| What should every type of physician know? |
|
What should other physicians who claim to be surgeons know? How should seniority of physician surgeon medical emergency, physician surgeon elective surgery be categorized? What should physician surgeon medical emergency know? What should physician surgeon elective surgery know? How many subcategories of surgeries are there? How are other regions categorizing surgical categories? What questions should be answered before, during and after surgical procedure? |
Physician surgeon medical emergency
Human Organ Systems functions
Human
|
What are you expected to know about a matured human? Annotations or definition. Abilities. Bones. Drugs required for human medical conditions. Equipment required for human medical conditions. Health care settings. Human anatomy by category. Resources required for human health care. Internal organs (main). Muscles. Medical conditions. Systems of the human body Survival needs. What is a human? Human as per scientific classification. Human as per human body systems. Human as per matured human abilities. How many human body systems are there? 11 The structure of the 11 systems of the human body is different than other mammals. What are the names of human body systems? http://www.qureshiuniversity.com/human.html How many bones, muscles, internal organs, and cells does a mature human have? Bones: 206 Internal organs (main): 22 Muscles: 600 100 trillion cells How many human body bones are there in one matured human being? (206) What are the names of human body bones? www.qureshiuniversity.com/human.html How many human body muscles are there in one matured human being? 600 muscles What are the names of human body muscles? www.qureshiuniversity.com/human.html Human anatomy by category How many human anatomy categories are there? 19 What should you know about human anatomy by category? www.qureshiuniversity.com/human.html How many human body internal organs are there in one human being? 22 internal organs What are the names of human body internal organs? www.qureshiuniversity.com/human.html How many abilities should a matured human have relevant to age? 24 abilities. What is a matured human? A matured human is an individual between 18 to 75 years old. What are examples of matured human abilities relevant to age? Abstract reasoning Breathing Clothing Cooking food Communicating through various means (written, spoken, sign language). English language Caring for oneself (eating, dressing, toileting, etc.) Creating and using numerous other technologies Creating and extinguishing fires or heat Following a variety of values, social norms, and rituals Getting started after sleep Hearing Intellectual ability knowledge, English language abilities, and able to answer Learning Language (English language, problem solving) Moving or manipulating objects Performing manual tasks Replying to relevant questions Seeing Speaking Sitting Sleeping normally Having sexual desire Working Walking This is applicable to 18–75-year-olds. If an individual is less that 18 or more than 75 and feels issues are not due to age less than 18 or old age, that individual needs evaluation as well. Here are further guidelines. |
Annotation or definition of surgical emergencies.
|
What is a surgical emergency? A surgical emergency is a medical emergency for which immediate surgical intervention is the only way to solve the issue successfully. How have surgical emergencies been categorized? Pediatric surgical emergencies. Adult surgical emergencies, age 19 and older. What are prerequisites so that you become a competent physician surgeon medical emergency, physician surgeon elective surgery? You should be able to answer: What should every type of physician know? Here are further guidelines. http://www.qureshiuniversity.com/physician.html What are examples with diagnosis of surgical emergencies? There are more than 50 such examples of surgical emergencies. |
Types of surgical emergencies.
|
What should physician surgeon medical emergency know? You have to know everything of these entities.
