Who are the audience for these training programs in the state and outside the state?
Physician medical emergency room
Physician surgeon medical emergency
Physician medical emergency responder
Paramedics
Other advanced practitioners use ATLS
Police officers, particularly police patrolling officers
Others relevant to requirement
Questions that need to be answered.
What are other names for early management of severe trauma?
How should you go ahead in an acute trauma case?
What is included in primary survey of acute trauma patients?
What is early management of severe trauma?
Can the patient speak relevant to age?
What do you do if the airway of the patient is obstructed due to trauma?
What should you do next?
What should you look for?
What are examples of life threatening thoracic conditions?
What are the causes of preventable deaths after trauma?
How do you do a quick neurological assessment in trauma cases?
What should you do if there is altered level of consciosuness?
How should you cover the patient?
What is included in a secondary survey?
What is included in a tertiary survey of trauma cases?
Has there been trauma in the past few minutes?
Questions you need to answer
What should people know about trauma?
What should a medical doctor, nurse, paramedic, or counselor know about trauma?
What should a police officer or military officer know about trauma?
How should you evaluate a medical doctor regarding skills and knowledge of diagnosis and treatment of trauma?
|
Early Management of Severe Trauma
What are other names for early management of severe trauma?
Advanced trauma life support.
How should you go ahead in an acute trauma case?
On the spot assessment and management.
Primary survey.
Airway maintenance with cervical spine protection
Breathing and ventilation
Circulation with hemorrhage control
Disability/Neurologic assessment
Exposure and environmental control
Here are further guidelines
|
When the primary survey is completed, resuscitation efforts are well established, and the vital signs are normalizing, the secondary survey can begin.
Secondary survey.
| |
Tertiary survey.
|
Primary survey.
What is included in primary survey of acute trauma patients?
What is early management of severe trauma?
A simple mnemonic, ABCDE.
Airway maintenance with cervical spine protection
Can the patient speak relevant to age?
If yes, the airway is likely to be clear.
What do you do if the airway of the patient is obstructed due to trauma?
The airway can be opened using a chin lift or jaw thrust. Airway adjuncts may be required. If the airway is blocked (e.g., by blood or vomit), the fluid must be cleaned out of the patient's mouth by the help of suctioning instruments. In case of obstruction, pass an endotracheal tube.
Head tilt/Chin lift
Chin lift | 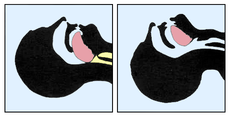
The head-tilt/chin-lift is a procedure used to prevent the tongue obstructing the upper airways. The maneuver is performed by tilting the head backwards in unconscious patients, often by applying pressure to the forehead and the chin.
The maneuver is used in any patient in whom cervical spine injury is not a concern and is taught on most _____ courses as the standard way of clearing an airway.
If cervical spine injury is a concern and/or the patient is immobilized on a long spine board and/or with cervical collar; the jaw-thrust maneuver can be used instead.
If the patient is in danger of aspirating; he or she should be placed in the recovery position or advance airway management should be used.
| |
Jaw-thrust maneuver | 
The jaw-thrust maneuver is a procedure used to prevent the tongue obstructing the upper airways. The jaw thrust maneuver is a technique used on patients with a suspected spinal injury and is used on a supine patient.
The maneuver is performed by placing the index and middle fingers to physically push the posterior aspects of the mandible upwards while their thumbs push down on the chin to open the mouth. When the mandible is displaced forward, it pulls the tongue forward and prevents it from obstructing the entrance to the trachea.
| |
Suctioning instruments | | |
Airway Adjuncts | Bag-Mask Ventilation
Nasopharyngeal/Oropharyngeal Airways |
Advanced airway management
Endotracheal tube. | Here are further guidelines.
|
Breathing and ventilation
What should you do next?
The chest must be examined by inspection, palpation, percussion, and auscultation.
What should you look for?
Subcutaneous emphysema and tracheal deviation must be identified if present.
The aim is to identify and manage six life-threatening thoracic conditions.
What are examples of life threatening thoracic conditions?
Airway obstruction
Tension pneumothorax
Massive haemothorax
Open pneumothorax
Flail chest segment with pulmonary contusion
Cardiac tamponade.
Flail chest, tracheal deviation, penetrating injuries, and bruising can be recognized by inspection.
Subcutaneous emphysema can be recognized by palpation.
Tension pneumothorax and haemothorax can be recognized by percussion and auscultation.
Circulation with hemorrhage control
What are the causes of preventable deaths after trauma?
Hemorrhage is the predominant cause of preventable post-injury deaths. Hypovolemic shock is caused by significant blood loss. Two large-bore intravenous lines are established and crystalloid solution may be given. If the person does not respond to this, type-specific blood, or O-negative if this is not available, should be given. External bleeding is controlled by direct pressure. Occult blood loss may be into the chest, abdomen, pelvis, or from the long bones.
Disability/Neurologic assessment
How do you do a quick neurological assessment in trauma cases?
During the primary survey, a basic neurological assessment is made, known by the mnemonic AVPU (alert, verbal stimuli response, painful stimuli response, or unresponsive). A more detailed and rapid neurological evaluation is performed at the end of the primary survey. This establishes the patient's level of consciousness, pupil size and reaction, lateralizing signs, and spinal cord injury level.
The Glasgow Coma Scale is a quick method to determine the level of consciousness, and is predictive of patient outcome, if not done in the primary survey.
What should you do if there is altered level of consciosuness?
An altered level of consciousness indicates the need for immediate reevaluation of the patient's oxygenation, ventilation, and perfusion status. Hypoglycemia and drugs, including alcohol, may influence the level of consciousness. If these are excluded, changes in the level of consciousness should be considered to be due to traumatic brain injury until proven otherwise.
Exposure and environmental control
How should you cover the patient?
It is imperative to cover the patient with warm blankets in the emergency department to prevent hypothermia. Intravenous fluids should be warmed and a warm environment maintained. Patient privacy should be maintained.
Resuscitation Fluids
IV Fluids
What are IV fluids?
What are the advantages and risks of this procedure?
Venipuncture procedure
Secondary survey
What is included in a secondary survey?
When the primary survey is completed, resuscitation efforts are well established, and the vital signs are normalizing, the secondary survey can begin. The secondary survey is a head-to-toe evaluation of the trauma patient, including a complete history and physical examination, including the reassessment of all vital signs. Each region of the body must be fully examined. X-rays indicated by examination are obtained. If at any time during the secondary survey the patient deteriorates, another primary survey is carried out as a potential life threat may be present. The person should be removed from the hard spine board and placed on a firm mattress as soon as reasonably feasible as the spine board can rapidly cause skin breakdown and pain while a firm mattress provides equivalent stability for potential spinal fractures.
Tertiary survey
What is included in a tertiary survey of trauma cases?
A careful and complete examination followed by serial assessments help recognize missed injuries and related problems, allowing a definitive care management. The rate of delayed diagnosis may be as high as 10%. Since emergency physicians, Physician surgeon medical emergency, Physician medical emergency responder, paramedics and other advanced practitioners use ATLS as their model for trauma care it makes sense that programs for other providers caring for trauma would be designed to interface well with ATLS.
What should people know about trauma?
What should a medical doctor, nurse, paramedic, or counselor know about trauma?
What should a police officer or military officer know about trauma?
How should you evaluate a medical doctor regarding skills and knowledge of diagnosis and treatment of trauma?
Annotation or Definition
Causes
Case scenario
Complications
Diagnostic tests
Diagnosis
Disabilities associated with this medical condition
Emergencies associated with this medical condition
Epidemiology
Glossary.
Healthcare Professionals (Trauma & Surgical Critical Care)
History of this medical condition
Medical history relevant to this medical condition
Mechanism or pathogenesis
Normal values
Prevention
Relevant anatomy, physiology, biochemistry
Risk factors
Research
Symptoms and signs
Types
Treatment or management
What is advanced trauma life support?
If you get an emergency call of emergency physical trauma, you first have to engage in advanced trauma life support. Based on the findings, surgical intervention may or may not be required.
Questions you need to answer
What are the details of the location of injury of this individual?
_________________________
Has there been trauma in the past few minutes?
_________________________
Is there a history of trauma within a few minutes or hours?
_________________________
How much time has elapsed from the start of the emergency until now?
_________________________
What is the cause of trauma?
_________________________
Is trauma due to road traffic crash, assault, fall, or other cause?
_________________________
If patient is able to talk, this is one of proof of airway patency and normal higher brain functions.
A few more questions need to be asked to verify these findings.
Has there been unconsciousness in the past few minutes?
_________________________
If yes, go ahead with on the spot diagnosis and treatment.
Do not delay in diagnosis and treatment.
Do on-the-spot diagnosis and treatment.
Do not wait for transfer of patient from the location of the medical emergency to a medical emergency room.
What are the vital signs of this patient at this point?
Date/time/location:
Vitals: normal/abnormal.
Verified by:
_________________________
What best describes the injury after physical trauma?
Fracture.
Incisional wound.
Tissue laceration.
Hematoma.
Internal bleed.
Neuro deficit.
Penetrating wound.
Amputation.
If other specify.
_________________________
What part of the human body of this individual has suffered from physical trauma?
_________________________
What were the causes and circumstances of this physical trauma?
_________________________
Does this case need surgical intervention?
_________________________
If so, what type of surgical intervention does this case need?
_________________________
Are there any obvious injuries? What are they?
_________________________
Where was patient when the injuries occurred?
_________________________
1. inside other building ______________________________________
2. outdoor location ___________________________________________
3. unknown
Date of first E.R. Visit ____/____/____ Arrival Time :______________
How did patient get to hospital?
_________________________
1. ambulance (name ____________________________)
2. private vehicle
3. public transportation
4. walked or was carried
5. helicopter
6. other (specify________________________________)
7. unknown
Was the patient transported from another health care facility?
_________________________
Y/N Unknown
If yes, specify: ________________________________________
Disposition from Emergency Department
1. discharged home
2. admitted
3. transferred to other facility (specify _________________________________________)
4. left against medical advice
5. dead on arrival
6. expired in emergency department
8. other
(specify___________________________________________)
9. unknown
If patient was admitted:
Date of Admission ____/____/____ Date of Discharge/Death ____/____/____
Discharge Disposition:
1. home
2. acute care hospital _____________________________
3. skilled nursing facility __________________________
4. intermediate care facility ________________________
5. other hospital ___________________________________
6. home health care
7. left against medical advice
8. expired in hospital
9. other _________________________________________
10. unknown
How did injury occur:
Injury Report Form
Are long-term physical disability/sequelae likely?
_________________________
___definite
___likely
___unlikely
___unknown
If so, what type of disability?
___neurologic
___physical
___hearing
___vision
___ other
|
What are usually surgical interventions after physical trauma?
_________________________
What are various types of trauma?
Physical trauma.
Sexual trauma.
Emotional trauma.
Sexual and emotional trauma have separate treatments.
Physical and sexual trauma have delayed sequel of emotional trauma.
