| Admissions | Ambassadors | Accreditation | A to Z Degree Fields | Books | Catalog | Colleges |Contact Us | Continents/States | Construction | Contracts | Distance Education | Emergency | Emergency Medicine | Examinations | English Editing Service | Forms | Faculty | Governor | Grants | Hostels | Honorary Doctorate degree | Human Services | Human Resources | Internet | Investment | Instructors | Internship | Login | Lecture | Librarians | Languages | Manufacturing | Membership | Observers | Publication | Professional Examinations | Programs | Professions | Progress Report | Recommendations | Ration food and supplies | Research Grants |Researchers | Students login | School | Search | Software | Seminar | Study Center/Centre | Sponsorship | Tutoring | Thesis | Universities | Work counseling |
Patient in a Coma
Coma-Related Skills and Knowledge
|
What rules should you follow in this situation?
|
When a patient goes into a coma, the facts with answers to the mentioned questions from emergency medicine physicians, critical care physicians, and supervisors should be displayed through the Internet for further deliberations about the correct diagnosis and treatment.
The state police are required to assist in these public services. This is in addition to replacing the licensing resources for physicians in American states and worldwide. They are engaging in medical negligence and then putting everything under some other heading, including coronavirus, that is not justified. The virus is an issue for the current situation of the public, but it is not necessarily the cause and circumstance of so many deaths according to Doctor Asif Qureshi. Various treasuries should immediately forward large government grants and government checks so that Doctor Asif Qureshi can educate American lawmakers, including all governors and specific required physicians through the Internet. At this point there is a need to teach Illinois emergency medicine physicians and critical care physicians the reversible causes of cardiac arrest, the reversible causes of coma, and treatment. |
Emergency health assessment on the spot.
Assessment in medical emergency situation.
Analysis of complaints, incidents, issues, and problems.
|
How do you know a person is in a coma? How do you know a person is not in a coma? How do you know a human being has collapsed and needs cardiopulmonary resuscitation? When do you start cardiopulmonary resuscitation? How do you start cardiopulmonary resuscitation in adults who suddenly fall unconscious? What should be your first question in case a patient is referred to you? Questions that must be answered. Where is the patient now? How old is the patient? What is the gender of the patient? Who is reporting this emergency? What seems to be the complaint? What seems to be the problem? Glasgow Coma scale analysis. First, analyze Glasgow Coma scale, then analyze vital signs including consciousness. When was the patient normal? Can the patient open both eyes spontaneously? Can the patient talk or make noise relevant to age? Can the patient walk or move extremities relevant to age? Here are further guidelines. Here are further guidelines. |
|
Are there any differences between cardiac arrest and a coma? How do you know a person is in a coma? How do you know a person is not in a coma? How do you know a human being has collapsed and needs cardiopulmonary resuscitation? Are there any differences between cardiac arrest and a coma? Yes. Cardiac arrest: What are the findings? Sudden collapse No pulse No breathing Loss of consciousness Sometimes other signs and symptoms occur before sudden cardiac arrest. These might include: Chest discomfort Shortness of breath Weakness Palpitations In a coma, the individual has a pulse and is breathing. In a coma, the individual cannot engage in spontaneous eye opening, talking, or walking. How do you know a human being has collapsed and needs cardiopulmonary resuscitation? Start with the coma scale. When should you start on-the-spot cardiopulmonary resuscitation? Was the patient able to see, talk, and move a few minutes earlier? Yes. Can the patient open both eyes spontaneously? No. Can the patient talk or make noises relevant to age? No. Can the patient walk or move their extremities relevant to age? No. Put your hand on the radial pulse. Is there a pulse? No. Put your hand on the chest. Is there respiratory movement? No. The patient was able to see, talk, and move a few minutes earlier. There is no pulse, no breath movement, and/or no heart sounds at this point. Start cardiopulmonary resuscitation. |
Coma skills and knowledge.
Cardiac Arrest |
Patient in a Coma
|
Do you have a coma patient that needs an executive specific physician consultation via the internet? Coma-Related Skills and Knowledge What questions must a medical emergency physician on duty, a nurse, or a similar entity be ready with answers according to the program director, Dr. Asif Qureshi? Can you display the details via the internet? What is the profile of the patient? What is the coma scale of this patient at this point? Can you give details about the situation of the patient at this point? What are the patient’s vitals, including date, time, and location? Where is the Comprehensive Metabolic Panel (CMP) of the patient at this point? Where is the toxicology report of the patient at this point? Where is the arterial blood gas report of the patient at this point? Where are the other mentioned tests of the patient at this point? This patient is in a coma: What is the cause of it at this point? What is the treatment at this point? What regulators are responsible for circulating directives for a patient in a coma via the internet? Which is better: display the situation via the internet and prolong the life of the patient or hide the situation to cause premature death? How will a reasonable person answer this question via the internet? What did you understand? What is your answer via the internet? Patient in a coma: What tests are required? 1. CBC 2. Blood chemistry: Comprehensive Metabolic Panel (CMP) 3. Toxicology 4. ABG 5. Urine analysis. Urine test: Ketones 6. Serum osmolality 7. 12-lead ECG may be required, depending on potassium levels 8. Chest X-ray 9. Further tests depending on the situation, such as a brain scan (CT scan, MRI, EEG) and a sonography 10. Drug levels in certain situations if the person was taking any medications prior to the coma 11. Blood culture in the case of a coma due to septicemia, pneumonia, or a similar diagnosis 12. Further tests depending on the situation How many tests are included in the blood test basic metabolic panel? Usually 8 tests. What is included in the blood test basic metabolic panel? Glucose Calcium Sodium Potassium Bicarbonate Chloride Blood urea nitrogen Creatinine How many tests are included in the blood test comprehensive metabolic panel? Usually 14 tests. What is included in the blood test comprehensive metabolic panel? Alanine aminotransferase Albumin Alkaline phosphatase Aspartate aminotransferase Bicarbonate Bilirubin Blood urea nitrogen Calcium Chloride Creatinine Glucose Potassium Sodium Total protein What is the executive-level role of the program director, Dr. Asif Qureshi, in this situation? In this situation, the executive-level program director, Dr. Asif Qureshi, researches, plans, develops, implements, and circulates one or more of the professional training programs or professional services. All these professional questions and answers have been authored by the program director, Dr. Asif Qureshi. What is a SOAP note? It was originally referred to as a problem-oriented medical record (POMR). SOAP notes include four headings that correspond with each letter of the acronym. SOAP: subjective, objective, assessment, plan The plan or treatment written after each diagnosis here is part of a SOAP note. Dr. Asif Qureshi, the program director for medical emergency physicians and similar entities, has written a SOAP note for your practice. You have to follow the guidelines for the SOAP note displayed below. How does a specific physician write a SOAP note? 1. Subjective: Current problems or symptoms: What seems to be the problem? Answer these 10 questions: www.qureshiuniversity.com/assessment.html 2. Objective: Vitals, medical records, appearance, behavior, and mood: What are the patient’s vitals, including date, time, and location? 3. Assessment: This section combines subjective and objective sections. Answer: What is the diagnosis? 4. Plan: What is the plan of action? What is the treatment? |
What is the person’s medical history?
