic assessment is key to monitoring the status of the patient and determining if the coma is improving, worsening or remaining stable. What tests are there for coma? The strategy to decide which tests will help provide a diagnosis will depend upon the suspected cause. Many times, the cause involves many factors and the sequence of events will require serious detective work. Blood tests, electrocardiogram and CT scan of the head are most often obtained. Further test options depend upon the patient's situation. What is the outcome and prognosis for a patient in a coma? Depending upon the diagnosis, the evaluation may be no more than assessing blood sugar, treating hypoglycemia, and having complete resolution of the situation. On the other hand, the cause of coma may be a catastrophic brain hemorrhage without hope for significant recovery. The outlook very much depends on the cause of the coma and the ability to correct the particular situation. Induced Coma There are times when a patient has brain injury or inflammation, and part of the treatment plan is to decrease intracranial pressure and rest the brain. Barbiturate medications such as Pentothal and pentobarbital can be injected similar to providing a general anesthetic. These medications can decrease the metabolic rate. Another effect is to constrict or narrow blood vessels and hopefully decreasing the volume of blood in the skull thereby decreasing pressure within it. This technique is often used in patients with head trauma, ruptured aneurysms, and stroke. |