Sexual and/or emotional trauma can occur without physical trauma.
On February 18, 2014, I received an update about sexual, physical, and emotional trauma.
Advanced trauma life support is for physical trauma assessment and treatment.
Sexual and emotional trauma has separate guidelines.
Advanced Trauma Life Support
Primary survey
Airway maintenance with cervical spine protection
Breathing and ventilation
Circulation with hemorrhage control
Disability/Neurologic assessment
Exposure and environmental control
Secondary survey
Tertiary survey
See also
Advanced Cardiac Life Support
Advanced Life Support
Basic Life Support
|
Trauma
Annotation or Definition
|
Causes
What causes trauma?
|
Case scenario
|
Complications
What complications can occur?
What are the complications or effects of physical trauma and psychological trauma?
How do traumatic experiences affect people?
What do trauma survivors need to know?
What are the common effects of trauma?
What are common secondary and associated posttraumatic symptoms?
|
Diagnostic tests
What are various diagnostic tests for trauma?
How is the test done?
What kind of information will the test provide?
Is this test the only way to find out that information?
What are the risks and benefits of having this test?
How accurate is the test?
What do I need to do to prepare for the test?
Will the test be uncomfortable?
How long will it take to get the results, and how will I get them?
What's the next step after the test?
What can you do?
What about the test results?
| |
Functional Assessment
|
When can a patient recover from medical condition at home?
If consciousness, pulse, blood pressure, temperature, respiratory rate, behavior, and mobility relevant to age are normal without any acute external or internal injury, and proper survival and civilized conditions exist at home, the patient can recover from the medical condition at home.
| |
Complete Blood Count (CBC)
| |
RADIOLOGY
| |
Death Investigation
|
|
Diagnosis
How should you do on-the-spot diagnosis and treatment of a trauma patient?
Here are further guidelines.
Factors with post-traumatic, depressive, crisis, or similar consequences.
Glasgow Coma Scale
Eyes
Verbal
Motor
How do you evaluate and diagnose a patient with physical trauma and psychological trauma?
| |
Disabilities associated with this medical condition
|
Emergencies associated with this medical condition
Are all trauma cases medical emergencies?
When is trauma a medical emergency?
|
Epidemiology
How many such cases occur worldwide every year?
How many trauma cases have been reported in 2012 worldwide?
How many cases of trauma have been reported in 2010 in your state?
|
Healthcare Professionals (Trauma & Surgical Critical Care)
What should people know about trauma?
What should a medical doctor, nurse, paramedic, or counselor know about trauma?
What should a police officer or military officer know about trauma?
How should you evaluate a medical doctor regarding skills and knowledge of diagnosis and treatment of trauma?
Here are further guidelines.
|
History of this medical condition
How has diagnosis and treatment of this medical condition evolved?
How did the diagnosis and treatment of trauma evolve?
As a matter of fact, advanced trauma life support did not exist up to 1976.
|
Medical history relevant to this medical condition
What medical history should you seek relevant to this issue?
Is there potential for improvement in the care of injured patients?
Injury Description Table
|
Mechanism or pathogenesis
What happens in this medical condition?
|
Normal values
When can a person be declared normal after a trauma?
When can a patient recover from medical condition at home?
If consciousness, pulse, blood pressure, temperature, respiratory rate, behavior, and mobility relevant to age are normal without any acute external or internal injury, and proper survival and civilized conditions exist at home, the patient can recover from the medical condition at home.
|
Prevention
How can trauma be prevented?
Here are further guidelines.
|
Relevant anatomy, physiology, biochemistry
What human body anatomy, physiology, and biochemistry should you know that is relevant to trauma?
|
Risk factors
What are risk factors for trauma?
| |
|
Research
What research is being done on this issue?
How can I help?
How can you help?
|
Symptoms and signs
How is this medical condition reported?
What should happen before reporting this medical condition?
What are the symptoms and signs of trauma?
Victims usually do not report this medical condition.
Others report this medical condition.
|
TypesWhat are the types of this medical condition?
What are the types of trauma?
What are the types of traumas and abuses?
Here are further guidelines.
|
Treatment or management
What are various treatment options?
Treat the underlying cause.
What is the best setting or location to treat this medical condition?
Do on-the-spot treatment as described.
Shift to ER or ICU after the on-the-spot treatment.
Treatment or management
How is trauma treated?
What are the criteria for admission to hospital for a trauma patient?
Treatment of trauma depends on the severity of the injury and diagnosis after proper evaluation.
Here are guidelines for treating trauma.
Any problem with airway, breathing, or circulation needs on-the-spot diagnosis and treatment.
Any fracture that is not open, and without loss of alignment, needs hospital emergency department diagnosis and treatment.
This does not need admission to the hospital.
Any fracture that is open, with loss of alignment, needs hospital admission.
Fixing the fracture depends on the type and location of the fracture.
The Golden Hour is a term used to describe the first hour immediately following a serious injury. If a patient receives proper medical care in that first hour, his chances of survival triple and the long-term side effects of injury are significantly decreased. This is one of the reasons distance between the scene of an accident and a trauma center as well as rapid response on the part to a trauma center following a severe injury, the chances for recovery diminish.
| |
Airway
| |
Airway
| |
Airway: Management
|
ASSESSING HYPOVOLAEMIA
RATE OF FLUID ADMINISTRATION
FLUID BOLUS (WHEN AND HOW MUCH)
| |
Fluid resuscitation
| |
Wound cleaning
| |
Infection control
| |
Nutritional support
| |
Surgical wound care - open
| |
Caring for Your Incision After Surgery
| |
Casts and Splints
| |
Cast Care
| |
Postures and Direction of Movement
|
Cardiopulmonary Resuscitation (CPR)
When is CPR important?
What happens during CPR?
What happens if CPR isn't done?
What are the benefits of CPR?
What are the risks of CPR?
How do I learn CPR?
| |
Hemorrhage control
| |
Resuscitative thoracotomy
| |
The Effects of Trauma
| |
Trauma And Orthopedics
| |
Trauma Emergencies
|
Common orthopaedic trauma emergencies
Common accompanying complications
Tips for management
Improve your care of the trauma patient
| |
Head trauma | |
Suspected spinal injury | |
Rapid Sequence Intubation | |
Traumatic brain injury | |
Sexual assault (rape) | |
The ATLS Program
| |
Child Abuse
| |
Initial Trauma Review
| |
BLS
| |
Cardiac Emergencies
| |
ACLS
| |
Trauma Counseling
|
Traumatic Brain Injury
Road traffic crash
Road Traffic Sabotage
What are examples of road traffic sabotage in the state or outside the state?
These examples will make you understand.
In 1985, in Lalbazar Srinagar, Kashmir, Asif Qureshi was asked to take an  vehicle. vehicle.
The vehicle was sabotaged in such a manner that when the vehicle is driven half a mile, the clutch, steering block, and steering will disassemble in such a manner that the  will be hit on the chest. will be hit on the chest.
This is what happened. Asif Qureshi was traumatized, but survived.
This criminal conspiracy was done while arranging a specific mechanic who does this type of sabotage with others.
In Medina in 1998, Doctor Asif Qureshi was asked to take a vehicle with some individuals for spiritual prayers at a Medina mosque.
Behind the scenes, an oil tanker was kept ready to bang Doctor Asif Qureshi and others in the vehicle.
It was discovered later on that such sabotage has been planned while asking him to go to a mosque at Medina, behind which the oil tanker was placed to do harm.
Harms occurred; however, Doctor Asif Qureshi survived.
What was the motive of saboteurs and criminal conspirators in these situations?
They were politically motivated criminal conspiracies.
Questions that remain unanswered.
Were the saboteurs arrested and punished?
Did the system make other aware such sabotage occurred and how to prevent such sabotage harms?
What did the system do to prevent, punish such sabotage and harms, and give relief to victims?
What are the recommendations?
Every road traffic crash is a criminal investigation unless proven otherwise.
Punishments to saboteurs and conspirators must go ahead.
Relief to victims must go ahead.
If you survived road traffic sabotage, an air crash can happen due to sabotage, criminal activities.
Here are further guidelines.
Case report of blood alcohol concentration in an emergency room
If blood alcohol concentration results in an emergency room are greater than expected, what should an emergency room physician do?
Here is a case report.
This case report will make you understand.
This happened in Chicago, Illinois, North America, before the year 2004.
A person had never consciously consumed alcohol because of being religious Muslim.
Suddenly, he had an accident. There was no injury but he felt something was wrong and he needed to go to a medical emergency room. He was taken to Swedish Covenant Hospital in Chicago, Illinois.
In the medical emergency room, his blood tests show a high concentration of alcohol.
What negligence was the emergency physician guilty of?
He did not ask him these questions.
He did not verify answers to these questions.
Do you consume alcohol?
No.
Have you ever consciously consumed alcohol?
No.
How did alcohol concentration come up in his blood?
Here are further facts.
Before taking a vehicle, he asked for a glass of water from a restaurant while having a meal near Swedish Covenant Hospital.
Instead of giving him water he was intentionally given alcohol by others so that sabotage occurred and he was harmed. Sabotage occurred due to the accident.
He had never consciously consumed alcohol.
This was a scenario of intentional harms and sabotage against him.
The emergency room physician should have reported this as medicolegal case and that the patient was a victim of sabotage.
What is the best scenario about this case?
The victim or patient in this case was himself an emergency room specialist with seven years of hospital experience at that point.
Here are further guidelines.
|
|
Glossary.
ABCDEFGHIJKLMNOPQRSTUVWXYZ.
A
Abduction
Movement of a part away the midline. related terms
.
ABI: ankle-brachial index
.
Absolute stability
Fixation of fracture fragments so that there is virtually no displacement of the fracture surfaces under physiological load. This allows direct bone healing. related terms
.
ACDF: anterior cervical discectomy and fusion
.
ACL: anterior cruciate ligament
related terms
.
ACT: autogenous chondrocyte transplantation
related terms
.
Adduction
Movement of a part towards the midline.
related terms
.
AFN: antegrade femoral nail
related terms
.
Aiming device
A device to guide a wire or drill bit in the correct direction.
related terms
.
ALARA: as low as reasonably achievable
ALARA is a principle in radiation protection. .Allograft
Bone or tissue transplanted from one individual to another individual of the same species. related terms
.Anatomical position
The reference position of the body: standing facing the observer, with the palms of the hands facing forward. related terms
.Anatomical reduction
Reinstatement of the exact prefracture shape of the bone. related terms
.