|
When was the person normal? When did person start to experience acute medical issues? What were the significant findings? When did the person go into coma? What is the profile of the treating physicians? How did the treating physicians verify the reversible causes of coma before the _______ of the person? What should be displayed on the Internet? Questions you need to answer on the Internet. What was the date and time circumstances when the patient went into a coma? What is the name of the patient? What is the date of birth of the patient? What is the name of the treating doctor seeing the patient every day, face to face and in person? What is the name(s) of the nurse(s) who see the patient every day? At what location is this patient receiving treatment? What is the patient’s medical history of the main medical problem, from first emergence until now? What other medical issues does the patient have? What are the patient’s vitals, including date, time, and location? What are the last known and previous pulse oximetry blood oxygen saturation results? What are the last known and previous blood biochemistry results of the patient? What is the diagnosis? What is the treatment? What should be included in a review of the diagnosis? What should be included in a review of the treatment? |
Office of the Director of Public Health Illinois: What is the requirement?
Issues that need public debate
Responsibilities of medical college deans in this situation.
|
Office of the Director of Public Health Illinois: What is the requirement? On or before April 22, 2020, deans of these medical colleges could not publicly elaborate on cardiac arrest and coma. On or after April 27, 2020, deans of these medical colleges should publicly elaborate on cardiac arrest and coma. These public deliberations are relevant to the existing situation. What is on the list? 1. Northwestern University Feinberg School of Medicine, 420 E. Superior St., Chicago, IL 60611 2. University of Illinois College of Medicine at Chicago Dean's Office, 1853 W. Polk St. Room 131 (M/C 784), Chicago, IL 60612 3. Rush Medical College, 600 S. Paulina St. Suite 202, Chicago, IL 60612 4. Chicago Medical School of Rosalind Franklin University of Medicine and Science, 3333 Green Bay Road North, Chicago, IL 60064 5. Southern Illinois University School of Medicine, 801 N. Rutledge St., Springfield, IL 62702 6. University of Chicago Pritzker School of Medicine, 924 E. 57th St. Suite 104, Chicago, IL 60637 7. Midwestern University Chicago College of Osteopathic Medicine, 555 31st St., Downers Grove, IL 60515 8. Carle Illinois College of Medicine, 807 S. Wright St. Suite 320, Champaign, IL 61821 9. Loyola University Chicago Stritch School of Medicine, 2160 S. 1st Ave., Maywood, IL 60153 10. NorthShore University, 2650 N. Ridge Ave., Evanston, IL 60201 All other similar entities have similar responsibilities. Let the office of the Director of Public Health help them answer the mentioned questions relevant to the existing situation. They seem to only be after grants, salaries, and resources. Public service is not their focus. What is another word for a dean of a medical college? Principal of a medical college. Deans of these medical colleges who cannot elaborate on issues related to cardiac arrest and coma on or after April 27, 2020, must be replaced as soon as possible. What are the topics? Cardiac arrest Coma Cardiac Arrest What do you know about cardiac arrest? What should you know about cardiac arrest? Coma What do you know about coma? What should you know about coma? How can a coma be prevented? Why are these questions relevant to existing situations? Doctor Asif Qureshi has answers to these questions. With a simple click, the answers to the identified questions can be displayed for the public as well as specific physicians and administrators. Display the answers to these questions on your website. Doctor Asif Qureshi's focus is on public well-being. If you need Doctor Asif Qureshi to teach physicians and administrators, he can teach about cardiac arrest, coma, and many more healthcare issues. He can also forward guidelines and materials relevant to these issues to the Director of the Illinois Department of Public Health for circulation to others. Areas in various states do not have in-person face-to-face critical care facilities. Which areas in various states do not have in-person face-to-face critical care facilities? Www.qureshiuniversity.com/criticalcareworld.html Also known as areas with zero ICU Beds. Here are Doctor Asif Qureshi’s guidelines. There are 47 causes of coma. There are 46 reversible causes of coma. The treatment is to fix the underlying cause. If others mention or someone else has mentioned that this patient has coronavirus, then emergency medicine physicians and critical care physicians should also focus on the 46 reversible, treatable causes of coma in addition to coronavirus-related issues. The director of the state’s public health entity can provide statistics. The governor of the state can provide insights about the economy and resources required. It is the duty and responsibility of emergency medicine physicians and critical care physicians to guide actions in this situation. As of 5 pm on April 17, 2020, not a single emergency medicine physician or critical care physician from any American state had come forward to provide guidelines for other emergency medicine physicians, critical care physicians, or similar health care professionals. You can imagine the situation in other parts of the world. If you have any further questions, call 773-561-6102 in Chicago, Illinois, or email Doctor Asif Qureshi at admin@qureshiuniversity.com |
What is a coma?
|
How many causes of a coma are there? At least 47. You have to correlate the causes of a coma and the causes of reversible cardiopulmonary arrest. How many reversible causes of cardiopulmonary arrest are there? At least 14. The treatment is to fix the underlying cause. How do you proceed if a person is in a coma? Find the cause of the coma. Treat the underlying cause. Identify the causes of the coma and fix the underlying causes. Here are further guidelines. What is the category of this coma? 1. Severe head injury. What is the cause of the head injury? 2. Primary brain disorder. What is the cause of this brain disorder? 3. A lack of oxygen to the brain. What is the cause of the lack of oxygen to the brain? 4. Severe general or metabolic illness. What is the specific cause of the severe general or metabolic illness? 1. Severe head injury, most commonly from: Motor vehicle accidents Violence Falls 2. Primary brain disorder Brain Tumor and Brain hemorrhage or Stroke Brain infection 3. Lack of oxygen to the brain due to: High Blood Pressure Very low blood pressure or Shock Cardiac Arrest Severe Seizure Disorder 4. Severe general or metabolic illness. Severe bodily infections Severe acute liver or Kidney Failure High carbon dioxide levels Carbon Monoxide Poisoning Toxicity from poisons, medication, Alcohol Abuse and Alcoholism , or Drug Abuse and Drug Addiction Abnormal hormone levels, such as from the thyroid or adrenal gland Abnormal blood chemistries, such as sodium or calcium Very low or very high levels of blood sugar Very low or very high body temperatures Severe nutrient deficiency Liver failure Kidney Failure Inherited metabolic diseases |
Causes
|
How many causes are there? At least 47. What is done in a critical care unit or medical emergency unit? 1. Constant and close monitoring of the patient. 2. Support for the organ systems of the patient using specific equipment. 3. Medication to keep the body functioning normally until the patient recovers. What is the treatment? Fix the underlying cause. Here are further guidelines. |
What are the causes of a coma?
| Dr. Asif Qureshi has authored these executive professional questions and answers. Dr. Asif Qureshi has elaborated on his experience and research; he can guide 19 specific types of physicians in addition to teachers, lawyers, engineers, specific physicians, law enforcement, and similar other professions. Some reference treatments are recommended from https://my.clevelandclinic.org/, mayoclinic.com, webmd.com, and cdc.gov on or after March 12, 2024. |
-
Alcohol Intoxication and Alcohol Poisoning
What are the acute complications of alcohol consumption?