|
Obstetrics emergencies
|
6 Pregnancy Warning Signs Vaginal Bleeding Baby’s Activity Level Significantly Declines Contractions Early in the Third Trimester Leakage of Fluid from the Vagina Headache Severe Nausea and Vomiting A Persistent Severe Headache, Abdominal Pain, Visual Disturbances, and Swelling During Your Third Trimester The first principles of dealing with obstetric emergencies are the same as for any emergency (see to the airway, breathing, and circulation), but remember that in obstetrics there are two patients; the fetus is very vulnerable to maternal hypoxia Abruption of the placenta Placenta praevia Postpartum haemorrhage Amniotic fluid embolism Inversion of uterus Infection Psychological conditions Stillbirth and intrauterine death Clinical features of abruption of the placenta Symptoms •Abdominal pain •Severe shock with symptoms beyond vaginal blood loss •Vaginal bleeding—usually old blood Signs •Shock •Spasm of uterus—described as woody •Tender uterus •Fetal parts hard to feel •Often no fetal heart is heard All emergency protocols should have been considered beforehand and mutually agreed by obstetricians, midwives, general practitioners, and paramedics. Everybody then knows their immediate priority, and hazards to the woman can be minimised. Abruption of the placenta An abruption is a death threat to the fetus and a hazard to the mother. When the placenta separates from its bed (probably because of the rupture of a malformed blood vessel), the damage to the fetus follows not just because of the barrier that the clot makes between the placental bed and villi but also because the release of prostaglandins causes a major degree of uterine spasm. This interferes with perfusion of the placenta, which remains attached. Blood tracking into the myometrium often goes as far as the peritoneum over the uterus, causing much pain and shock, with spasm of the uterine muscle. Emergency treatment of abruption Treat the shock •Give oxygen •Insert intravenous lines •Arrange a cross match of 6 units of blood •Give morphine (if fetus dead) Deliver the fetus •By caesarean section (if fetus is alive and gestation is mature) •By rupturing membranes (if cervix is ripe or fetus is dead) Treat disseminated intravascular coagulopathy •Urgent haematological consultation •Check platelet count •Give cryoprecipitate (fresh frozen plasma) •Transfuse with fresh blood if available In major degrees of placental abruption the woman is shocked well beyond the apparent amount of blood loss and needs urgent transport into hospital. A wide bore intravenous line should be set up and blood sent for cross matching of at least six units of blood. Until this blood arrives, other plasma expanding fluids, such as Haemaccel, should be used. If the fetus is still alive and gestation sufficiently advanced, caesarean section is the best management. However, if the fetus is dead, conservative management can be pursued provided that the woman does not continue deteriorating—for example, by developing a coagulopathy. Most women with a severe abruption that kills the fetus will go into spontaneous labour soon and have an easy delivery, but caesarean section is occasionally necessary for maternal indications alone. Treatment must be aimed at the shock and at preventing disseminated intravascular coagulopathy. Usually the placenta is implanted on the anterior wall of the uterus, but sometimes it is posterior when the abruption is less painful and not so severe that the mother is shocked; the fetus may still be at risk, however. Diagnosis in these cases is by recognition of the excessively frequent contractions produced by the prostaglandin release and the abnormal pattern of the fetal heart rate secondary to fetal hypoxia; these are best shown with cardiotocography, a priority investigation in all women admitted with abdominal pain in pregnancy. Placenta praevia The blastocyst occasionally implants in the lower part of the uterus. Stretching and thinning of the uterine muscle of the lower segment in the third trimester may sheer off part of the placental attachment. This is accompanied by painless bleeding. Clinical aspects of placenta praevia Symptoms •Vaginal bleeding—bright red, painless, recurrent Signs •Soft, pain free uterus •Easy to feel fetus—often high head, breech, or transverse lie •No fetal distress •Do not do a digital vaginal examination •A speculum examination in an inpatient to exclude any local bleeding is acceptable Often the fetus is not affected by the first small bleeds, but they should be taken seriously for there is a risk that the mother could have a