Anchor screw
A screw that serves as a point of fixation to anchor a wire loop, strong suture, or instrument (eg, articulated compression device). .Ankylosis
Fusion of a joint by bony or a tight fibrous union, occurring spontaneously as a result of a disease process, eg, following septic arthritis. .Antibiotic
Any drug or naturally occurring substance, which can inhibit the growth of or destroy microorganisms. .Antiglide plate
Prevents shear displacement of a fragment by functioning as a buttress. Classically, it is only fixed to one main fragment. related terms
.AO: Arbeitsgemeinschaft für Osteosynthesefragen
The AO Foundation, is a medical non-profit organization with international research and educational activities led by surgeons specialized in trauma, spinal, craniomaxillofacial, and veterinary surgery. Its mission is to foster and expand its network of healthcare professionals in education, research, development, and clinical investigation to achieve more effective patient care worldwide. Founded in 1958, the AO today represents the world’s leading knowledge organization in this field. It comprises one of the most important and extensive networks in medicine with more than 10,000 surgeons, and an international faculty of over 3,000 experts in more than 100 countries. .AP: anteroposterior
.APC: anodic plasma-chemical treatment
.APL: abductor pollicis longus
related terms
.APTT: activated partial thromboplastin time
.ARDS: adult respiratory distress syndrome
.ARR: absolute risk reduction (or increase)
related terms
.
Arthritis
An inflammatory condition of a synovial joint. It may be septic or aseptic. .Arthrodesis
Fusion of a joint by bone as a planned outcome of a surgical procedure. .Articular fracture, complete
The entire articular surface is separated from the diaphysis. related terms
.Articular fracture, multifragmentary-depression
A fracture in which part of the joint is depressed and the fragments are completely separated. related terms
.Articular fracture, partial
Only part of the joint is involved in the fracture, while the remainder remains attached to the diaphysis. There are several varieties. related terms
.Articular fracture, pure depression
An articular fracture in which there is depression of the articular surface alone without split. The depression may be central or peripheralâ€â€see impacted fracture. related terms
.
Articular fracture, pure split
An articular fracture in which there is a longitudinal metaphyseal and articular split, without any additional osteochondral lesion. related terms
.Articular fracture, split-depression
An articular injury with a fracture line running into the metaphysis (split) and impaction of separate osteochondral joint fragments (depression). related terms
.ASA: acetylsalicylic acid
.ASIA: American spinal injury association
.ATLS: advanced trauma life support
.Autograft
A graft of tissue from one site to another within the same individual. related terms
.Avascular necrosis (AVN)
Bone which has been deprived of its blood supply dies. In the absence of sepsis, this is called avascular necrosis. The dead bone retains its normal strength (although it is unable to heal) until the natural process of revascularization, by creeping substitution, starts to remove the dead bone, in preparation for the laying down of new bone. Loaded areas may then collapse. .AVN: avascular necrosis
Bone which has been deprived of its blood supply dies. In the absence of sepsis, this is called avascular necrosis. The dead bone retains its normal strength (although it is unable to heal) until the natural process of revascularization, by creeping substitution, starts to remove the dead bone, in preparation for the laying down of new bone. Loaded areas may then collapse. .Avulsion
Pulling off. A bone fragment pulled off by a ligament or muscle attachment is an avulsion fracture. .B
Bactericidal
Capable of killing bacteria. .BCP: biphasic calcium phosphate
related terms
.Bending stiffness
The bending stiffness of an intramedullary nail is inversely proportional to the square of the working length. related terms
.Bicortical screw
A screw that purchases in both the near cortex and the far cortex. related terms
.Biocompatibility
The ability to exist in harmony with, and not to injure, associated biological tissues or processes. .Biological internal fixation
A technique of careful surgical exposure, fracture reduction, and fixation, which favors the preservation of the blood supply of the fracture site and, thereby, optimizes the healing potential of the bone and soft tissues. .BMC: bone mineral content
related terms
.BMD: bone mineral density
related terms
.BMP: bone morphogenic protein
.
Bone graft
Bone removed from one skeletal site and placed at another. Bone grafts are used to stimulate bone union and also to restore skeletal continuity where there has been bone loss see allograft, autograft, and xenograft. related terms
.
Bone resorption
Removal of bone by osteoclasts. This is an integral element of bone remodeling either during growth or after fracture. Pathological removal of bone by activated osteoclasts and giant cells occurs if bone is dead, when bone is infected, and around implants where there is excessive movement. .Bone substitute
Nonosseous biological or inorganic material that can be used in place of, or to augment, bone graft to fill a defect or to support unfractured bone. .Bridging plate
A plate which spans the fracture site and is attached to each main fragment of a multifragmentary fracture maintaining axial and rotational alignment and length. It is not fixed to nor does it disturb the blood supply of intervening fragments. more detail related terms
.BSSO: bilateral sagittal split osteotomy
.Butterfly fragment
Where there is a fracture complex with a third fragment which does not comprise a full cross section of the bone (ie, after reduction there is some contact between the two main fragments), the wedge-shaped fragment, which due to a rotation mechanism may be spiral, is occasionally referred to as a butterfly fragmentâ€â€see wedge fracture. .Buttress
A construction that resists axial load by applying force at 90° to the axis of potential deformity. related terms
.C
C-clamp: compression clamp (for pelvis)
related terms
.Calcar
(Latin = spur) The medial cortex of the femoral neck, proximal to the lesser trochanter, which transmits the majority of compressive force generated in the femoral neck during load bearing. .Callus
A tissue of immature bone and cartilage that is formed at the site of bony repair to bridge a fractureâ€â€see healing, indirect. related terms
.Cancellous bone
Spongy trabecular bone, found mostly at the proximal and distal bone ends. related terms
.CAOS: computer-assisted orthopedic surgery
related terms
.CaP: calcium phosphate
related terms
.CAS: computer-assisted surgery
related terms
.CDMP: cartilage derived morphogenic protein
related terms
.CE: Conformité Européenne
.CER: control event rate
related terms
.CFN: cannulated femoral nail
related terms
.Chondrocytes
The active cells of cartilage which produce type II collagen and proteoglycans that make up the chondral matrix. related terms
.CME: continuing medical education
.CNS: central nervous system
.
Coating
A thin layer that is applied to the surface of an implant and which may contain different agents (eg, antibiotics, or bone morphogenic protein). .CoE: classes of evidence
.Combination hole
The plate hole of the locking compression plate (LCP) that consists of two parts: the nonthreaded dynamic compression unit (DCU; shaped like the holes of a dynamic compression plate (DCP)), and the threaded part which has a reciprocal thread for the insertion of a locking head screw (LHS). more detail related terms
.Compartment syndrome
Raised pressure in a closed fascial compartment that results in painful local tissue ischemiaâ€â€see muscle compartment, ischemia-reperfusion injury. more detail related terms
.Complete articular fracture
The entire articular surface is separated from the diaphysis. related terms
.Complex fracture
A fracture with one or more intermediate fragment(s) in which there is no contact between the main fragments after reductionâ€â€see multifragmentary fracture. related terms
.Complex regional pain syndrome (CRPS)
Neuropathic pain with associated sudomotor and vasomotor disturbances that develops after trauma, another inciting event, or a period of immobilization. The diagnostic criteria are broad and there are no specific tests for the diagnosis of this condition. There are two types (CRPS I and CRPS II) that have the same signs and symptoms, the difference being that an identifiable nerve lesion is associated with CRPS II. CRPS is also known under different names: fracture disease, algodystrophy, reflex sympathetic dystrophy, Sudeck’s atrophy. .Compression
The act of pressing together to increase or achieve stability. related terms
.Compression, interfragmentary
Bone fragments are pressed together, either with a lag screw or plate, to produce absolute stability. related terms
.Contact healing
One form of direct bone healing, which occurs between two fragments of bone maintained in motionless contact (absolute stability). The fracture is repaired by direct internal remodeling. related terms
.Continuous passive motion (CPM)
The use of an apparatus providing periods of passive movement of a joint through a controlled range of motion. .Conventional screw
Any screw with a smooth outer surface of the head (ie, without threads) that is used for fracture or plate fixation. more detail related terms
.Coronal plane
The vertical plane of the body passing from side to side, so that a coronal bisection of the body would cut it into a front half and a back half. Also called the frontal plane. related terms
.Corrosion
This is an electrochemical process that results in the destruction of metal by the liberation of ionic metal. .Cortical bone
The dense bone forming the tubular element of the shaft, or diaphysis (middle part), of a long bone. The term is also applied to the dense, thin shell covering the cancellous bone of the metaphysis. related terms
.Corticotomy
A special osteotomy where the cortex is surgically divided but the medullary content and the periosteum are not injured. related terms
.Countersink
The process of making a shallow recess around a screw hole to increase the contact area between the bone and the screw head. The term can also refer to the tool for making such a recess. related terms
.CPM: continuous passive motion
The use of an apparatus providing periods of passive movement of a joint through a controlled range of motion. .CPM: continuous passive motion
The use of an apparatus providing periods of passive movement of a joint through a controlled range of motion. .cpTi: commercially pure titanium
related terms
.
Creeping substitution
The slow replacement of dead bone with living, vascular bone. related terms
.CRIF: closed reduction internal fixation
related terms
.Critical strain level
The strain level at which a tissue disrupts or ceases to perform its normal physiological function. related terms
.CRP: C-reactive protein
.CRPS I: complex regional pain syndrome type I
related terms
.CRPS II: complex regional pain syndrome type II
related terms
.CRPS: complex regional pain syndrome
Neuropathic pain with associated sudomotor and vasomotor disturbances that develops after trauma, another inciting event, or a period of immobilization. The diagnostic criteria are broad and there are no specific tests for the diagnosis of this condition. There are two types (CRPS I and CRPS II) that have the same signs and symptoms, the difference being that an identifiable nerve lesion is associated with CRPS II. CRPS is also known under different names: fracture disease, algodystrophy, reflex sympathetic dystrophy, Sudeck’s atrophy. .CSF: cerebrospinal fluid
.CSLP: cervical spine locking plate
related terms
.CTA: computed tomography angiography
related terms
.CTN: cannulated tibial nail
related terms
.D
DAD: distal aiming device (for tibial nail)
related terms
.Damage-control surgery (DCS)
Rapid emergency surgery to save life and/or limb, while avoiding time-consuming and potentially traumatic definitive fracture fixation. DCS usually involves hemorrhage control, wound debridement, and the application of temporary external fixators rapidly to stabilize long-bone fractures and unstable fracture dislocations. related terms
.DBM: demineralized, lyophilized bovine bone graft
related terms
.dBP: diastolic blood pressure
.DCP: dynamic compression plate
A plate with chamfered oval holes through which eccentrically placed screws can be inserted to provide compression across a fracture site. more detail related terms
.DCS: damage-control surgery
Rapid emergency surgery to save life and/or limb, while avoiding time-consuming and potentially traumatic definitive fracture fixation. DCS usually involves hemorrhage control, wound debridement, and the application of temporary external fixators rapidly to stabilize long-bone fractures and unstable fracture dislocations. related terms
.DCS: dynamic condylar screw
.DCU: dynamic compression unit
The nonthreaded part of a LCP combination hole that is shaped like the hole of a dynamic compression plate (DCP). related terms
.DDD: degenerative disc disease
.Debridement
The surgical excision from a wound injury zone or pathological area, of foreign material and all avascular, contaminated, and infected tissue. related terms
.Deformation, elastic
A temporary change in length or angle of a material that will recover its former state when the deforming force is released. related terms
.Deformation, plastic
A change in length or angle of a material that is permanent and will not recover when the deforming force is released. related terms
.Deformity
Any abnormality of the form of a body part. .Delayed union
Fracture healing is not taking place at what is accepted as the expected time course for a particular fracture (and the patient’s age)â€â€see nonunion. related terms
.DFN: distal femoral nail
related terms
.DHS: dynamic hip screw
related terms
.Diaphysis
The cylindrical or tubular part between the ends of a long bone, often referred to as the shaft. related terms
.