Alcohol intoxication
Alcohol poisoning
In what locations do you find such cases?
Such cases are in the United States. In some cultures, you will not find such cases.
Alcohol intoxication: What is it?
Acute alcohol intoxication is a condition associated with drinking too much alcohol in a short amount of time.
What are the chronic complications of alcohol consumption?
Alcohol use disorder
Here are further guidelines: https://www.qureshiuniversity.com/alcohol.html
What must be monitored?
Blood alcohol content (BAC)
Alcohol intoxication: What are the findings? Alcohol intoxication: What are the signs and symptoms?
1. Sobriety or low-level intoxication: The blood alcohol content (BAC) of the person is 0.01 to 0.05 percent.
2. Euphoria: The blood alcohol content (BAC) of the person is 0.03 to 0.12 percent.
3. Excitement: The blood alcohol content (BAC) of the person is 0.09 to 0.25 percent.
4. Confusion: The blood alcohol content (BAC) of the person is 0.18 to 0.30 percent.
5. Stupor: At this stage, the blood alcohol content (BAC) of the person is 0.25 to 0.40 percent.
6. Coma: At this stage, the blood alcohol content (BAC) of the person is 0.35 to 0.45 percent.
7. Death: At this stage, the blood alcohol content (BAC) of the person is 0.45 percent or above.
At a BAC of 0.45 percent or above, a person is likely to die from alcohol.
Diagnosis
In addition to checking for visible signs and symptoms of alcohol poisoning, your doctor will likely order blood and urine tests to check blood alcohol levels and identify other signs of alcohol toxicity, such as low blood sugar.
Alcohol intoxication: What are the findings?
The blood alcohol content (BAC) of the person at this stage will range from 0.03 to 0.12 percent.
Alcohol Poisoning: What are the findings?
The blood alcohol content (BAC) of the person at this stage will range from 0.35 to 0.45 percent.
Alcohol Poisoning: What are the signs and symptoms?
Coma
Treatment
What is the treatment?
1. Conscious: Encourage the person to lie on their side in a safe place until help arrives.
2. Conscious and able to swallow: Encourage the person to drink water.
3. Stay with the person until medical help arrives.
4. Carefully monitor vital signs.
DUI Laws by State
In every state, it's illegal—a "per se" DUI—to drive with a blood alcohol concentration (BAC) of .08% or more.
Alcohol poisoning treatment usually involves supportive care while the body rids itself of the alcohol. This typically includes:
Monitoring to prevent breathing or choking problems.
Oxygen therapy.
Fluids given through a vein to prevent dehydration.
Use of vitamins and glucose to help prevent serious complications.
Unconscious:
1. Prevent choking on vomit.
2. Prevent breathing or choking problems with a breathing tube that opens the airway.
3. Give oxygen therapy.
4. Give intravenous (IV) fluids to prevent dehydration.
5. Give vitamins and glucose (sugar) to prevent complications.
6. Fit a catheter, which allows urine to drain into a bag, so the person does not wet themselves.
7. Pump the stomach (gastric lavage) to minimize the body’s absorption of already-ingested alcohol.
8. Give activated charcoal to further minimize the body’s absorption of alcohol.
Is there a new patient?
What is the blood alcohol content in this situation?
How was it measured?
From what situation was the patient recovering?
Is the patient conscious or unconscious?
What is the treatment?
See treatment for a conscious patient.
See treatment for an unconscious patient.
Hemodialysis is indicated in certain types of alcohol poisoning.
People who accidentally consume methanol or isopropyl alcohol may need hemodialysis. This is a mechanical way of filtering waste and toxins from the blood. It can speed the removal of alcohol from the blood.
Diabetic Ketoacidosis or Hyperosmolar Coma or Hypoglycemia:
Check blood sugar every hour.
Check blood sugar every hour until normal.
How could this be prevented?
Maintain normal blood sugar levels.
Maintain normal fasting blood sugar levels at 70-99 mg/dL.
Maintain normal blood sugar levels after eating to not less than 70 mg/dL or more than 140 mg/dL.
-
Hypovolemic Shock
Hypovolemic shock: What causes it?
1. Bleeding from a gunshot wound
2. Bleeding from blunt traumatic injuries due to the mentioned cause
3. Bleeding from serious cuts or wounds
4. Bleeding from the digestive tract
5. Blood in your urine
6. Endometriosis
7. Excessive or prolonged diarrhea
8. Excessive sweating
9. Internal bleeding from abdominal organs or ruptured ectopic pregnancy
10. Protracted or excessive vomiting
11. Severe burns
12. Significant vaginal bleeding
13. Any other issue specified
Hypovolemic shock: What is the treatment? How is hypovolemic shock treated?
Find the underlying cause. Treat the underlying cause.
Start an intravenous line. Start normal saline intravenous relevant to hypovolemia.
If hemorrhagic shock occurs, start intravenous blood relevant to blood loss. Do not continue intravenous blood for more than 4 hours.
If you know better recent advances in treatments that can prolong life and enhance the well-being of the victim, email Dr. Asif Qureshi at admin@qureshiuniveristy.com.
Why was there need for Dr. Asif Qureshi to elaborate on these issues?
See the findings.
Who did not have relevant skills and knowledge about comas and were getting executive remuneration?
See the list. So many people died because of their harms.
What must others know?
They had a duty to serve the people.
They were getting income to serve the people.
They failed to serve the people.
They failed to have the skills and knowledge required for these executive jobs.
Those who selected, nominated, or confirmed them had a duty to verify their skills and knowledge.
Irreparable harms have occurred.
They should lose their executive job with further proceedings.
Those who nominated or confirmed them do not have executive healthcare skills and knowledge.
Few of them have the executive skills of an accountant. This is not enough. They must have problem-solving skills relevant to their executive job. <
Unconsciousness or Coma
-
Epileptic Fits
Seizures
Status Epilepticus
Essentials of Diagnosis
What is it?