much larger bleed. Hence, women with bright red, painless vaginal bleeding are considered to have placenta praevia until proved otherwise and should be admitted to hospital. Vaginal ultrasound examination is the best technique for investigating possible placenta praevia, but, although it has a high sensitivity and specificity for central placenta praevia in the third trimester, it is much less precise in the late second trimester or for marginal placenta praevia. Management should therefore always be based on appropriate clinical judgment. If placenta praevia is confirmed the woman should stay in hospital for at least 48 hours after the bleeding has stopped. Management is conservative, even to the level of giving blood transfusions for severe bleeds, until the fetus is mature (at about 36 weeks). Studies do not show any benefit in keeping women in hospital until delivery, provided that they have a telephone at home and live close enough to the hospital to be brought in by the emergency services within 20 minutes if they start bleeding again (Love et al, 1996). Unless it is very obvious—for example, a complete placenta praevia on ultrasound examination, together with a transverse lie of the fetus—placenta praevia is sometimes confirmed by examination under general anaesthesia in theatre, proceeding in most instances to caesarean section performed by a senior obstetrician. Occasionally, if the placenta is anterior and only just engaging in the lower segment, the membranes may be ruptured and a vaginal delivery expected, as the head coming down into the mother’s pelvis will compress the bleeding placental bed against the back of the pubis symphysis. The same cannot be said for any degree of posterior placenta praevia. After delivery, a postpartum haemorrhage is likely because the placental bed is situated over less well contracting uterine muscle and may well bleed despite oxytocic stimulation. This often requires blood transfusion. Postpartum haemorrhage After a normal delivery a woman commonly loses up to 300 ml of blood. As her blood volume has increased because of fluid retention during pregnancy, this is a loss which can be coped with readily. However, a loss of >500?ml measured clinically in the first 24 hours is considered to be a primary postpartum haemorrhage. Blood loss is commonly underestimated by the attending practitioners. The mother should be watched carefully and treatments given to prevent any further loss. Management of primary postpartum haemorrhage Preventive •Intramuscular oxytocin at the end of the second stage of labour Curative •Repeat oxytocic administration •Rub up a contraction •Check completeness of the placenta—if it is not delivered or a lobule is missing, prepare for manual removal •Bimanual compression •Intramyometrial prostaglandin E2 or carboprost •Surgical ligation—uterine arteries, internal iliac arteries, or braces (or Lynch) suture of uterus •Hysterectomy If the uterus has not contracted firmly, manual stimulation may work by rubbing up a contraction, and a further oxytocic is given. If the placenta is incomplete the uterine cavity is explored for the remaining lobules whose presence in the uterine cavity may prevent the organ contracting down. If neither of these conditions exists, trauma to the lower uterus, cervix, or upper vagina may be the cause of the bleeding. Such traumas should be looked for (in theatre with a good light) and sutured appropriately. A rare cause of continuing primary postpartum haemorrhage is a rupture of the uterus. This needs diagnosis and treatment with either hysterectomy or abdominal resuturing. After the first 24 hours, any bleeding is a secondary postpartum haemorrhage. It is commonly associated with infection, which should be treated vigorously with intravenous antibiotics. If it persists, suction evacuation of the uterus should be undertaken by a senior obstetrician; perforation of the soft uterus is a major risk in this situation. A complication of severe and prolonged blood loss is a consumptive coagulopathy, when the mother’s blood does not clot owing to interference with the clotting cascade. The continuing cooperation of a senior haematologist is essential. The mother continues to bleed not just from the placental bed but from other sites in the body. This needs firm and prompt correction so that full coagulation can be restored. Giving cryoprecipitate (frozen precipitate) provides the missing components. Amniotic fluid embolism Occasionally, when the uterus is contracting strongly and there is an opening between the amniotic sac and the uterine veins, a bolus of amniotic