Diastasis screw
A position screw that is placed between the fibula and tibia to maintain their normal anatomical relationship at the distal tibiofibular syndesmosis. The screw must gain purchase in both bones as compression must not be applied. related terms
.DICOM: digital imaging and communications in medicine
related terms
.Direct healing
It is observed following internal fixation with absolute stability. It is characterized by the absence of callus; there is no resorption at the fracture site. Bone forms by internal remodeling without intermediate repair tissue. Direct fracture healing was formerly called primary healing. related terms
.Direct reduction
Hands or instruments manipulate fracture fragments under direct vision. related terms
.Dislocation
A displacement of a joint such that no part of one articular surface remains in contact with the other. Sometimes used incorrectly to denote fracture displacement. related terms
.Displacement
The condition of being out of place. A fracture is displaced if the fragments are not perfectly anatomically aligned. related terms
.Distal
Away from the center of the body, more peripheral. .Distraction osteogenesis
The induction of bone formation by the application of tension to soft tissue that has the potential to form bone, eg, organized hematoma, periosteum, and endosteum at the site of an osteotomy or osteoclasis. This phenomenon was first described by Bier (1927) and scientifically investigated by the Russian surgeon Ilizarov. related terms
.DMB: demineralized bone matrix
related terms
.Dorsal
Pertaining to the backâ€â€or dorsumâ€â€of the body in the anatomical position. An exception is the foot; the top of the foot, even though it faces forward in the anatomical position, is called the dorsum. Dorsal is only used to describe the dorsum of the hand and foot. For all other parts the terms “anterior†and “posterior†are used. related terms
.DRUJ: distal radioulnar joint
related terms
.
Ductility
The degree of permanent (plastic) deformation a material tolerates before it breaks. The ductility of a material determines the degree to which an implant, such as a plate, can be contoured without breaking. related terms
.DVT: deep vein thrombosis
related terms
.DVT: digital volume tomography
related terms
.DXA: dual x-ray absorptiometry
related terms
.Dynamic compression plate (DCP)
A plate with chamfered oval holes through which eccentrically placed screws can be inserted to provide compression across a fracture site. more detail related terms
.Dynamic compression unit (DCU)
The nonthreaded part of a LCP combination hole that is shaped like the hole of a dynamic compression plate (DCP). related terms
.Dynamic locking
When an interlocking screw is placed into the oval hole of an intramedullary nail, this controls rotation and alignment, but allows some (controlled) impaction of the fracture during weight bearingâ€â€see dynamization. related terms
.Dynamization
Diverting the mechanical load from a fixation de vice to load the fracture site in order to enhance bone formation. .E
Early total care (ETC)
Definitive treatment in polytrauma of all injuries, including major long-bone fractures, within 24 hours of injury. related terms
.EBL: estimated blood loss
.EBOS: evidence-based orthopaedic surgery
.EER: eperimental event rate
related terms
.EGF: epithelial growth factor
related terms
.EHN: expert humeral nail
related terms
.Elastic deformation
A temporary change in length or angle of a material that will recover its former state when the deforming force is released. related terms
.EMG: electromyogram
.End segment
This term has been created for the AO classification of articular fractures in the adult. It is defined by drawing a line across the widest part of the metaphysis on an x-ray. This line is then used to create a square and one line is placed along the articular surface. The bone lying within the square is defined as the end segment. In children, the end segment is further divided into epiphysis and metaphysis which are separated by the growth plate. related terms
.
Endosteum
A single layered membrane that lines the interior surface of the bone ie, the wall of the medullary cavity. Its cells have osteogenic potential. related terms
.Energy transfer
When tissues are injured, the damage is due to energy that is transferred to the tissues. This is most commonly due to the transfer of kinetic energy from a moving object (car, missile, falling object, etc) but can also be due to thermal energy. related terms
.ENT: ear, nose and throat
.EPB: extensor pollicis brevis
related terms
.Epiphysis
The end of a long bone which bears the articular component. The epiphysis develops from the cartilaginous element between the joint surface and the growth plateâ€â€see metaphysis. related terms
.EPL: extensor pollicis longus
related terms
.ERG: electroretinogram
related terms
.ESIN: elastic stable intramedullary nailing
.ESR: erythrocyte sedimentation rate
.ETC: early total care
Definitive treatment in polytrauma of all injuries, including major long-bone fractures, within 24 hours of injury. related terms
.ETNS: expert tibial nail system
related terms
.Evidence-based medicine
Using the strength or robustness of scientific investigation to make clinical decisions. The strength of clinical evidence is based on the strength of studies, for example, reports of case series are weak and a randomized prospective trial is strong. related terms
.External fixation
Skeletal stabilization using pins, wires, or screws that protrude through the skin and are linked externally by bars or other devices. related terms
.Extraarticular fracture
The fracture does not involve the articular surface but is within the end segment of a long bone and may be within the joint capsule. related terms
.F
FA: facial artery
.Far cortex
The cortex more distant from the operatorâ€â€see near cortex. related terms
.Fasciocutaneous flaps
Soft-tissue flaps, based upon a perforating artery, which include the skin, the subcutaneous tissues, and the deep fascia. .Fasciotomy
The surgical division of the wall of a muscle compartment, usually to release high intracompartment pressure see compartment syndrome. related terms
.Fatigue failure
If any material is subjected to multiple loading cycles, it may develop microscopic cracks and eventually fail at a stress well below the tensile strength, and often below the yield strength of the pristine material. related terms
.FCR: flexor carpi radialis
related terms
.FCU: flexor carpi ulnaris
related terms
.FDA: Food and Drug Administration
.FES: fat embolism syndrome
.FGF: fibroblast growth factor
related terms
.Fibrocartilage
Tissue consisting of elements of cartilage and of fibrous tissue. It is the normal constituent of the menisci and the triangular fibrocartilage at the wrist. It forms as the repair tissue after injury to articular cartilage. related terms
.Fixed-angle device
An implant with two or more parts that are solidly connected at an angle so that it will resist forces tending to angulate one part with respect to the other. Such devices are used to prevent angular displacement of fractures. Fixed-angle devices may be manufactured as a single, solid device, eg, 95° angled blade plate, or produced by mechanically coupling two implants, eg, a locking compression plate with a locking head screw. related terms
.FN: facial nerve
.FPL: flexor pollicis longus
related terms
.Fracture disease
A condition characterized by disproportionate pain, soft-tissue swelling, patchy bone loss, and joint stiffness see type II complex regional pain syndrome. related terms
.Fracture fixation
Application of a mechanical device to a broken bone to allow healing in a controlled position and (usually) to facilitate early functional rehabilitation. The surgeon determines the degree of reduction required and the mechanical environment, which in turn influences the mode of bone healing. related terms
.
Fracture treatment, goal
According to Müller et al the goal of fracture treatment is to restore optimal function of the limb in respect to mobility and load-bearing capacity while avoiding complications. .Free vascularized graft/flap
Soft tissue and/or bone that is transplanted to a separate anatomical site in the same individual and revascularized using microsurgical techniques to attach its vascular pedicle to vessels at the recipient site. related terms
.FWB: full weight bearing
related terms
.G
Gap healing
One form of direct bone healing when there is absolute stability but a small gap between the fracture fragments. Lamellar bone forms in the gap and is then remodeled by penetrating osteons. related terms
.GCS: Glasgow coma scale
related terms
.GDF: growth and differentiation factor
related terms
.Glide hole
The cortex under the screw head is drilled to the size of thread diameter so that the thread gets no purchase. This is used for the lag screw technique. related terms
.Gliding splint
The linkages (couples) between the bone and the splinting device allow (controlled) axial movement, so that the distance between the couples can change (eg, dynamically locked nail). related terms
.Goal of fracture treatment
According to Müller et al the goal of fracture treatment is to restore optimal function of the limb in respect to mobility and load-bearing capacity while avoiding complications. .GOS: Glasgow outcome scale
related terms
.Guide wire
A wire inserted into bone to allow precise positioning of a cannulated drill, reamer, or implant that is passed over the wire. related terms
.H
HA: hydroxyapatite
.Haversian system
The cortical bone is composed of a system of small channels (osteons) about 0.1 mm in diameter. These channels contain the blood vessels and are remodeled after a disturbance of the blood supply to bone. There is a natural turnover of the Haversian system by continuous osteonal remodeling; this process is part of the dynamic and metabolic nature of bone. It is also involved in the adaptation of bone to an altered mechanical environment. related terms
.HDU: high dependency unit
related terms
.Healing
Returning to preinjury condition. Bone healing is regarded as complete when bone has regained normal stiffness and strength. related terms
.
Healing, contact
One form of direct bone healing, which occurs between two fragments of bone maintained in motionless contact (absolute stability). The fracture is repaired by direct internal remodeling. related terms
.Healing, direct
It is observed following internal fixation with absolute stability. It is characterized by the absence of callus; there is no resorption at the fracture site. Bone forms by internal remodeling without intermediate repair tissue. Direct fracture healing was formerly called primary healing. related terms
.Healing, gap
One form of direct bone healing when there is absolute stability but a small gap between the fracture fragments. Lamellar bone forms in the gap and is then remodeled by penetrating osteons. related terms
.Healing, indirect
Bone healing by callus formation in fractures treated either with relative stability or left untreated. related terms
.Heterotopic (ectopic) ossification (HTO)
Formation of new bone in soft tissues, secondary to trauma or other pathology. .HFS: Hanover fracture scale
related terms
.hGH: human growth hormone
.HMSC: human mesenchymal stem cells
related terms
.Hook plate
A plate that is bent so that it captures a fracture fragment which can then be reduced by applying tension to the plate. The hook can be part of a specially designed plate for a specific anatomical site, or improvised by cutting and bending a conventional plate. related terms
.HRT: hormone replacement therapy
.HTA: health technology assessment
.HTO: heterotopic (ectopic) ossification
Formation of new bone in soft tissues, secondary to trauma or other pathology. .HTO: high tibial osteotomy
related terms
.I
IAN: inferior alveolar nerve
.IASP: International Association for the Study of Pain
related terms
.ICBG: iliac crest bone graft
related terms
.ICP: intracranial pressure
related terms
.ICU: intensive care unit
.IGF-BP: insulin-like growth factor - binding proteins
related terms
.IGF: insulin-like growth factor
related terms
.IGS: image guided surgery
related terms
.IMF: intermaxillary fixation
related terms
.IMP: intramuscular pressure
related terms
.Impacted fracture
A fracture in which the opposing bone surfaces are driven into each other and behave as a single unit. This is a combined clinical and radiological diagnosis. related terms.