A prolonged seizure lasting 5–15 minutes
Continuous or multiple seizures without intervening periods of consciousness
Clinical Findings
A prolonged seizure lasting more than 5 minutes, or multiple seizure episodes without intervening periods of consciousness defines status epilepticus. Search carefully for seizure activity in the comatose patient. Manifestations may be subtle (eg, deviation of head or eyes; repetitive jerking of fingers, hands, or one side of the face).
Protect the Airway
Insert a nasopharyngeal airway. Administer 100% oxygen by nasal cannula or non-rebreathing face mask and monitor with pulse oximetry. Prepare for possible endotracheal intubation in the event that anticonvulsants fail to terminate the seizure.
Insert an Intravenous Catheter
Obtain blood specimens for glucose, electrolytes, magnesium, and calcium determinations; hepatic and renal function tests; and complete blood count; as well as 3–4 tubes of blood for possible toxicology screen or determination of drug levels (including anticonvulsants if patient is known or suspected to be taking them).
Rule-Out Hypoglycemia
Obtain a bedside glucose and give glucose, 50 mL of 50% solution IV if the patient is hypoglycemic. Note: If malnutrition is suspected, give thiamine, 100 mg IV, slowly prior to, or at the same time as, glucose.
What is the treatment?
Pharmacological Treatment Protocol
First-Line Agent
Benzodiazepines
Give lorazepam, 2–4 mg (0.05–0.1 mg/kg) IV every 3–4 minutes to 8 mg total in adults and an additional dose of 0.05 mg/kg can be given in children. Diazepam, 5–10 mg (0.25 mg/kg) IV every 3–4 minutes up to 30 mg total dose in adults and 5 mg in children. These drugs have been shown to be equally effective as first-line choices. Lorazepam has a longer duration of action compared to diazepam. Because of this property, lorazepam is currently considered the drug of choice. If venous access cannot be obtained, diazepam can be given rectally, endotracheally, or intraosseously, or midazolam, 0.2 mg/kg, can be given intramuscularly.
Second-Line Agent
Phenytoin or Fosphenytoin
If the seizure persists after adequate doses of benzodiazopines, give phenytoin 20 mg/kg by IV infusion at a rate of 50 mg/min or slower. If the seizure persists, an additional 10 mg /kg is given. Infusion of phenytoin at more rapid rates (especially if given into centrally placed IV lines) can precipitate cardiac arrhythmias or hypotension. These unwanted hemodynamic and cardiac side effects can be avoided by the use of fosphenytoin, a prodrug of phenytoin. Fosphenytoin dosages are expressed as phenytoin equivalents (PE). Advantages of fosphenytoin are that it can be administered faster than phenytoin (150 PE/min) and be given intramuscularly if needed. The standard dose ...
-
Emergency treatment for severe hyperglycemia
Acute and Chronic Complications of Diabetes
- What are the acute complications of diabetes? Answer
- What are the chronic complications of diabetes? Answer
- When do blood sugar values need emergency attention for diabetic ketoacidosis or hyperosmolar coma or hypoglycemia? Answer
- What must happen next? Answer
- What if you have 300 mg/dl or more blood sugar? Answer
- What tests must be done? Answer
- Diabetic ketoacidosis or hyperosmolar coma: How is it diagnosed? Answer
- What are the statistics relevant to diabetes for the number and rate of emergency department visits among individuals 18 years or older in the United Diabetic Ketoacidosis What is the treatment? Answer
- What must you monitor? Answer
- What do the statistics reveal? Answer
- How do you classify diabetic ketoacidosis? Answer
- What must be given for fluid therapy in patients with diabetic ketoacidosis? Answer
- What must be given in electrolyte therapy in patients with diabetic ketoacidosis? Answer
- What must be given relevant to insulin in patients with diabetic ketoacidosis? Answer
- What must be the focus or aim of insulin therapy in patients with diabetic ketoacidosis? Answer
- Hyperosmolar Coma Who gets hyperosmolar hyperglycemic state complications? Answer
- Hyperosmolar Hyperglycemic State (HHS): What is the treatment? Answer
- What must be monitored in this situation? Answer
- How is dehydration corrected in HHS treatment? Answer
- What about insulin in HHS treatment? Answer
- What else is important in HHS treatment? Hypoglycemia Answer
- What is considered low blood sugar? Answer
- Does the patient have recurrent hypoglycemia? Answer
- Where exactly is thiamin (vitamin B1) utilized in glycolysis? Answer
- What can happen due to thiamine deficiency? Answer
Coma
Diabetic Ketoacidosis or Hyperosmolar Coma or Hypoglycemia
Acute and Chronic Complications of Diabetes
What are the acute complications of diabetes?
Diabetic ketoacidosis
Hyperosmolar coma
Diabetic hypoglycemia or other causes of low blood sugar
What are the chronic complications of diabetes?
https://www.qureshiuniversity.com/diabetes.html
When do blood sugar values need emergency attention for diabetic ketoacidosis or hyperosmolar coma or hypoglycemia?
If blood sugar is 240 mg/dl or more according to the CDC and WebMD.
If blood sugar is 300 mg/dl or more according to the Mayo Clinic (mayoclinic.com).
According to Dr. Asif Qureshi, we will focus on blood sugar that is 200 mg/dl or more as needing medical emergency attention from a specific physician.
Normal range of fasting blood sugar (fasting means you have not eaten in the preceding 8 hours): 70-99 mg/dL
Fasting blood sugar: 100-125 mg/dl indicates pre-diabetes
Fasting blood sugar: more than 126 mg/dl indicates type 1 or type 2 diabetes
Random blood sugar after eating should not be less than 70 mg/dL or more than 140 mg/dL.
Random blood sugar that exceeds 200 mg/dL after eating is likely a medical emergency.
Hypoglycemia: Blood sugar below 70 mg/dL is considered low. Usually blood sugar below 55 mg/dL is considered severely low. The patient will likely be unconscious in this situation.
Here we are focusing on blood sugar values that need emergency attention.
What must happen next?
Test for ketones
Anytime you’re sick or your blood sugar is 240 mg/dL or above, use an over-the-counter ketone test kit to check your urine or a meter to test your blood for ketones every 4 to 6 hours. Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated immediately.
What if you have 300 mg/dl or more blood sugar?
Report to the nearest medical emergency hospital as soon as possible.
Even if tests for ketones are not available, report to the nearest medical emergency hospital.
What tests must be done?
1. CBC
2. Blood chemistry: Comprehensive Metabolic Panel (CMP)
3. ABG
4. Urine test: Ketones
5. Serum osmolality
6. 12-lead ECG may be required depending on potassium levels
Diabetic ketoacidosis or hyperosmolar coma: How is it diagnosed?