fluid is pumped into the circulation. This passes through the heart, and an accumulation of amniotic cells becomes trapped in the pulmonary circulation. The amniotic fluid may cause local disseminated intravascular coagulation, which may spread. This rare condition can occur late in the last trimester or during labour. Amniotic fluid embolism used to be diagnosed on histology only after a postmortem examination but is now sometimes diagnosed before death. The symptoms include collapse while having strong contractions, shock without any blood loss, sudden dyspnoea, and the production of frothy sputum. Treatment is supportive, with steroids, intravenous plasma expansion, and urgent delivery. This obstetric emergency is rare and has a bad prognosis for both mother and fetus, usually owing to delay in diagnosis. Inversion of uterus Very rarely, if misapplied pressure has been used on the uterine fundus or traction on the cord of a non-separated placenta in a multiparous woman, the uterus can dimple and invert. This is a very shocking event as the fundus turns inside out and goes through the cervix into the vagina. Treatment requires an experienced obstetrician, who will try to return the uterus under general anaesthesia. This can be very difficult. Infection After delivery the genital tract has several sites of potential ingress of bacteria. The placental bed itself is a large raw area, and ascending infection from the lower genital tract may be assisted by previous intrauterine procedures—for example, forceps delivery. Infection of the cervix or, uncommonly, of the episiotomy site, may also occur; the breast can also be a site of infection in the puerperium. Treating infections •Infections manifest themselves by local inflammation (swelling and tenderness) and a raised temperature •Treatment is local heat to the area, analgesia, and broad spectrum antibiotics until the results of bacteriological swabs are available •Co-amoxiclav and erythromycin are both good choices because they deal with penicillinase-producing staphylococci and streptococci, especially group B •Metronidazole is often added for uterine infections •If the infection persists, anaemia may follow, which may ultimately require a blood transfusion Psychological conditions Pregnancy and childbirth are times of high psychological stimulation. Any pre-existing psychological disorder may be exaggerated at this time and requires treatment. Many women go through mood swings (blues) in relation to childbirth, which can usually be managed by sympathetic support. If postnatal depression persists for a week or so, mild antidepressants may be needed, and the Edinburgh postnatal depression questionnaire may be helpful in diagnosing the condition. If the condition continues, formal psychiatric help is needed. Three levels of psychiatric state associated with childbirth Postpartum blues (1 in 5 mothers) •Transient and treatable by reassurance Puerpural depression (1 in 10 mothers) •Low mood, lack of energy, guilt, irritability, and insomnia •Treated by counselling (midwives and health visitors) •Antidepressants—refer to GP if depression continues Puerpural psychosis (1 in 500 mothers) •Affective, depressive, or manic behaviour; insomnia; confusion; perplexity •Refer to psychiatrist and admit to mother and baby unit At the extreme of the spectrum of disease a puerperal psychosis may occur; both the mother and her baby should be admitted to a dedicated maternity/psychiatric unit as both are at risk. Here the mother can have expert psychiatric nursing and medical care while looking after her own baby. There is a 25% risk of recurrence in a future pregnancy. Stillbirth and intrauterine death In _______ 3-4 babies per 1000 are stillborn and another 3-4 per 1000 die in the first week of life. The grief reactions in both the woman and her partner need careful management by the midwifery and medical staff. The couple may go through a phase of anger; all hospital and community staff should be trained to cope with this. Midwifery and medical staff must be prepared to listen and offer their sympathies without attributing blame. Parents should be encouraged to agree to a postmortem examination of the fetus and placenta by a skilled paediatric pathologist. Getting permission for this from the couple requires sensitivity. If a full postmortem examination is declined, a limited examination of the baby may be acceptable (x ray examination, computed tomography, blood samples from the heart area for chromosome analysis, and bacteriological swabbing of the relevant areas of the body). Cultural attitudes of the parents influence these decisions and must be respected. It is probable that the couple will not object to full histological examination of the placenta. Here are further guidelines. |
