|
Acute Coronary Syndrome (ACS) |
Term that describes a range of clinical conditions, including unstable angina, that are due to insufficient blood supply to the heart muscle resulting from coronary heart disease (CHD)
|
|
Acute Myocardial Ischemia |
An episode of chest pain due to reduced blood flow to the heart muscle
|
|
Angina Pectoris |
Pain in the chest that comes and goes at different times; caused by a lack of oxygen reaching the heart; can be stable (occurring under exertion or stress) or unstable (occurring at rest, without reason)
|
|
Arrhythmia |
Disturbance in the regular rhythmic beating of the heart
|
|
Asystole |
A condition where the heart has stopped generating electrical activity
|
|
Atherosclerosis |
A condition in which deposits of plaque, including cholesterol (a fatty substance made by the liver and found in foods containing animal or animal products) build up on the inner walls of the arteries, causing them to harden and narrow, reducing the amount of blood that can flow through; develops gradually and can go undetected for many years
|
|
Atrial Fibrillation |
Irregular and fast electrical discharges of the heart that lead to an irregular heartbeat; the most common type of abnormal cardiac rhythm
|
|
Atrioventricular (AV) Node |
A cluster of cells in the center of the heart, between the atria and the ventricles; serves as a relay to slow down the signal received from the sinoatrial (SA) node before it passes through to the ventricles
|
|
Automated External Defibrillator (AED) |
A portable electronic device that analyzes the heart's electrical rhythm and, if necessary, can deliver an electrical shock to a person in cardiac arrest
|
|
Cardiac Arrest |
A condition in which the heart has stopped or beats too irregularly or weakly to pump blood effectively
|
|
Cardiac Chain of Survivial |
A set of four critical steps in responding to a cardiac emergency: early recognition and access to the EMS system, early cardiopulmonary resuscitation (CPR), early defibrillation, and early advanced medical care
|
|
Cardiopulmonary Resuscitation (CPR) |
A technique that combines chest compressions and ventilations to circulate blood containing oxygen to the brain and other vital organs for a person whose heart and breathing have stopped
|
|
Cardiovascular Disease |
A disease affecting the heart and blood vessels
|
|
Chest Compressions |
A technique used in CPR, in which external pressure is placed on the chest to increase the level of pressure in the chest cavity and cause the blood to circulate through the arteries
|
|
Cholesterol |
A fatty substance made by the liver and found in foods containing animal or animal products; diets high in cholesterol contribute to the risk of heart disease
|
|
Commotio Cordis |
Sudden cardiac arrest from a blunt, non-penetrating blow to the chest, of which the basis is ventricular fibrillation (V-fib) triggered by chest wall impact immediately over the heart
|
|
Congestive Heart Failure |
A chronic condition in which the heart no longer pumps blood effectively throughout the body
|
|
Coronary Heart Disease (CHD) |
A disease in which cholesterol and plaque build up on the inner walls of the arteries that supply blood to the heart; also called coronary artery disease (CAD)
|
|
Defibrillation |
An electrical shock that disrupts the electrical activity of the heart long enough to allow the heart to spontaneously develop an effective rhythm on its own
|
|
Electrocardiogram (ECG or EKG) |
A test that measures and records the electrical activity of the heart
|
|
Heart |
A fist-sized muscular organ that pumps blood throughout the bod
|
|
Hypertension |
Another term for high blood pressure
|
|
Implantable Cardioverter-Defibrillator (ICD) |
A miniature version of an AED, implanted under the skin that acts to automatically recognize and help correct abnormal heart rhythms
|
|
Myocardial Infarction (MI) |
The death of cardiac muscle due to a sudden deprivation of circulating blood; also called a heart attack
|
|
Normal Sinus Rhythm (NSR) |
The normal, regular rhythm of the heart, set by the sinoatrial node in the right atrium of the heart
|
|
Pacemaker |
A device implanted under the skin, sometimes below the right collarbone, to help regulate heartbeat in someone with a weak heart, a heart that skips beats, or one that beats too fast or too slow
|
|
Risk Factors |
Conditions or behaviors that increase the chance that a person will develop a disease
|
|
Silent Heart Attack |
A heart attack during which the patient has either no symptoms or very mild symptoms that the person does not associate with heart attacks; mild symptoms include indigestion or sweating
|
|
Sinoatrial (SA) Node |
A cluster of cells in the right atrium that generates the electrical impulses that set the pace of the heart's natural rhythm
|
|
Sudden Cardiac Arrest |
A condition where the heart's pumping action stops abruptly, usually due to abnormal heart rhythms called arrhythmias, most commonly V-fib; unless an effective heart rhythm is restored, death follows within a matter of minutes
|
|
Transdermal Medication Patch |
A patch on the skin that delivers medication; commonly contains nitroglycerin, nicotine, or other medications; should be removed prior to defibrillation
|
|
Ventricular Fibrillation (V-fib) |
A life-threatening heart rhythm in which the heart is in a state of totally disorganized electrical activity
|
|
Ventricular Tachycardia (V-tach) |
A life-threatening heart rhythm in which there is very rapid contraction of the ventricles
|
|
Form a General
Impression
|
Observe overall appearance of the patient, age, body position, and responsiveness. Observe
work of breathing and circulation. Pale skin and cyanosis are indicators of poor perfusion.