CBC, blood chemistry, ABG, UA, ketones, serum osmolality, and 12-lead ECG may be required depending on potassium levels
DKA HHS/Hyperosmolar Coma/Hyperosmolar Hyperglycemic State (HHS): Serum glucose more than 240 more than 600 PH less than 7.3 more than 7.3 HCO3 less than 18 greater than 18 Urine/Serum Ketones positive elevated negative or not enough to be abnormal Anion Gap greater than 12 less than 12 Serum Osmolarity variable normal or high super high greater than 320
What are the statistics relevant to diabetes for the number and rate of emergency department visits among individuals 18 years or older in the United States in 2019?
Reference source for these statistics: https://www.cdc.gov/diabetes/data/statistics-report/index.htmlDiabetes as any listed diagnosis 17,939,000 patients Hyperglycemic crisis 255,000 patients Diabetic ketoacidosis 229,000 patients Hyperosmolar hyperglycemic syndrome 26,000 patients Hypoglycemia 246,000 patients
These professional questions and answers have been authored by Dr. Asif Qureshi.
These professional questions and answers were not at https://www.cdc.gov on or before March 5, 2024.
Diabetic Ketoacidosis
What is the treatment?
1. IV Normal Saline: How do you calculate IV fluids required in this situation?
2. Insulin: 50 units to decrease blood sugar by 50 mg/dl. For how many minutes should this be given?
What must you monitor?
Make sure the patient does not become hypoglycemic.
Make sure the patient does not get volume overload.
What do the statistics reveal?
Diabetic ketoacidosis accounts for 135,000 hospital admissions per year in the United States.
How do you classify diabetic ketoacidosis?
Mild
Moderate
Severe
Classification of diabetic ketoacidosis*
Parameter Mild Moderate Severe Serum bicarbonate (mmol/L) 15-18 10-<15 <10 Arterial pH 7.25-7.30 7.0-7.24 <7.0 Anion gap >10 >12 >12 Mental status Alert Alert/drowsy Stupor/coma
What must be given for fluid therapy in patients with diabetic ketoacidosis?
Normal saline (0.9% sodium chloride) is recommended as the initial IV fluid replacement in DKA. Initial IV fluid replacement starts with 0.9% sodium chloride at a rate of 15–20 ml/kg (about 1–1.5 L) over the first hour. Thereafter, the rate and type of fluids are determined by an assessment of the clinical condition.
What must be given in electrolyte therapy in patients with diabetic ketoacidosis?
Once the serum potassium level is ≤5.2 mmol/L, potassium replacement should be started to achieve a goal of maintaining it at 4–5 mmol/L. For levels between 3.3 and 5.2 mmol/L, replacement should be started using 20–30 mEq of potassium in each liter of IV fluids. If serum potassium at presentation is <3.3 mmol/L, insulin should not be started, as it can further lower serum potassium and potassium replacement at 20–30 mEq/h should be given until serum potassium level rises to >3.3 mmol/L.
What must be given relevant to insulin in patients with diabetic ketoacidosis?
Insulin is usually given via an IV, starting with a bolus of regular insulin at a dose of 0.1 unit/kg body weight and then, within 5 minutes, followed by a continuous infusion of regular insulin of 0.1 unit/kg/h.
In children, a bolus dose of insulin prior to the IV infusion is not recommended, as it does not improve clinical outcomes and may contribute to the development of cerebral edema.
With insulin therapy, plasma glucose levels are expected to be reduced by about 2.8–3.9 mmol/L (50–70 mg/dL)/h or 10% from initial glucose concentration after the first hour. If glucose levels do not decrease by these rates, hydration status and rates of IV fluids should be evaluated and optimized if necessary.
What must be the focus or aim of insulin therapy in patients with diabetic ketoacidosis?
Maintaining blood glucose levels at 8.3–11.1 mmol/L (150–200 mg/dL).
On or before March 7, 2024, these professional questions and answers authored by Dr. Asif Qureshi were not at https://www.ncbi.nlm.nih.gov/. They are encouraged to display these professional questions and answers authored by Dr. Asif Qureshi.
Reimbursements, significant grants, retroactive credits, and credits that will count toward retirement for Dr. Asif Qureshi are required.
Hyperosmolar Coma
Who gets hyperosmolar hyperglycemic state complications?
Adults with type 2 diabetes mellitus.
Hyperosmolar Hyperglycemic State (HHS): What is the treatment?
1. IV medications, including fluids to hydrate you.
2. Electrolytes (such as potassium) to balance the minerals in your body.
3. Insulin to regulate your blood sugar levels; 50 units of insulin to reduce blood sugar by 50 mg/dl.
Hyperosmolar Hyperglycemic State (HHS) Treatment
What must be monitored in this situation?
Treatment begins with intensive monitoring of the patient and laboratory values, especially glucose, sodium, and potassium levels.
How is dehydration corrected in HHS treatment?
An average of 9 L of 0.9% saline over 48 hours in adults. After urine output is established, potassium replacement should begin. A rate of 9 L of 0.9% saline over 48 hours in adults is recommended by https://www.aafp.org/.
Dr. Asif Qureshi recommends fewer IV fluids than this due to the risk of volume overload. Public debate should immediately take place to discuss these issues.
What about insulin in HHS treatment?
Once dehydration is partially corrected, adults should receive an initial bolus of 0.1 units of intravenous insulin per kg of body weight, followed by a continuous infusion of 0.1 units per kg per hour (or a continuous infusion of 0.14 units per kg per hour without an initial bolus) until the blood glucose level falls below 300 mg per dL. In children and adolescents, dehydration should be corrected at a rate of no more than 3 mOsm per hour to avoid cerebral edema.
What else is important in HHS treatment?
Monitor risk of fluid overloads.
First IV fluids, then insulin.
The identification and treatment of underlying and precipitating causes are necessary.
Phosphate replacement should be considered in patients with HHS only if hypophosphatemia is severe (less than 1.0 mEq per L [1.0 mmol per L]) or if respiratory depression, anemia, or cardiac dysfunction is present.
Treatment reference from: https://www.aafp.org/
American Diabetes Association: Management of DKA and HHS
Professional questions and answers were authored by Dr. Asif Qureshi.
Emergency treatment for severe hyperglycemia
If you have signs and symptoms of diabetic ketoacidosis or hyperosmolar hyperglycemic state, you may be treated in the emergency room or admitted to the hospital. (4p4) Emergency treatment can lower your blood sugar to a normal range. Treatment usually includes:
Fluid replacement. You'll receive fluids — usually through a vein (intravenously) — until your body has the fluids it needs. This replaces fluids you've lost through urination. It also helps dilute the extra sugar in your blood.