|
Adnexal torsion Tubo-ovarian abscess, hemorrhagic ovarian cysts Gynecologic hemorrhage Vulvovaginal trauma. |
Neurosurgical Emergencies
Neurological surgery emergencies
|
Subarachnoid hemorrhage Intracranial Hemorrhage Brain AVM (arteriovenous malformation) Spine Fracture CaudaEquina Penetrating Injury Intracranial Lesions –Focal Open Skull fracture Head Trauma Cushing response Epidural Hematomas Epidural Hemorrhage Uncal Herniation Pituitary Adenoma Pituitary apoplexy Traumatic Compression Fracture Jumped facets Ballistic trauma or gunshot wound (GSW) Shunt malfunction T7-8 corptectomyand T6-T9 fusion Cord compression Clinical signs of high ICP Here are further guidelines. |
New Surgical Technique
|
General surgery |
| Orthopaedic surgery |
| Urology |
| Neurosurgery |
| Plastic Surgery |
|
Surgical Skills
Do you know various surgical skills? What are various surgical skills? What is a surgical technique? A systematic surgical procedure by which a medical condition is treated. What questions should you answer in case you introduce new surgical technique? Is this a new surgical technique or already listed in surgical skills practiced by others on human beings? New Surgical Technique Is there any specific name for this new surgical technique? What is the name of this new surgical technique? Have you discussed with other doctors the benefits, complications, and harms due to this new surgical technique? For what type of patients is diagnosis and treatment with this new surgical technique useful? How is this surgical technique going to improve the condition of the patient? How is this surgical technique performed, from beginning to end? For what medical condition is this surgical technique the only option of treatment? What issues is this medical condition causing the patient? What complications can occur due to this surgical technique? |
Orthopaedic surgery emergencies
|
Top 10 pediatric orthopaedic surgical emergencies: a case-based approach for the surgeon on call. Pediatric patients who require orthopaedic surgical emergency care are often treated by orthopaedic surgeons who primarily treat adult patients. Essential information is needed to safely evaluate and treat the most common surgical emergencies in pediatric patients, including hip fractures; supracondylar humeral, femoral, and tibial conditions of the hip (such as slipped capital femoral epiphysis and septic arthritis); and limb- and life-threatening pathologies, including compartment syndrome, the dysvascular limb, cervical spine trauma, and the polytraumatized child. Open fractures (bone is exposed outside of a wound) Open Fractures or Joints Fractures with joint involvement Isolated breaks Stress fractures Multiple fractures Non-union fractures (fractures that do not heal) Malunion fractures (fractures that heal incorrectly) Acute Compartment Syndrome Neurovascular injuries Joint dislocations Ligament sprains Muscle strains Tendon injuries Septic Joints Cauda Equina Syndrome Here are further guidelines. |
Fractures
Open Fractures
| Annotation of definition | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Cause | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Symptoms | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Diagnosis and Treatment | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Description | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Doctor Examination and Initial Treatment | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Gustilo Classification for Open Fractures | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Treatment | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Complications | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Osteology | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Skeletal System | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Recovery | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Prevention | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Research | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|
What are Fractures? A fracture is the medical term for a broken bone. What are common types of fractures? 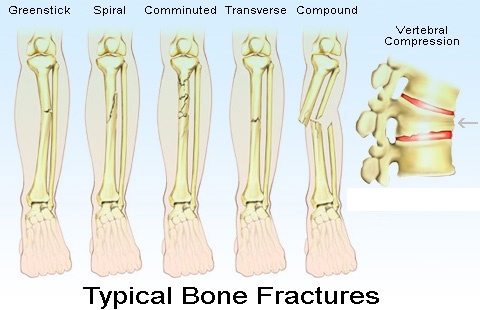

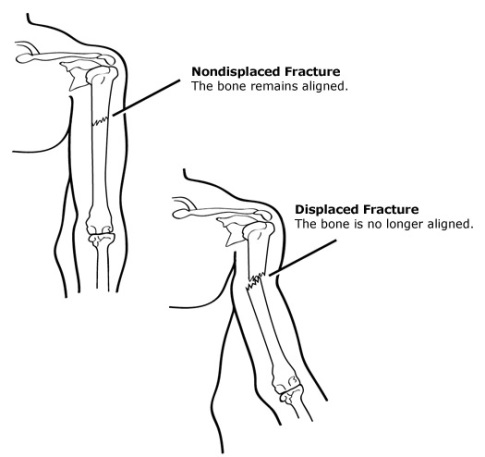