Indirect healing
Bone healing by callus formation in fractures treated either with relative stability or left untreated. related terms
.Indirect reduction
Fragments are manipulated by applying corrective forces at a distance from the fracture zone, by distraction or other means, without exposing the fracture site. related terms
.Injury severity score (ISS)
An anatomical scale that was developed to give a numerical value to the extent of trauma in patients with multiple trauma. The highest abbreviated injury scale (range 0–5) is calculated for a maximum of three systems (eg, head trauma, musculoskeletal trauma, abdominal injuries). Each abbreviated injury score is squared and the three squared scores added together to calculate the ISS (maximum = 3 x 5² = 75)â€â€see polytrauma. related terms
.INR: international normalized ratio
.Interfragmentary compression
Bone fragments are pressed together, either with a lag screw or plate, to produce absolute stability. related terms
.Interlocking screw
Also called (inter)locking bolt. It couples an intramedullary nail to the bone to maintain length, alignment, and rotation. related terms
.
Internal fixator
Mechanical device that is underneath the skin and bridges a fracture zoneâ€â€similar to external fixationâ€â€providing an angularly locked, extramedullary splint resulting in relative stability (eg, LCP, LISS). related terms
.Ischemia
Reduction in blood flow resulting in tissue hypoxia. related terms
.Ischemia-reperfusion injury
Prolonged tissue hypoxia results in the activation of superoxide enzymes which produce free oxygen radicals when the circulation is restored. These free radicals cause cell membrane damage resulting in increased permeability that may lead to cell swelling and edema. Ultimately, this can result in cell death and, in a closed anatomical compartment, compartment syndrome can be the outcome. more detail related terms
.ISS: injury severity score
An anatomical scale that was developed to give a numerical value to the extent of trauma in patients with multiple trauma. The highest abbreviated injury scale (range 0–5) is calculated for a maximum of three systems (eg, head trauma, musculoskeletal trauma, abdominal injuries). Each abbreviated injury score is squared and the three squared scores added together to calculate the ISS (maximum = 3 x 5² = 75)â€â€see polytrauma. related terms
.IVC: inferior vena cava
.J
JLCA: joint line convergence angle
.Joystick
A Schanz screw or threaded pin with an attached handle inserted into a fracture fragment to allow direct manipulation of the fragment to effect fracture reduction. related terms
.K
K-wire: Kirschner wire
related terms
.Kinetic energy
The energy stored by a body by virtue of the fact that it is in motion. Kinetic energy is calculated according to the formula E = ½ mv², where m is the mass of the moving object and v its velocity. related terms
.L
Lag screw
A screw that passes through a glide hole to grip the opposite fragment in a thread hole, producing interfragmentary compression when it is tightened. more detail related terms
.LC-DCP: limited contact dynamic compression plate
The limited-contact dynamic compression plate (LC-DCP) was introduced by Perren in 1990 and has become the gold standard for plate fixation. The plate is available in two sizes, 3.5 and 4.5 mm, which is determined by the thread diameter of the cortex screws used together with the plate. The screw hole design allows for axial compression by eccentric screw insertion. more detail related terms
.LCL: lateral canthal ligament
.LCL: lateral collateral ligament
related terms
.LCP: locking compression plate
See locking plate and internal fixator. related terms
.LD: lacrimal duct
.LDTA: lateral distal tibial angle
.LDUH: low-dose unfractionated heparin
related terms
.LG: lacrimal gland
.LHS: locking head screw
A screw with a thread cut into its head which provides a mechanical couple, or linkage, to a threaded screw hole in a plate, thereby creating a fixed-angle device. more detail related terms
.Ligamentotaxis
Traction is applied across a fractured joint so that tension in capsular and ligamentous attachments reduces fracture fragments. related terms
.Limited-contact dynamic compression plate (LC-DCP)
The limited-contact dynamic compression plate (LC-DCP) was introduced by Perren in 1990 and has become the gold standard for plate fixation. The plate is available in two sizes, 3.5 and 4.5 mm, which is determined by the thread diameter of the cortex screws used together with the plate. The screw hole design allows for axial compression by eccentric screw insertion. more detail related terms
.
Limited-contact plate
A plate designed to limit contact with the underlying bone which preserves the maximum possible periosteal blood supply. The most common variety is the limited-contact dynamic compression plate (LC-DCP). related terms
.LIPUS: low intensity pulsed ultrasound
.LISS: less invasive stabilization system
related terms
.LMWH: low-molecular weight heparin
related terms
.Locked splint
There is a fixed linkage (couple) between the bone and splinting device, above and below the fracture zone, so that the working length between the couples cannot change (eg, statically locked nail). related terms
.
Locking compression plate (LCP)
See locking plate and internal fixator. related terms.
Locking head screw (LHS)
A screw with a thread cut into its head which provides a mechanical couple, or linkage, to a threaded screw hole in a plate, thereby creating a fixed-angle device. more detail related terms
.Locking plate
A plate with threaded screw holes that allow mechanical coupling to a locking head screw (LHS). The less invasive stabilization system (LISS) will accept only this type of screw, while locking compression plates (LCPs) have a combination hole that will accept conventional screw heads or threaded screw heads. related terms
.LPFA: lateral proximal femoral angle
.M
MA: malar arch
.Malunion
The fracture has healed in a position of deformity. related terms
.MCL: medial canthal ligament
.MCL: medial collateral ligament
related terms
.MEFiSTO: monolateral external fixation system for traumatology and orthopedics
related terms
.MESS: mangled extremity severity score
related terms
.
Metaphysis
In the adult, this is the segment of a long bone located between the articular surface and the shaft. It consists mostly of cancellous bone within a thin cortical shell. related terms
.MFA: musculoskeletal function assessment
.Minimally invasive osteosynthesis (MIO)
Any fracture fixation undertaken using small skin incisions and designed to limit the deeper soft-tissue surgical trauma. Examples include percutaneous K-wiring and closed intramedullary nailing as well as minimally invasive plate osteosynthesis (MIPO). related terms
.Minimally invasive plate osteosynthesis (MIPO)
Reduction and fixation with a plate of any design, without direct surgical exposure of the fracture site, using small skin incisions and subcutaneous or submuscular insertion of the plate. .Minimally invasive surgery (MIS)
Any surgical procedure undertaken using small skin incisions. Examples include laparoscopic abdominal surgery, arthroscopy, and closed intramedullary nailing. .MIO: minimally invasive osteosynthesis
Any fracture fixation undertaken using small skin incisions and designed to limit the deeper soft-tissue surgical trauma. Examples include percutaneous K-wiring and closed intramedullary nailing as well as minimally invasive plate osteosynthesis (MIPO). related terms
.MIPO: minimally invasive plate osteosynthesis
Reduction and fixation with a plate of any design, without direct surgical exposure of the fracture site, using small skin incisions and subcutaneous or submuscular insertion of the plate. .MIPPO: minimally invasive percutaneous plate osteosynthesis
.MIS: minimally invasive surgery
Any surgical procedure undertaken using small skin incisions. Examples include laparoscopic abdominal surgery, arthroscopy, and closed intramedullary nailing. .MMA: methyl methacrylate
related terms
.MMF: mandibulomaxillary fixation
related terms
.MN: mental nerve
.MOdDAD: modular aiming device
related terms
.MODS: multiple organ dysfunction syndrome
related terms
.Modulus of elasticity
Ratio of stress to strain in the linear region of a stress-strain curve. Also called Young’s modulus. related terms
.MOF: multiple organ failure
related terms
.Monocortical screw
A screw that purchases only in the near cortex. related terms
.MPP: mean muscle perfusion pressure
related terms
.MPTA: medial proximal tibial angle
.MRC: Medical Research Council
.MRI: magnetic resonance imaging
related terms
.MRSA: methicillin-resistant Staphylococcus aureus
.MSC: mesenchymal stem cells
related terms
.Multifragmentary fracture
A fracture with more than one fracture line so that there are three pieces or moreâ€â€see complex fracture. related terms
.Multifragmentary-depression articular fracture
A fracture in which part of the joint is depressed and the fragments are completely separated. related terms
.
Muscle compartment
An anatomical space, bounded on all sides either by bone or deep fascia, which contains one or more muscle bellies. related terms
.MVA: motor vehicle accident
.N
NDI: neck disability index
.Near cortex
The cortex near the operator and on the side of insertion of an implant. related terms
.Neutralization (plate) refers to Protection (plate)
A plate, or other implant, which reduces the load placed upon a lag screw fixation, thus protecting it from overload. This term has replaced neutralization (plate). more detail related terms
.NLS: nasolacrimal sac
.NNT: number needed to treat/number neede to harm
related terms
.
Nonunion
The fracture is still present and healing has stopped. The fracture will not unite without surgical intervention. A nonunion is usually due to inadequate mechanical or biological conditions–see union, pseudarthrosis, and delayed union. related terms
.NSAIDs: nonsteroidal antiinflammatory drugs
related terms
.NVS: neurovascular structures
.O
OA: osteoarthritis
A degenerative condition of synovial joints which is characterized by loss of articular cartilage, subchondral bone sclerosis, bone cysts, and the formation of osteophytes. related terms
.OC: oral contraceptives
.OPG: orthopantomogram
related terms
.OR: operating room
related terms
.ORIF: open reduction and internal fixation
A widely used abbreviation for open reduction and internal fixation (osteosynthesis). related terms
.ORP: operating room personnel
related terms
.Orthosis
An external device that is applied to the body in order to protect and/or stabilize a body part, to prevent or correct scarring and deformities, or to aid movement. related terms
.Osteoarthritis
A degenerative condition of synovial joints which is characterized by loss of articular cartilage, subchondral bone sclerosis, bone cysts, and the formation of osteophytes. related terms
.
Osteoconduction
The physical property of a material that provides the microstructure for the ingrowth of cells that produce bone. related terms
.Osteogenesis
The formation of new bone from progenitor tissue. related terms
.Osteoinduction
The property of stimulating new bone formation (osteogenesis). related terms
.Osteomyelitis
An acute or chronic inflammatory condition affecting bone and its medullary cavity, usually the result of infection. related terms
.Osteon
The name given to the small channels which combine to make up the Haversian system in cortical bone. related terms
.Osteopenia
A reduction in bone mass of between 1 and 2.5 standard deviations below the mean for a young adult (ie, a T score of –1 to –2.5)â€â€see osteoporosis. related terms
.Osteoporosis
A reduction in bone mass of more than 2.5 standard deviations below the mean for a young adult (ie, a T score of < –2.5)â€â€see osteopenia and pathological fracture. related terms
.Osteosynthesis
A term coined by Albin Lambotte to describe the “synthesis†(derived from the Greek for making together or fusing) of a fractured bone by a surgical intervention using implants. It includes external fixation. related terms
.Osteotomy
Controlled surgical division of a bone. related terms
.OTA: Orthopaedic Trauma Association
.OTD: Orthopedic Trauma Directions
.