Electrolyte replacement. Electrolytes are minerals in your blood that are necessary for your tissues to work properly. A lack of insulin can lower the level of electrolytes in your blood. You'll receive electrolytes through your veins to help keep your heart, muscles and nerve cells working the way they should.
Insulin therapy. Insulin reverses the processes that cause ketones to build up in your blood. Along with fluids and electrolytes, you'll receive insulin therapy — usually through a vein. As your body returns to normal, your health care provider will consider what may have triggered the severe hyperglycemia. Depending on the circumstances, you may need additional tests and treatment.
-
Head Injuries
Cervical Spine Immobilization
Any patient with blunt force injury to the head should be suspected of having cervical spine injury until proven otherwise. Penetrating injuries to the torso and extremities not associated with blunt force are rarely associated with cervical spine injury. Cervical spine injury is associated with 5% of all blunt force injuries to the head; the greater the force, the greater the incidence of associated injury. Immobilization of the cervical spine during transport of a patient with potential injuries must include an appropriately sized and fitted cervical collar, head blocks, and a long, rigid spine board to which the patient is secured. Immobilize the cervical spine during evaluation by manual stabilization and logrolling the patient. Do not apply traction to the cervical spine.
Airway
Hypoxia is associated with increased morbidity and mortality in trauma patients. In patients with traumatic brain injury hypoxia is an independent risk factor for mortality with a 50% higher incidence that in those without hypoxia. Hypoxia must be avoided or corrected immediately. All patients with traumatic head injury should receive 100% oxygen by high-flow nonrebreathing mask as initial therapy. Keep the airway clear by suctioning of blood and secretions as needed. Remove foreign bodies, avulsed teeth, and dental appliances. Loss of gag reflex, inability to adequately clear secretions, or Glasgow Coma Scale (GCS) score of 8 or less are all indications to secure the airway with an endotracheal tube. Use clinical judgment to determine if a patient needs to be intubated in other situations, with priority on maintaining the airway during resuscitation, evaluation, and transport. Ventilate apneic or hypoventilating patients with an Ambu bag and 100% oxygen until intubation can be accomplished. Over ventilation is also dangerous to the head injured patient as hypocarbia will lead to cerebral vasospasm and worsen outcome. Avoid using a bag to provide positive-pressure ventilation to an actively breathing patient because this induces gastric distention.
Perform intubation while maintaining manual in-line cervical immobilization without applying traction. Rapid sequence induction intubation should be strongly considered for all patients. Once sedatives and paralytics have taken effect, remove the cervical collar and maintain manual stabilization. After intubation, secure the endotracheal tube and replace the cervical collar.
Orotracheal intubation is preferred because of the technical difficulty of nasotracheal intubation as well as the complications of bleeding, elevated intracranial pressure, and possible passage of the endotracheal tube through a fractured cribiform plate into the cranium. If orotracheal intubation is not successful, intubate the patient using a retrograde Seldinger technique, fiberoptic-guided intubation, or cricothyroidotomy depending on the equipment available immediately, the clinical status of the patient and the procedures with which the physician is most skilled. In addition, consider a temporizing device, such as a laryngeal mask airway, in the patient who is difficult to intubate. After intubation, confirm endotracheal tube position by auscultation over the lung fields and epigastrium.
Loss of gag reflex, inability to adequately clear secretions, or Glasgow Coma Scale (GCS) score of 8 or less are all indications to secure the airway with an endotracheal tube.
Endotracheal intubation
Here are further guidelines.
https://www.qureshiuniversity.com/endotrachealintubation.html
-
Hypoglycemia
Hypoglycemia
What is considered low blood sugar?
Blood sugar below 70 mg/dL is considered low.
Low blood sugar: What is the treatment?
1. Conscious: Usually blood sugar between 55-69 mg/dL, raise it by following the 15-15 rule: have 15 grams of carbs and check your blood sugar after 15 minutes.
A. 1 tablespoon of sugar, honey, or syrup.
B. 3-4 glucose tablets (follow instructions).
C. 4 ounces (½ cup) of juice or regular soda.
D. Hard candies, jellybeans, or gumdrops (see food label for how much to eat).
E. 1 dose of glucose gel (usually 1 tube; follow instructions).
Recheck blood sugar levels 15 minutes after treatment. If blood sugar levels are still under 70 mg/dL (3.9 mmol/L), eat or drink another 15 to 20 grams of fast-acting carbohydrate and recheck your blood sugar level again in 15 minutes. Repeat these steps until the blood sugar is above 70 mg/dL (3.9 mmol/L).
Have a snack or meal. Once your blood sugar is back in the standard range, eating a healthy snack or meal can help prevent another drop in blood sugar and replenish your body's glycogen stores.
Does the patient have recurrent hypoglycemia?
Treatment of an underlying condition.
1. Nutrition counseling
2. Adding, changing, or stopping medication if medication is the cause
3. Identifying if a tumor is present for tumor treatment.
2. Unconscious:
Usually blood sugar below 55 mg/dL is considered severely low. The patient will be usually unconscious. Injectable glucagon is the best way to treat severely low blood sugar.
Mild hypoglycemia
Moderate hypoglycemia
Severe hypoglycemia requires different treatment
Treatment
Immediate hypoglycemia treatment
If you have hypoglycemia symptoms, do the following:
Eat or drink 15 to 20 grams of fast-acting carbohydrates. These are sugary foods or drinks without protein or fat that are easily converted to sugar in the body. Try glucose tablets or gel, fruit juice, regular (not diet) soda, honey, or sugary candy. Recheck blood sugar levels 15 minutes after treatment. If blood sugar levels are still under 70 mg/dL (3.9 mmol/L), eat or drink another 15 to 20 grams of fast-acting carbohydrate, and recheck your blood sugar level again in 15 minutes. Repeat these steps until the blood sugar is above 70 mg/dL (3.9 mmol/L). Have a snack or meal. Once your blood sugar is back in the standard range, eating a healthy snack or meal can help prevent another drop in blood sugar and replenish your body's glycogen stores. Immediate treatment of severe hypoglycemia Hypoglycemia is considered severe if you need help from someone to recover. For example, if you can't eat, you might need a glucagon injection or intravenous glucose.
In general, people with diabetes who are treated with insulin should have a glucagon kit for emergencies. Family and friends need to know where to find the kit and how to use it in case of emergency.
If you're helping someone who is unconscious, don't try to give the person food or drink. If there's no glucagon kit available or you don't know how to use it, call for emergency medical help.
Treatment of an underlying condition
Preventing recurrent hypoglycemia requires your health care provider to identify the condition causing hypoglycemia and treat it. Depending on the cause, treatment may involve:
Nutrition counseling. A review of eating habits and food planning with a registered dietitian may help reduce hypoglycemia.