Some fracture types are: • A Greenstick fracture is an incomplete fracture in which the bone is bent. This type occurs most often in children. • A transverse fracture is when the broken piece of bone is at a right angle to the bone's axis. • An oblique fracture is when the break has a curved or sloped pattern. • A comminuted fracture is when the bone breaks into several pieces. • A buckled fracture, also known as an impacted fracture, is one whose ends are driven into each other. This is commonly seen in arm fractures in children. • A pathologic fracture is caused by a disease that weakens the bones. • A stress fracture is a hairline crack. 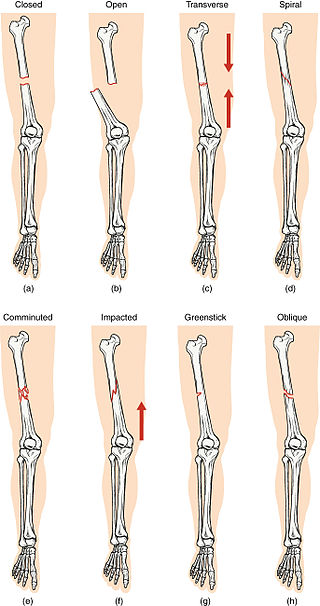 Compare healthy bone with different types of fractures: (a) closed fracture (b) open fracture (c) transverse fracture (d) spiral fracture (e) comminuted fracture (f) impacted fracture (g) greenstick fracture (h) oblique fracture What are the most common types of fractures? The most common types of fractures in older adults are fractures to the pelvis, hip, femur, vertebrae, humerus, hand, forearm, leg, and ankle. What is an open (compound) fracture? An open (or compound) fracture occurs when the skin overlying a fracture is broken, allowing communication between the fracture and the external environment. What is Human Anatomy? How will study of this subject help in diagnosis of human medical conditions, medical advice as per international standards and recent advances, as per preventive and curative concepts of medicine? Let's examine this question. Which splints and casts should be used for various injuries? What bones, muscles, arteries, veins, nerves, are associated with this injury or fracture? Which structures and movements are affected with this injury or fracture? What will happen if you don't immediately manage an injury or fracture? Where and when will you use a nail, screw, rod, plate in fixation of a fracture? This is an orthopedics question. To answer this question correctly. You have to know about human bones, muscles, arteries, veins, nerves and all related subjects. What are the most common fractures? How many total fracture cases were reported every year from last 20 years? What are the most common fractures reported at your hospital every year? How many reported fractures were operated? How many developed post operative deformities? Do you know anyone who developed post operative deformity? Did you developer any post operative deformity? Bones How many bones are in the human body? What is the longest bone in the human body? What is the smallest bone in the human body? What are the bones of upper limb? What are the bones of lower limb? What comes under axial skeleton? What muscles originate from each bone? What are the main foramen of base of skull? What structures pass through each foramen? How do bones form? How do bones grow? What types of cells form bone? What is the structure of bone? What materials make up bone? How do muscles attach to bones? What is the function of bone? What are the differences between a human skeleton and a chimpanzee skeleton? Why do teeth come in different shapes? How long does it take a bone to heal normally after a fracture? What is the difference between a splint and a cast? Which splints and casts should be used for various injuries? How each is applied? What should be proper position of the injured extremity? Why is this the proper position of the injured extremity? Muscles of upper limb What are the muscles that move the glenohumeral joint? What is axial skeleton? What are the muscles originating on axial skeleton? What are the muscles originating on scapula? What are the muscles that move the scapula? How can the deltoid muscle both extend and flex the arm? What are the arm muscles that move the elbow joint or forearm? What are the types of movement? What are the hand muscles? What is the origin, insertion, nerve supply and type of movement? What movements are associated with this muscle? How does exercise help build muscles? Cranial nerves How many total cranial nerves are there? What is the location of the nucleus of cranial nerves? What is the pathway from the nucleus to the nerve supply? How many spinal nerves are there? Blood What are the constituents of human blood? What is hematopoiesis? Where are hematopoietic stem cells located? What are the different types and functions of blood cells? Why and how does total cell count increase during infection? Here are further guidelines. Cause The most common causes of fractures are: • Trauma. A fall, a motor vehicle accident, or a tackle during a football game can all result in fractures. • Osteoporosis. This disorder weakens bones and makes them more likely to break. • Overuse. Repetitive motion can tire muscles and place more force on bone. This can result in