Overbending (of a plate)
An exactly contoured plate is given a slight extra bend at the level of a transverse fracture, so that its central portion stands slightly off the underlying cortex. As compression is applied by tensioning the plate, the far cortex is compressed first, then the near cortex, resulting in even compression across the transverse diameter of the bone. Without the overbend, the plate will only compress the near cortex, resulting in an unstable fixation and the risk of cyclical loading of the plate and eventual fatigue failure. related terms
.P
PACS: picture archiving and communication systems
related terms
.Partial articular fracture
Only part of the joint is involved in the fracture, while the remainder remains attached to the diaphysis. There are several varieties. related terms
.Pathological fracture
A fracture through abnormal bone which occurs at normal physiological load or stress. related terms
.PCA: patient-controlled analgesia
.PCL: polycaprolactone
.PCL: posterior cruciate ligament
related terms
.PDGF: platelet derived growth factor
related terms
.PDLLA: poly-D,L-lactide
related terms
.PDS: polydioxanone
.PE: pulmonary embolism
related terms
.PEEK: polyetheretherketone
related terms
.PEG: polyethylene glycol
related terms
.PEKK: polyetherketoneketone
related terms
.PEP: pulmonary embolism prevention
related terms
.Periosteum
The fibrovascular membrane covering the exterior surface of a bone. The deep cell layer has osteogenic potential. related terms
.Personality of the fracture
The term "personality" of the fracture was coined by EA. Nichol (1965) to express the combination of attributes of a fracture that determine its outcome after treatment. There are three key factors: the patient; the soft tissues; and the fracture itself. related terms
.PET: positron emission tomography
related terms
.PFN: proximal femoral nail
related terms
.PFNA: proximal femoral nail antirotation
related terms
.PGA: polyglycolic acid
related terms
.PHILOS: proximal humerus internal locked system
related terms
.PHN: proximal humeral nail
related terms
.Pilot hole
A drill hole which is the same diameter as the core of the screw. This can then be used to guide the insertion of screws that cut their own thread (self-tapping screw) or a tap that will cut the threads and produce a thread hole. related terms
.Pin loosening
Bone resorption at an external fixator pin-bone interface. related terms
.PISA-PED: prospective investigative study of acute pulmonary embolism diagnosis
PISA-PED prospective investigative study of acute pulmonary embolism diagnosis related terms
.PLA: polylactic acid
related terms
.Plastic deformation
A change in length or angle of a material that is permanent and will not recover when the deforming force is released. related terms
.Plate screw
Preload and friction is applied to create force between the plate and the bone. related terms
.PLGA: polyglycolides
related terms
.PLLA: polylactides
related terms
.PMMA: polymethylmethacrylate
related terms
.PMN: polymorphonuclear neutrophils
.POL: posterior oblique ligament
.
Poller screw
A screw used as a fulcrum to redirect an intramedullary nail. related terms
.Polytrauma
A syndrome of multiple injuries to one or more body systems or cavities with sequential systemic reactions that may lead to dysfunction or failure of remote organs and vital systems, which have not themselves been directly injured. It can also be defined as an injury severity score (ISS) of = 17. related terms
.Position screw
A position screw is placed between two adjacent bones or fracture fragments to maintain their normal, relative anatomical relation without applying compression. After restoration of the normal relationship of the bones, a pilot hole or thread hole is drilled through both the near and far cortices. A fully threaded screw is introduced and the absence of a glide hole means that no compression is generated between the head of the screw and the far cortex. The diastasis screw used in type C ankle fractures is an example of a position screw. related terms
.PQ: pronator quadratus
.Prebending (precontouring) of a plate
Preoperative or intraoperative bending of a plate to the shape of the bone. related terms
.
Preload
The application of interfragmentary compression keeps the fragments together until a tensile force is applied which exceeds the compression (preload). related terms
.Preshaped plate
A plate that is designed and shaped during manufacture to fit a specific anatomical site so that intraoperative contouring of the plate is usually not needed. related terms
.Protection (plate)
A plate, or other implant, which reduces the load placed upon a lag screw fixation, thus protecting it from overload. This term has replaced neutralization (plate). more detail related terms
.PRUJ: proximal radioulnar joint
related terms
.
Pseudarthrosis
It literally means false joint. When a nonunion is mobile and allowed to persist for a long period, the bone ends become sclerotic and the intervening soft tissues differentiate to form a type of synovial articulationâ€â€see delayed union, union. related terms
.PTH: parathyroid hormone
.PTSD: post-traumatic stress disorder
.Pure depression articular fracture
An articular fracture in which there is depression of the articular surface alone without split. The depression may be central or peripheralâ€â€see impacted fracture. related terms
.Pure split articular fracture
An articular fracture in which there is a longitudinal metaphyseal and articular split, without any additional osteochondral lesion. related terms
.Push-pull screw
A temporary anchor screw which provides a point of fixation for an instrument to reduce a fracture by distraction and/or compression. related terms
.Push-pull technique
An implant (usually a plate) is applied to one side of a fracture. An instrument (eg, bone spreader) is attached between an anchor point (usually a temporary screw) on the other side of the fracture and the implant. The instrument is then used to distract (push) or appose (pull) the fracture and obtain reduction. related terms
.PWB: partial weight bearing
related terms
.
Q
QCT: quantitative computed tomography
related terms.
QMR: quantitative magnetic resonance imaging
related terms.
QST: quantitative sensory testing.
QUS: quantitative ultrasound.
R
RAPD: relative afferent pupillary defect
related terms.
RCT: randomized control trial.
Reconstruction plate
A notched plate which can be bent on the flat as well as in the conventional manner, producing complex 3-D shapes for fixation of fractures in irregularly shaped bones such as the pelvis. related terms.
Reduction
The realignment of a displaced fracture. related terms
.Reduction screw
A conventional screw used through a plate to pull fracture fragments towards the plate; the screw may be removed or exchanged once alignment is obtained. related terms
.Reduction, direct
Hands or instruments manipulate fracture fragments under direct vision. related terms
.Reduction, indirect
Fragments are manipulated by applying corrective forces at a distance from the fracture zone, by distraction or other means, without exposing the fracture site. related terms
.Refracture
A further fracture occurring after a fracture is solidly bridged by bone, at a load level otherwise tolerated by normal bone. The resulting fracture line may coincide with the original fracture line, or be within the area of bone that has undergone changes as a result of the fracture and its treatment. related terms
.Relative stability
A fixation or support construction that allows small amounts of motion in proportion to the load applied. This results in indirect healing by callus formation. related terms
.
Remodeling (of bone)
The process of transformation of external bone shape (external remodeling), or of internal bone structure (internal remodeling, or remodeling of the Haversian system). related terms
.RES: reticuloendothelial system
.RFN: retrograde femoral nail
related terms
.RIA: reamer irrigator aspirator
.ROM: range of motion
related terms
.RRR: relative risk reduction (or increase)
related terms
.RSD: reflex sympathetic dystrophy
Reflex sympathetic dystrophy (RSD) is also called complex regional pain syndrome (CRPS). related terms
.RSTL: relaxed skin tension lines
.RTW: return to work
.S
Safe zone
A surgeon must be familiar with the anatomy of the different cross sections of a limb in order to avoid injuries to nerves, vessels, tendons, and muscles while placing percutaneous wires or external fixator pins. This must only be carried out in one of the safe zones for pin placement. related terms
.Sagittal plane
This is a vertical plane of the body passing from front to back, so that a sagittal bisection of the body would cut it into a right half and a left half. related terms
.Schanz screw
A partially threaded pin that is inserted into bone as part of external fixation. Standard Schanz screws have a trocar-shaped tip and require predrilling. There are also selfdrilling Schanz screws. related terms
.
Screw
A device for converting rotational movement into longitudinal motion. related terms.
Second look
Surgical inspection of a wound or injury zone, 24–72 hours after the initial management of a fracture or wound. .Segmental
If the shaft of a bone is broken at two levels, leaving a separate shaft segment between the two fracture sites, it is called a “segmental†fracture complex. related terms.
Self-drilling screw
A screw with a sharp, pointed drill tip bearing cutting flutes which will cut its own threaded pilot hole. related terms
.
Self-tapping screw
A screw with cutting flutes which create a thread in a predrilled pilot hole as the screw is inserted into the pilot hole. A tap is not used. related terms
.
Sequestrum
A piece of dead bone lying alongside but separated from the osseous bed from which it came. Infected sequestra are formed in chronic osteomyelitis. related terms
.Shear
A shearing force is one which tends to cause one segment of a body to slide upon another, as opposed to tensile forces, which tend to elongate or shorten a body. related terms
.SIGN: Surgical Implant Generation Network
.Simple fracture
There is a single fracture line producing two fracture fragments. related terms
.
SIRS: systemic inflammatory response syndrome
related terms.
SMP: sympathetically maintained pain
related terms.
SPION: superparamagnetic iron oxide nanoparticles
.Splint, gliding
The linkages (couples) between the bone and the splinting device allow (controlled) axial movement, so that the distance between the couples can change (eg, dynamically locked nail). related terms
.Splint, locked
There is a fixed linkage (couple) between the bone and splinting device, above and below the fracture zone, so that the working length between the couples cannot change (eg, statically locked nail). related terms
.
Splinting
A splint is made of stiff material that is applied to a fractured body region to reduce motion at the fracture site. It can be applied externally (plaster cast, external fixator) or internally (plate, intramedullary nail, internal fixator). related terms
.Split-depression articular fracture
An articular injury with a fracture line running into the metaphysis (split) and impaction of separate osteochondral joint fragments (depression). related terms
.Spontaneous fracture
A fracture that occurs at physiological load or stress, usually in abnormal boneâ€â€see pathological fracture. related terms
.SSSC: superior shoulder suspension complex
.Stability, absolute
Fixation of fracture fragments so that there is virtually no displacement of the fracture surfaces under physiological load. This allows direct bone healing. related terms
.Stability, relative
A fixation or support construction that allows small amounts of motion in proportion to the load applied. This results in indirect healing by callus formation. related terms
.Stable fixation
Fixation of a fracture that allows early motion of the adjacent joints and provides a mechanical environment that allows fracture healing before failure of the implant. related terms
.
Stiffness
The ability of a material to resist deformation. It is measured as the relationship between load applied and the resulting elastic deformation. The inherent stiffness of a material is expressed by its modulus of elasticity. more detail related terms
.Stiffness, bending
The bending stiffness of an intramedullary nail is inversely proportional to the square of the working length. related terms
.Stiffness, torsional
Torsional stiffness of an intramedullary nail is inversely proportional to the working length. related terms
.