Medications. If a medication is the cause of your hypoglycemia, your health care provider will likely suggest adding, changing or stopping the medication or adjusting the dosage.
Tumor treatment. A tumor in your pancreas is typically treated by surgical removal of the tumor. In some cases, medication to control hypoglycemia or partial removal of the pancreas is necessary.
Take a look at this.
For most people with diabetes, hypoglycemia is when your blood sugar level is below 70 milligrams per deciliter (mg/dL) or 3.9 millimoles per liter (mmol/L).
For most people without diabetes, hypoglycemia is when your blood sugar level is below 55 mg/dL or 3.1 mmol/L.
Hypoglycemia requires immediate treatment by eating or drinking sugar/carbohydrates. Severe hypoglycemia can be life-threatening and requires treatment with emergency glucagon and/or medical intervention.
Severe hypoglycemia requires different treatment than mild or moderate hypoglycemia. If someone you know is having a hypoglycemia episode and is slurring their speech, disoriented or unconscious, don’t give them food or liquid. They could choke.
Severe hypoglycemia episodes require the use of emergency glucagon. This is a synthetic form of glucagon that you can administer as an injection or nasal powder (dry nasal spray), depending on the type. Synthetic glucagon triggers your liver to release stored glucose, which then raises blood sugar. Take a look at this.
-
High carbon dioxide levels
Oxygen therapy. A machine delivers extra oxygen through a breathing mask or small tube (cannula). You may get oxygen at home or in the hospital.
Managing underlying conditions. You provider may treat you with other medications or procedures, depending on what’s causing respiratory failure.
Hypercapnic respiratory failure
Hypoxemic respiratory failure
Perioperative respiratory failure
Respiratory failure due to shock
-
Poisoning
Victims of Poisoning with Coma, Seizures, or Marked Obtundation
Keep Airway Open
Establish and maintain an adequate airway and ventilation. Begin supplemental oxygen, 12 L/min, by nonrebreathing mask. If the patient has no gag reflex, intubate for airway protection, to facilitate oxygenation and to remove airway secretions. Continuously monitor oxygen saturation. Obtain Arterial Blood Gas and pH Measurements
Obtain arterial blood for blood gas and pH measurements to determine adequacy of ventilation and perfusion.
Gain Intravenous Access
Insert a large-bore (≥18-gauge) peripheral or central intravenous catheter, and draw blood for complete blood count, serum electrolyte and blood glucose measurements, and tests of renal and hepatic function.
Treat Coma Promptly
Give glucose, 50 mL of a 50% solution (25 g of glucose) intravenously over 3–4 minutes, if a normal blood glucose cannot be determined immediately. If the patient's response is weak or if narcotic overdose is suspected, as indicated by pinpoint pupils and shallow respirations, give repeated doses of naloxone 2 mg every 1–2 minutes up to a total dosage of 10–20 mg. Note: The duration of action of naloxone (2–3 hours) is shorter than that of many of the narcotics it reverses. Patients responding to naloxone must be observed for at least 3 hours after the last dose.
If alcoholism or malnutrition is suspected, give thiamine, 100 mg intramuscularly or in intravenous solution with or prior to glucose administration.
Maintain Circulation
Maintain circulation, and treat shock by restoring intravascular volume with intravenous infusion of crystal-loid solutions. Caution: Fluid overload and pulmonary edema may occur with overly vigorous hydration. Some medications (salicylates) put patients at higher risk for pulmonary edema. If administration of more than 20–30 mL/kg of crystalloid solution and usual doses of dopamine (ie, 5–15 μg/kg/min intravenously) fail to restore blood pressure, insert a central venous catheter and arterial pressure catheter to obtain pressure readings and help guide further therapy with fluids or pressor agents.
Treat Seizures
If the patient is experiencing seizures, give diazepam, 0.1–0.2 mg/kg, or lorazepam, 0.05 mg/kg, intravenously. If this is not effective, within a few minutes, repeat the dose. If the seizures continue, administer phenobarbital, 20 mg/kg, intravenously over 20 minutes. Phenytoin is ineffective for stopping seizures caused by most poisonings.
Start Electrocardiographic Monitoring
Start cardiac monitoring. Obtain a 12-lead electrocardiogram (ECG) and note especially the rate; rhythm; presence of arrhythmias; and PR, QRS, and QT intervals. If overdose of tricyclic antidepressants is suspected, obtain serial ECGs.
Perform Gastric Decontamination
Place a nasogastric or orogastric tube for the administration of activated charcoal. Activated charcoal may be premixed with a 70% ...
Here are further guidelines.
-
Trauma
Traumatic injuryWhat is the cause of trauma?
The Revised Trauma Score (RTS)
What is the Revised Trauma Score?
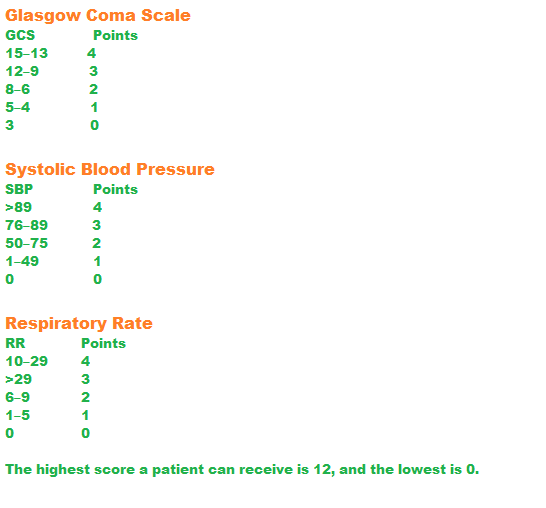
The Revised Trauma Score is made up of three categories: the Glasgow Coma Scale, systolic blood pressure, and respiratory rate.
The score ranges from 0 to 12. In START triage, a patient with an RTS score of 12 is labeled delayed, 11 is urgent, and 3–10 is immediate. Those who have an RTS below 3 are declared dead or highly unlikely to survive.
What does a lower Revised Trauma Score indicate?
A lower score indicates a higher severity of injury.
How do you calculate the Revised Trauma Score?
Trauma Management
Here are further guidelines.
Coma and Persistent Vegetative StateWhat is Coma and Persistent Vegetative State?
A coma is a profound or deep state of unconsciousness. An individual in a state of coma is alive but unable to move or respond to his or her environment. Coma may occur as a complication of an underlying illness, or as a result of injuries, such as head trauma. A persistent vegetative state (commonly, but incorrectly, referred to as "brain death") sometimes follows a coma. Individuals in such a state have lost their thinking abilities and awareness of their surroundings, but retain non-cognitive function and normal sleep patterns. Even though those in a persistent vegetative state lose their higher brain functions, other key functions such as breathing and circulation remain relatively intact. Spontaneous movements may occur, and the eyes may open in response to external stimuli. They may even occasionally grimace, cry, or laugh. Although individuals in a persistent vegetative state may appear somewhat normal, they do not speak and they are unable to respond to commands.