stress fractures. Stress fractures are more common in athletes. Symptoms Many fractures are very painful and may prevent you from moving the injured area. Other common symptoms include: •Swelling and tenderness around the injury •Bruising •Deformity — a limb may look "out of place" or a part of the bone may puncture through the skin Doctor Examination Your doctor will do a careful examination to assess your overall condition, as well as the extent of the injury. He or she will talk with you about how the injury occurred, your symptoms, and medical history. The most common way to evaluate a fracture is with x-rays, which provide clear images of bone. Your doctor will likely use an x-ray to verify the diagnosis. X-rays can show whether a bone is intact or broken. They can also show the type of fracture and exactly where it is located within the bone. Treatment Medication Splint Cast (or brace) Traction Internal fixation - implantation of plates, screws, pins and rods to set bones and facilitate healing External fixation – pins, screws and rods placed outside the body to set bones and facilitate healing. External fixators are sometimes used prior to surgical treatment. Surgery, including minimally invasive surgery performed through small incisions Bone stimulator (non-surgical) and bone grafting (surgical) for non-union fractures Evaluation of non-union fractures to identify why a bone did not heal correctly. For example factors such as diabetes, smoking or a thyroid condition may affect a bone’s ability to heal. Splint Commonly used splints Sugar Tong - Used for the forearm or wrist. They are named "sugar-tong" due to their long, U-shaped characteristics, similar to a type of utensil used to pick up sugar cubes Ulnar Gutter - Used for the forearm to the palm Volar Wrist Splint - Used for the wrist Thumb Spica - Used for the thumb Posterior Lower Leg Posterior Full Leg Posterior Elbow Finger Splints - Used for the fingers Ankle Stirrup - Used for the ankles Wrist/arm splint - Used for the wrist or arm Nasal splint Cast (or brace) Cast Types and Maintenance Instructions What is a cast? A cast holds a broken bone in place as it heals. Casts also help to prevent or decrease muscle contractions, and are effective at providing immobilization, especially after surgery. Casts immobilize the joint above and the joint below the area that is to be kept straight and without motion. For example, a child with a forearm fracture will have a long arm cast to immobilize the wrist and elbow joints. What are casts made of? The outside, or hard part of the cast, is made from two different kinds of casting materials. •Plaster (white in color) •Fiberglass (comes in a variety of colors, patterns, and designs) Cotton and other synthetic materials are used to line the inside of the cast to make it soft and to provide padding around bony areas, such as the wrist or elbow. Special waterproof cast liners may be used under a fiberglass cast, allowing the child to get the cast wet. Consult your child's doctor for special cast care instructions for this type of cast. What are the different types of casts? Below is a description of the various types of casts, the location of the body they are applied, and their general function. Type of cast Location Uses Short arm cast Long arm cast Arm cylinder cast
Type of cast Location Uses Shoulder spica cast Minerva cast Short leg cast Leg cylinder cast
Type of cast Location Uses Unilateral hip spica cast One and one-half hip spica cast Bilateral long leg hip spica cast
 Type of cast Location Uses Short leg hip spica cast
 Type of cast Location Uses Abduction boot cast
 How can your child move around while in a cast? Assistive devices for children with casts include: •Crutches •Walkers •Wagons •Wheelchairs •Reclining wheelchairs Cast care instructions •Keep the cast clean and dry. •Check for cracks or breaks in the cast. •Rough edges can be padded to protect the skin from scratches. •Do not scratch the skin under the cast by inserting objects inside the cast. •Can use a hairdryer placed on a cool setting to blow air under the cast and cool down the hot, itchy skin. Never blow warm or hot air into the cast. •Do not put powders or lotion inside the cast. •Cover the cast while your child is eating to prevent food spills and crumbs from entering the cast. •Prevent small toys or objects from being put inside the cast. •Elevate the cast above the level of the heart to decrease swelling. •Encourage your child to move his or her fingers or toes to promote circulation. •Do not use the abduction bar on the cast to lift or carry the child. Older