Determine the level of consciousness using the AVPU scale. Is the patient calm or anxious? Is
the patient able to speak in full sentences? Identify immediate threats to life. Determine priority
of care based on the MOI/NOI. If the patient is unconscious, determine whether CPR is needed.
If the patient has a poor general impression, call for ALS assistance. A rapid visual examination
will help you identify and manage life threats.
| |
|
Airway and
Breathing
|
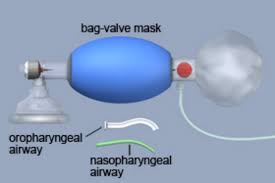
Ensure the airway is open, clear, and self-maintained. If needed, open and maintain the air-
way using a modi?ed jaw-thrust if a cervical-spine injury is suspected or a head-tilt—chin-lift
in nontrauma patients. A patient with an altered level of consciousness may need emergency
airway management; consider inserting a properly sized oropharyngeal airway in an unconscious
patient or use a nasopharyngeal airway if the patient has an intact gag re?ex. Assess for gur-
gling and stridor. Suction as needed. Evaluate the patient’s ventilatory status for rate and depth
of breathing, respiratory effort, and tidal volume. Quickly assess the chest for DCAP-BTLS,
accessory muscle use, and intercostal and abdominal muscle use, and treat any threats to life.
Assess lung sounds and determine whether they are normal, decreased, abnormal, or absent.
Patients with cardiac problems may present with crackles or rales, indicating ?uid (edema) in the
lungs. Administer high-?ow oxygen at 15 L/min, providing ventilatory support as needed.
| |
|
Circulation |
Evaluate distal pulse rate, quality (strength), and rhythm. Tachycardia may be an indicator of
shock or a myocardial infarction. Bradycardia might be due to cardiogenic shock as the heart
attempts to reduce oxygen demand. Observe skin color, temperature, and condition and capillary
re?ll time. Look for and treat any external bleeding. The transport of blood and oxygen may be
reduced if cardiac output is low. If distal pulses are not palpable, assess for a central pulse.
| |
|
Transport
Decision
|
If the patient has an airway or a breathing problem, severe chest discomfort, signs and
symptoms of internal bleeding, or other life threats, manage the problems immediately, and con-
sider rapid transport, performing the secondary assessment en route to the hospital. Delayed
transport in a cardiac emergency will cause more cardiac muscle damage. For patients without
life threats and in stable condition, perform a thorough assessment and history on scene. Do
not allow the patient to exert himself or herself by walking to the ambulance; a carrying device
should be used. Transportation should be to a cardiac care facility if one is close, otherwise take
the patient to the nearest hospital for evaluation and stabilization. Do not delay transport to
manage non—life-threatening conditions, instead treat en route to the hospital. Lights and sirens
might cause anxiety and stress to a patient with a cardiac problem; patient condition and dis-
tance from the hospital are factors you can use to evaluate the need to use lights and siren.
| |