Is there any treatment?
Once an individual is out of immediate danger, the medical care team focuses on preventing infections and maintaining a healthy physical state. This will often include preventing pneumonia and bedsores and providing balanced nutrition. Physical therapy may also be used to prevent contractures (permanent muscular contractions) and deformities of the bones, joints, and muscles that would limit recovery for those who emerge from coma.
What research is being done?
Here are further guidelines.
Common causes of coma include:Anoxic brain injury
Cerebral infarction
Cerebral hemorrhage
Traumatic
Cerebral neoplasms
Hypertensive encephalopathy
Hypoglycemia
Metabolic encephalopathy
Myxedema
Status epilepticus
Toxic encephalopathy
Findings may suggest a cause:Hypothermia: Environmental exposure, near-drowning, sedative overdose, severe hypothyroidism, Wernicke encephalopathy, or, in older people, sepsis
Hyperthermia: Heatstroke, infection, stimulant drug overdose, or neuroleptic malignant syndrome
Fever, petechial or purpuric rash, hypotension, or severe extremity infections (eg, gangrene of one or more toes): Sepsis or central nervous system (CNS) infection
Needle marks: Drug overdose (eg, of opioids or insulin)
A bitten tongue: Seizure
Breath odor: Alcohol, other drug intoxication, or diabetic ketoacidosis
Hypotension or pulse abnormalities: Cardiac dysfunction with hypoperfusion
Difficulty breathing: Acute respiratory dysfunction from bacterial or viral illness
-
Kidney Failure
Uremic encephalopathyWhat are the signs of chronic kidney disease (CKD)? https://qureshiuniversity.com/chronickidneydisease.html
Approach Considerations
The presence of uremic encephalopathy in a patient with either acute kidney injury or chronic kidney disease is an indication for the initiation of dialytic therapy (ie, hemodialysis, peritoneal dialysis, continuous renal replacement therapy).
Address the following factors when treating uremic encephalopathy, which are also included in the standard care of any patient with ESRD:
Adequacy of dialysis
Correction of anemia
Regulation of calcium and phosphate metabolism
Administer medications (eg, iron, erythropoietin, phosphate binders, vitamin D analogues) for patients with ESRD to optimize their quality of life. Sedatives should be avoided.
Take a look at this.Further assessment of the situation.
Arterial blood gas
Acid-Base Disorders
Diagnosing Medical Acid Base DisordersAnnotation or definition. ABG interpreter Multiple Choice Questions- Acid Base Balance Normal Arterial Blood Gas Values Questions you need to answer. The Four Primary Disturbances of Acid-Base Balance Types of Acid-Base Disorders Why It Is Done
-
Infections
Encephalitis
Meningitis
Sepsis and Septic Shock
Infections. Infections such as encephalitis and meningitis cause swelling of the brain, spinal cord or the tissues that surround the brain. Severe cases of these infections can result in brain damage or a coma. -
Severe nutrient deficiency
Mini nutritional assessment
First name:
Last name:
Gender:
Age:
Weight, kg:
Height, cm:
Date:
Screening
-
A Has food intake declined over the past 3 months due to loss of appetite, digestive problems, chewing or
swallowing difficulties?
0 = severe decrease in food intake
1 = moderate decrease in food intake
2 = no decrease in food intake
-
B Weight loss during the last 3 months
0 = weight loss greater than 3 kg (6.6 lbs)
1 = does not know
2 = weight loss between 1 and 3 kg (2.2 and 6.6 lbs)
3 = no weight loss
-
C Mobility
0 = bed or chair bound
1 = able to get out of bed / chair but does not go out
2 = goes out
-
D Has suffered psychological stress or acute disease in the past 3 months?
0 = yes 2 = no
-
E Neuropsychological problems
0 = severe dementia or depression
1 = mild dementia
2 = no psychological problems
-
F1 Body Mass Index (BMI) (weight in kg) / (height in m)
2
0 = BMI less than 19
1 = BMI 19 to less than 21
2 = BMI 21 to less than 23
3 = BMI 23 or greater
Screening score
(max. 14 points)
12-14 points: Normal nutritional status
8-11 points: At risk of malnutrition
0-7 points: Malnourished
Is BMI <20.5?
Has the patient lost weight within the last 3 months?
Has the patient had a reduced dietary intake in the last week?
Is the patient severely ill? (e.g., in intensive therapy)
Severe Nutrient DeficiencyWhere exactly is thiamin (vitamin B1) utilized in glycolysis?
Glucose to Pyruvate
Pyruvate + Thiamin (B1) = Acetyl-CoA
Acetyl-CoA to ATP or Neurotransmitter synthesis
What can happen due to thiamine deficiency?
Thiamine deficiency is known as Wernicke-Korsakoff syndrome.
Take a look at this: Glycolysis
https://www.qureshiuniversity.com/glycolysis.html
Wernicke encephalopathy- What is it? Answer
- What causes it? Answer
- How many causes are there?Answer
- What are the risk factors? Answer
- What's normal? Answer
- How is it diagnosed?Answer
- What are the symptoms? Answer
- What are the signs? Answer
- What are the clinical findings? Answer
- What are the lab or investigation findings? Answer
- What is the treatment? Answer
- What are the workable treatment options? Answer
- How could this be prevented? Answer
Nutritional deficiencies of thiamine and niacin, rarely vitamin B (12), and possibly folate can cause a wide range of neuropsychiatric manifestations. Neurologic manifestations associated with these deficiency states are the focus of this review.
What is it?
Wernicke's encephalopathy (WE) is a severe neuropsychiatric disorder, which results from a nutritional deficiency of thiamine.
Diagnosis:
Brain magnetic resonance imaging confirmed the diagnosis of WE.
Interventions:
The patient was given thiamine and nutrition support therapy.
Other disorders caused by a lack of vitamin B1 include:
African seasonal ataxia.
Beriberi.
Central pontine myelinolysis (CPM).
Leigh’s disease.
Nutritional optic neuropathy.
Nutrition
How much food or nutrition does a human being need per day?
What is the difference between macronutrients and micronutrients?
Is there a difference between terms utilized for nutrients and food?
What is the difference between terms utilized for nutrients and food?
What is human starvation?
Why is an essential commodities act essential?
Here are further guidelines.
https://www.qureshiuniversity.com/nutrition.html
Last Updated: March 10, 2024 -
A Has food intake declined over the past 3 months due to loss of appetite, digestive problems, chewing or
swallowing difficulties?