Strain
Change in length of a material when a given force is applied. Normal strain is the ratio of deformation (lengthening or shortening) to original length. It has no dimensions but is often expressed as a percentage. related terms
.Strain theory by Perren
With a small fracture gap, any movement will result in a relatively large change in length (ie, high strain). If this exceeds the strain tolerance of the tissue, healing will not take place. If a larger fracture gap is subjected to the same movement, the relative change in length will be smaller (ie, less strain) and, if the critical strain level is not exceeded, there will be normal tissue function and indirect healing by callus. related terms
.
Strain tolerance
This determines the tolerance of tissues to mechanical conditions. No tissue can function normally when an increase in length (ie, strain) causes the tissue to disrupt. This is the critical strain level. .Strength
The ability of a material to resist the application of force without deformation. The strength of a material can be expressed as ultimate tensile strength, bending strength, or torsional strength. Strength determines the level of load an implant can resist. related terms
.Stress concentration
The build-up of stresses in an implant or bone where there is a defect, a change in cross section, a hole, or a scratchâ€â€see stress distribution. related terms
.Stress distribution
As bending stresses are distributed over a long segment of a plate, the stress per unit area is correspondingly low, which reduces the risk of fatigue failure. related terms
.Stress protection
Using a plate to reduce peak loads applied to a screw fixationâ€â€see protection (plate). related terms
.Stress riser
A defect (eg, empty screw hole) that brings about a concentration of stressâ€â€see stress concentration. related terms
.Stress shielding
Bone deprived of functional stimulation by having its physiological stresses reduced by a load-sharing implant may react by becoming less dense according to Wolff’s law (1872). related terms
.Subluxation
A displacement of a joint with partial contact between the two articular surfaces. related terms
.SUN: simplified universal nail
related terms
.SXA: single x-ray absorptiometry
related terms
.T
TAN: titanium aluminium niobium
related terms
.Tap
The process by which a thread is cut in a predrilled hole. It also refers to the instrument used to cut the thread. related terms
.TBI: traumatic brain injury
.TEN: titanium elastic nail
related terms
.
Tension band
The principle by which an implant, attached to the tension side of a fracture, converts the tensile force into a compressive force at the cortex opposite the implant. While wires, cables, and sutures are often used for tension band fixation, plates and external fixators, when appropriately placed, can also function as tension bands. more detail related terms
.TFCC: triangular fibrocartilaginous complex
related terms
.TFN: trochanteric femoral nail
related terms
.TGF: transforming growth factor
.Thread hole
A pilot hole is drilled and a tap is used to cut the spiral groove that receives the thread of the screw. The result is a thread hole. related terms
.Ti-15Mo: titanium molybdenum
related terms
.TLSO: thoracolumbosacral orthosis
related terms
.TMJ: temporomandibular joint
.Toggling
Slight movement at the couple between a screw and a plate or intramedullary nail. Implants may be designed to allow toggle, eg, intramedullary nails, where the tolerances of the assembly do not permit exact fit. Toggle between plates and screws may occur during plate failure with loosening of the implant. related terms
.Torque
The moment produced by a turning or twisting force. As an example, torque is applied to drive home and tighten a screw. The moment is equal to the product of lever arm (unit meter) and force (unit Newton) producing torsion and rotation about an axis (the unit of torque in Newton meter). related terms
.Torsional stiffness
Torsional stiffness of an intramedullary nail is inversely proportional to the working length. related terms
.TPLO: tibial plateau leveling osteotomy
related terms
.
Traction table
An operating table with attachments that allow safe and precise positioning of the patient and the application of tension or compression through a limb to reduce a fracture and allow access for surgery and radiological imaging. Also known as a fracture table. related terms
.Translation
Displacement of one bone fragment in relation to another, usually at right angles to the long axis of the bone. related terms
.TRAP: triceps-reflecting anconeus pedicle
.TSP: trochanteric stabilizing plate
.TTWB: touch toe weight bearing
related terms
.U
UHMWPE: ultra-high molecular weight polyethylene
related terms
.UHN: unreamed (solid) humeral nail
related terms
.Union
The bone has healed and regained its normal stiffness and strength. In clinical terms, this means there is no movement or tenderness at the fracture site and no pain on stressing the fracture site. Radiologically, there should be evidence of bone trabeculae bridging the fracture site. related terms
.
.USS: universal spine system
related terms
.UTN: unreamed tibial nail
related terms
.V
VAC: vacuum-assisted wound closure
An open wound is sealed with an impervious, adherent dressing and low pressure suction is applied to remove any exudates and enhance the formation of granulation tissue. .Vacuum-assisted wound closure
An open wound is sealed with an impervious, adherent dressing and low pressure suction is applied to remove any exudates and enhance the formation of granulation tissue.
Valgus
Deviation away from the midline in the anatomical position. related terms.
Varus
Deviation towards the midline in the anatomical position. related terms.
VAS: visual analog scale.
VEGF: vascular endothelial growth factor
related terms.
VEP: visual evoked potential
related terms.
VTE: venous thromboembolism
related terms.
W
Wave plate
The central section of a plate is contoured to stand off the near cortex over a distance of several holes. This leaves a gap between the plate and the bone, which (a) preserves the biology of the underlying bone, (b) provides a space for the insertion of a bone graft, and (c) increases the stability because of the distance of the waved portion of the implant from the neutral axis of the shaft. Such plating is useful in nonunion treatment. related terms.
WBAT: weight bearing as tolerated
related terms.
Wedge fracture
A fracture complex with a third fragment, mostly due to a direct trauma, in which, after reduction, there is some direct contact between the two main fragmentsâ€â€see butterfly fragment. related terms.
Working length
The distance across a fracture site between the two nearest points where the implant (usually an intramedullary nail) and the bone are coupled. related terms
X
Xenograft
Tissue transplanted from one species to another. related terms.
Y
Young's modulus
Ratio of stress to strain in the linear region of a stress-strain curve. .Z
Zone of injury
The entire volume of bone and soft tissue damaged by energy transfer during trauma. The microcirculation is disturbed and this may endanger tissue viability. related terms.
|
What should you do before going ahead with any emergency surgery?
Verify diagnosis and alternative treatments with two other competent doctors.
Document the findings of three separate doctors separately.
Experience has revealed that an individual who knows how to make an eight-inch incision and closing in three layers.
This individual is claiming to be surgeon specialist.
A surgical technician knows more than these skills.
Correct diagnosis of a human in various healthcare settings with various options of treatment is a prerequisite for all medical doctors.
Injury Prevention Issues
INJURY PREVENTION
With the degree of injury that is preventable, trauma centers need to focus on prevention programs and healthy communities. Although sometimes difficult to measure, a program is effective if even one injury is prevented. Programs should focus on local common causes of injury. The data is obtainable through the trauma registry and local databases, such as the medical examiner and police crash database.
Education  Most commonly offered program  Lecture format, brochures, ads on television or newspaper/ billboards  Common topics include Motor vehicle safety (seat belts, car seats, airbags, drinking and driving, speed, elder driving training) Playground safety (structure, surface, architecture) Home safety (burn, fire prevention, fall prevention/ exercise) Gun safety (proper handling, locks/safes)  Messages should be simple, clear statements
|
Airway Adjuncts
Bag-Mask Ventilation
Nasopharyngeal/Oropharyngeal Airways
Airway Adjuncts
Nasopharyngeal/Oropharyngeal Airways

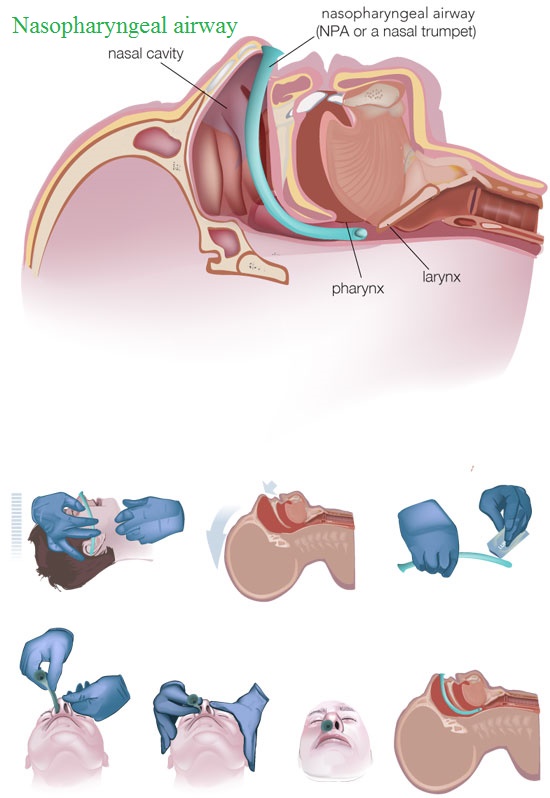
Nasopharyngeal and oropharyngeal airways can be very useful tools in certain situations, in both the field and hospital setting. But before reaching for one of these airway devices, it is essential to understand the indications, contraindications and appropriate use of these devices.
Function and Indications
When a patient becomes unconscious, regardless of the cause, maintaining a patent airway is critical. One of the most common causes of airway obstruction in an unconscious patient is the tongue. Once a person loses consciousness, the tongue may fall to the back of the throat and block the patient’s airway. Using an oropharyngeal or nasopharyngeal airway is an effective way to maintain an open airway, which allows you to ventilate the patient effectively if needed.
The main indication for use of an oropharyngeal airway is if your patient is at risk for airway obstruction due to relaxed upper airway muscles or blockage of the airway by the tongue. For example, if you perform a head tilt-chin lift maneuver on a patient to open their airway and are not able to ventilate the patient successfully, placement of an oropharyngeal airway is indicated. In addition, if you are manually ventilating a patient you may inadvertently push down on the patient’s chin, obstructing their airway. Using an oropharyngeal airway can prevent this from occurring. Oral airways can only be used in the unconscious patient.
A nasopharyngeal airway is a second type of device that can be used for patients who are either conscious or unconscious. It is also used to keep the airway open and is especially helpful in semi-conscious patients. Semi-conscious patients may still be at risk for airway obstruction, but cannot have an oropharyngeal airway placed due to an intact gag reflex.
Nasopharyngeal airways may work well for patients who are clenching their jaw, which makes inserting an oral airway difficult. A nasopharyngeal airway can also be helpful in patients who are semi-conscious and need frequent nasal-tracheal suctioning.
Insertion Procedure
The first step in inserting either type of adjunct airway device is selecting the correct size. If you select an inappropriate size, the device will not serve its purpose and could cause more harm than good.
The oropharyngeal airway should be measured from the corner of the patient’s mouth to the angle of the mandible. A device that is too big may cause injury or block the airway.
Before inserting the airway, clear the mouth of secretions such as vomit, blood or sputum using a suction catheter. Place the oral airway in the mouth with the curved end towards the hard palate or the roof of the mouth. As you are inserting the device and it approaches the posterior pharynx, rotate the device 180 degrees into the correct position.
After the oral airway is inserted, the flange of the device should rest on the patient’s lip. There is no need to secure the device with tape. Be sure to suction the airway as needed.
