|
Pulmonologist
|
| 1 |
What is a pulmonologist/pulmonary specialist?
|
Answer |
| 2 |
What is pulmonology?
|
Answer |
| 3 |
What are other names for pulmonology?
|
Answer |
| 4 |
What are the most common conditions of patients who are admitted to hospital having respiratory conditions?
|
Answer |
| 5 |
What should a primary care physician know to be successful in other human healthcare settings like intensivist, hospitalist, emergency medicine specialist (emergency room), emergency medicine specialist (first responder), physician-scientist, physician-surgeon?
|
Answer |
| 6 |
What should every physician know about mathematics in human health care?
|
Answer |
| 7 |
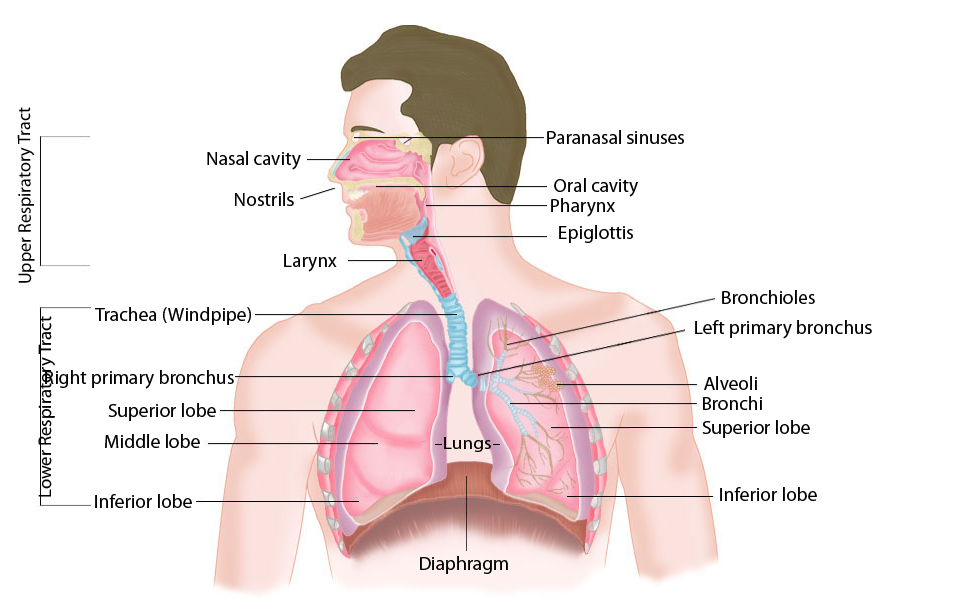
What should a primary care physician, emergency medical specialist, or any other type of physician know about the human respiratory system?
|
Answer |
| 8 |
What are the most common complaints patient have with underlying pulmonary conditions?
|
Answer |
| 9 |
What are the four components of the pulmonary examination?
|
Answer |
|
Respiratory Disorders
|
| 1 |
What Are the Types of Lung Disease?
|
Answer |
| 2 |
What questions do we need to follow up on?
|
Answer |
| 3 |
What is respiratory failure?
|
Answer |
| 4 |
What are other names for respiratory failure?
|
Answer |
| 5 |
When does a person get combination of acute and chronic respiratory failure?
|
Answer |
| 6 |
How have computers and Internet enhanced human heath care around the planet earth?
|
Answer |
| 7 |
What is the difference between types 1 and type 2 respiratory failure?
|
Answer |
| 8 |
What is acute respiratory failure?
|
Answer |
| 9 |
What are the individuations of mechanical ventilation in acute hypoxemic respiratory failure?
|
Answer |
| 10 |
What should an internist know about mechanical ventilation?
|
Answer |
| 11 |
What are the types of mechanical ventilation?
|
Answer |
|
Pulse oximeter
|
| 1 |
What is normal human value of oxygen saturation Spo2 by pulse oximeter?
|
Answer |
| 2 |
What do manufacturers of pulse oximeters have to do?
|
Answer |
| 3 |
What is a pulse oximeter?
|
Answer |
| 4 |
How to use a pulse oximeter?
|
Answer |
| 5 |
What does a pulse oximeter reading mean?
|
Answer |
| 6 |
What is the Perfusion Index (PI) in a pulse oximeter?
|
Answer |
| 7 |
How accurate is a pulse oximeter?
|
Answer |
| 8 |
Which finger to use in a pulse oximeter?
|
Answer |
| 9 |
Why keep a pulse oximeter at home?
|
Answer |
| 10 |
What is pulse oximetry?
|
Answer |
| 11 |
Why might you need pulse oximetry?
|
Answer |
| 12 |
What are the risks of pulse oximetry?
|
Answer |
| 13 |
How do you get ready for pulse oximetry?
|
Answer |
| 14 |
What happens during pulse oximetry?
|
Answer |
| 15 |
What happens after pulse oximetry?
|
Answer |
Type 1 and Type 2 respiratory failure: Prevent, Detect, Intervene
SUCCESSFUL MANAGEMENT OF MIXED RESPIRATORY FAILURE
|
| 1 |
What is respiratory failure?
|
Answer |
| 2 |
What causes respiratory failure?
|
Answer |
| 3 |
What are the symptoms of respiratory failure?
|
Answer |
| 4 |
How is respiratory failure diagnosed?
|
Answer |
| 5 |
What are the treatments for respiratory failure?
|
Answer |
| 6 |
What are the types of respiratory failure?
|
Answer |
| 7 |
What is acute respiratory failure?
|
Answer |
| 8 |
What are the symptoms of acute respiratory failure?
|
Answer |
| 9 |
What causes acute respiratory failure?
|
Answer |
| 10 |
Who is at risk for acute respiratory failure?
|
Answer |
| 11 |
Who is at risk for acute respiratory failure?
|
Answer |
| 12 |
What can you expect in the long-term?
|
Answer |
| 13 |
What is chronic respiratory failure?
|
Answer |
| 14 |
What are the symptoms of chronic respiratory failure?
|
Answer |
| 15 |
What causes chronic respiratory failure?
|
Answer |
| 16 |
How is chronic respiratory failure diagnosed?
|
Answer |
| 17 |
How is chronic respiratory failure treated?
|
Answer |
| 18 |
What are the potential complications of chronic respiratory failure?
|
Answer |
| 19 |
How do you calculate respiratory failure?
|
Answer |
| 20 |
When does respiratory failure need intensive care?
|
Answer |
| 21 |
How should you care for elders at home?
|
Answer |
|
Vital signs
|
| 1 |
What are the vital signs of human organ systems functions?
|
Answer |
| 2 |
What is the normal respiratory rate for a newborn, infant, toddler, preschooler, school age child, and adolescent?
|
Answer |
| 3 |
What is the normal pulse rate for a newborn, infant, toddler, preschooler, school age child, and adolescent?
|
Answer |
| 4 |
What is the lower limit of normal systolic blood pressure in a newborn, infant, toddler, preschooler, school age child, and adolescent?
|
Answer |