Similar to the oropharyngeal airway, if you choose to use a nasopharyngeal airway, selecting the proper size is also important. To determine the correct size, measure from the tip of your patient’s nose to the tip of their earlobe. In addition, choose a nasopharyngeal airway which has a diameter a little smaller than the patient’s nares.
A nasopharyngeal airway should be inserted with the bevel pointing towards the septum and following the natural curvature of the floor of the nasal cavity as it is advanced. Once the device is inserted the flange should rest on the nostril opening.
Contraindications
Using an oropharyngeal airway on a conscious patient with an intact gag reflex is contraindicated. If your patient has the ability to cough they still have a gag reflex and you should not use an oral airway. If the patient has a foreign body obstructing the airway, an oropharyngeal airway should also not be used.
There are few contraindications for using a nasopharyngeal airway. The device should not be used on patients who have nasal fractures or an actively bleeding nose. In some cases, slight bleeding may occur when you insert the airway, which can be suctioned or wiped away.
Tips
•Be gentle when inserting either type of airway device.
•Use a water soluble lubricant when inserting a nasopharyngeal airway.
•Avoid forcing an oral airway, which can lead to trauma to the lips and tongue.
•If resistance is felt during insertion of a nasopharyngeal airway, stop and try the other nostril.
•Research has shown that the right nare is larger in most people- try the right nare first.
|
Advanced Airways
Endotracheal Intubation

Indications of endotracheal intubation.
Routine To provide anaesthesia
Emergency
Airway obstruction
Respiratory distress
Oxygenation failure (hypoxia)/Acute
Ventilation failure (hypercarbia)/Acute
Mental status alteration (GCS<8/15)/Acute
Flail chest/Pulmonary contusion/Acute
Cardio pulmonary resuscitation/Acute
Endotracheal tubes are used for patients undergoing a procedure that requires general anesthesia and/or mechanical ventilation. They are inserted either through the nose or the mouth past the epiglottis and vocal cords into the trachea and down to where the trachea bifurcates into the bronchi. ET tubes are not usually left in place for more than 14 days as doing so places the patient at risk for infection and airway injury.
Endotracheal tubes are made of a flexible plastic material and are available in a variety of sizes. The size used depends on the age and size of the patient. For adult patients, the ET tube will usually have a cuff that is inflated with air after insertion to prevent air from leaking around the tube and to prevent oral and gastric secretions from being aspirated.
Endotracheal Intubation
Use of Devices to Confirm Tube Placement
Postintubation Care
Automatic Transport Ventilators
Esophageal-Tracheal Combitube
Laryngeal Mask Airway
The LMA provides a more secure and reliable means of ventilation than the face mask.
Here are further guidelines.
|
Tracheostomy tube
Do not go ahead with surgery without second and third consultation from senior physicians for verification of diagnosis and appropriate treatment.
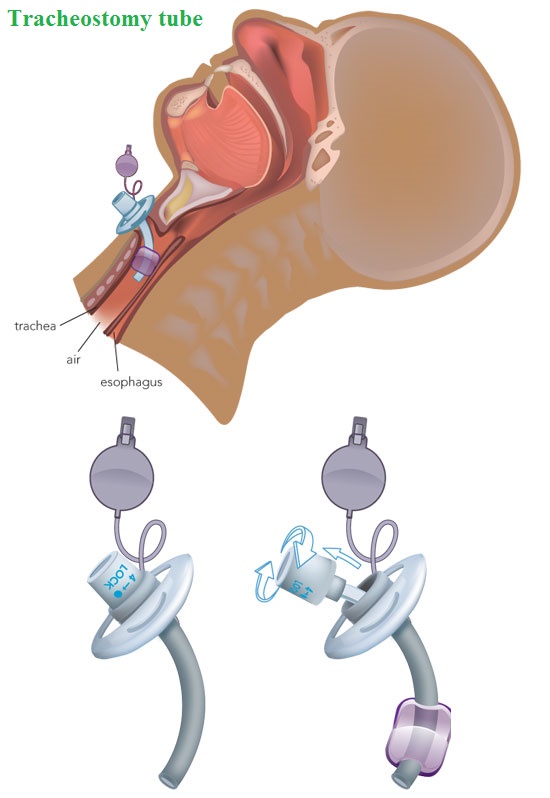 Tracheostomy tubes are used for long-term airway support. They are inserted through a small opening in the neck into the trachea. This type of airway may be permanent or temporary depending on the patient’s condition and reason for the tracheostomy.
Tracheostomy tubes are used for long-term airway support. They are inserted through a small opening in the neck into the trachea. This type of airway may be permanent or temporary depending on the patient’s condition and reason for the tracheostomy.
Tracheostomy tubes are made of either plastic or metal and are available in a variety of sizes. Because metal tracheostomy tubes are temperature-sensitive, they must be protected from heat and cold to prevent tissue injury. Like ET tubes, tracheostomy tubes may have a cuff that is inflated with air after insertion. Most tracheostomy tubes have an inner cannula that is temporarily removed during tracheostomy care.
Of the various types of airway management devices, a tracheostomy tube is the only one whose placement requires a surgical procedure. Postoperatively, the nursing priority is maintaining a patient airway. Tube obstruction is a major complication, as is tube dislodgement during the first 72 hours postoperatively. It is essential to keep a manual resuscitation bag, a tracheostomy tube of the same size and type, and a tracheostomy insertion tray at the patient’s bedside. Some other possible complications are pneumothorax, subcutaneous emphysema, hemorrhage (although small amounts of blood are to be expected), and infection, manifested by purulent drainage, erythema, pain, and edema.
|
Case scenario
On-the-spot emergency medical diagnosis and treatment
Early Management of Severe Trauma
Police officers, particularly police patrolling officers
Why do police patrolling officers need to know early management of severe trauma?
Usually, police patrolling officers know about trauma incident before emergency medical responders reaches the scene, physicians.
Simple techniques by police patrolling officer can save life of a severe trauma patient.
What do police patrolling officers have to do in severe trauma cases?
Can the patient speak relevant to age?
If yes, the airway is likely to be clear.
Ask patient these questions.
How are you?
Can I see you identity card?
No response.
Position the patient properly.
Position of patient on spot.
Supine
Airway maintenance
1. Chin lift or jaw thrust.
2. Airway adjuncts may be required.
Police officer can do these above mentioned maneuvers by the time physicians or paramedics arrive.
Physician medical emergency room
Physician surgeon medical emergency
Physician medical emergency responder
Paramedics
Other advanced practitioners use ATLS
Police officers, particularly police patrolling officers
Others relevant to requirement
What do you have to do?
1. Chin lift or jaw thrust.
2. Airway adjuncts may be required.
3. If the airway is blocked (e.g., by blood or vomit), the fluid must be cleaned out of the patient's mouth with the help of suctioning instruments.
4. In case of obstruction, pass an endotracheal tube.
If the airway is blocked (e.g., by blood or vomit), the fluid must be cleaned out of the patient's mouth with the help of suctioning instruments.
In case of obstruction, pass an endotracheal tube.
|
Prevention of trauma
Fix the underlying cause of trauma.
There are more than 12 causes of trauma.
Gun harms prevention.
Here are further guidelines.
http://www.qureshiuniversity.com/gunviolence.html
Prevention of trauma due to road traffic crashes.
Take public transportation.
Identify high risk locations for public transportation and fix the issues in the state and outside the state.
Identify high risk vehicles for public transportation and fix them.
Fix the underlying cause of trauma.
There are more than 12 causes of trauma.
|
Last Updated: August 10, 2023
|



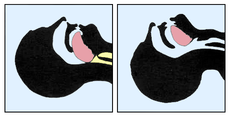

 vehicle.
vehicle.  will be hit on the chest.
will be hit on the chest. 

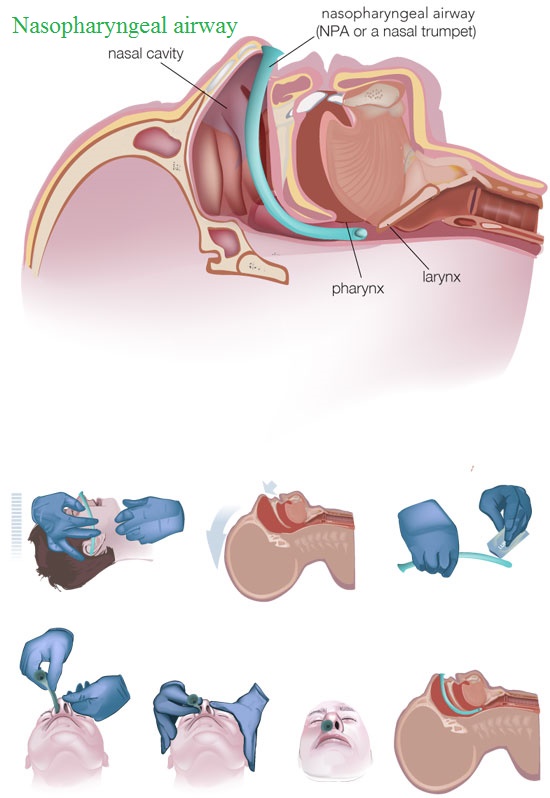

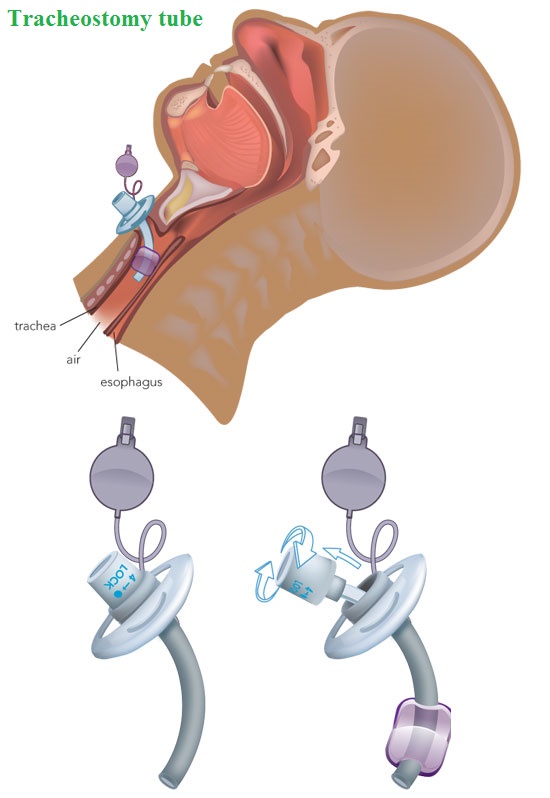 Tracheostomy tubes are used for long-term airway support. They are inserted through a small opening in the neck into the trachea. This type of airway may be permanent or temporary depending on the patient’s condition and reason for the tracheostomy.
Tracheostomy tubes are used for long-term airway support. They are inserted through a small opening in the neck into the trachea. This type of airway may be permanent or temporary depending on the patient’s condition and reason for the tracheostomy.