children with body casts may need to use a bedpan or urinal in order to go to the bathroom. Tips to keep body casts clean and dry and prevent skin irritation around the genital area include the following: •Use a diaper or sanitary napkin around the genital area to prevent leakage or splashing of urine. •Place toilet paper inside the bedpan to prevent urine from splashing onto the cast or bed. •Keep the genital area as clean and dry as possible to prevent skin irritation. When to call your child's doctor Contact your child's doctor or healthcare provider if your child develops one or more of the following symptoms: •Fever as directed by your healthcare provider or: • Your child is younger than 12 weeks and has a fever of 100.4°F (38°C) or higher because your baby may need to be seen by their healthcare provider. • Your child has repeated fevers above 104°F (40°C) at any age. • Your child is younger than 2 years old and their fever continues for more than 24 hours or your child is 2 years old and older and their fever continues for more than 3 day •Increased pain •Increased swelling above or below the cast •Decreased ability to move extremity in the cast •Complaints of numbness or tingling •Drainage or foul odor from the cast •Cool or cold fingers or toes •If the cast becomes wet or soiled •Blister, sores, or rash develop under the cast All forms of treatment of broken bones follow one basic rule: the broken pieces must be put back into position and prevented from moving out of place until they are healed. In many cases, the doctor will restore parts of a broken bone back to the original position. The technical term for this process is "reduction." Broken bone ends heal by "knitting" back together with new bone being formed around the edge of the broken parts. Surgery is sometimes required to treat a fracture. The type of treatment required depends on the severity of the break, whether it is "open" or "closed," and the specific bone involved. For example, a broken bone in the spine (vertebra) is treated differently from a broken leg bone or a broken hip. Doctors use a variety of treatments to treat fractures: About Casts Casts and splints support and protect injured bones and soft tissue. When you break a bone, your doctor will put the pieces back together in the right position. Casts and splints hold the bones in place while they heal. They also reduce pain, swelling, and muscle spasm. Splints and casts are sometimes applied after surgery. What are the different kinds of casts? A cast, which keeps a bone from moving so it can heal, is essentially a big bandage that has two layers — a soft cotton layer that rests against the skin and a hard outer layer that prevents the broken bone from moving. These days, casts are made of either: •plaster of paris: a heavy white powder that forms a thick paste that hardens quickly when mixed with water. Plaster of paris casts are heavier than fiberglass casts and don't hold up well in water. •synthetic (fiberglass) material: made out of fiberglass, a kind of moldable plastic, these casts come in many bright colors and are lighter. The covering (fiberglass) on synthetic casts is water-resistant, but the padding underneath is not. You can, however, get a waterproof liner. The doctor putting on the cast will decide whether a fiberglass cast with a waterproof lining is appropriate. Orthopedic cast Cast types Upper extremity casts Lower extremity casts Cylinder cast Body casts EDF cast Spica cast Mobility and hygiene Other casts Cast-cutting Removal of Plaster Casts How is a cast put on? First, several layers of soft cotton are wrapped around the injured area. Next, the plaster or fiberglass outer layer is soaked in water. The doctor wraps the plaster or fiberglass around the soft first layer. The outer layer is wet but will dry to a hard, protective covering. Doctors sometimes make tiny cuts in the sides of a cast to allow room for swelling. Can plaster of paris casts get wet? Absolutely not! A wet cast may not hold the bone in place because the cast could start to dissolve in the water and could irritate the skin underneath it, possibly leading to infection. So your child shouldn't swim and should use a plastic bag or special sleeve (available online or sometimes at pharmacies) to protect the cast from water. And instead of a shower, your child may need to take a sponge bath. Can synthetic (fiberglass) casts get wet? Although the fiberglass itself is waterproof, the padding inside a fiberglass cast is not. So it's still important to try to keep a fiberglass cast from getting wet. If this is a problem, talk to the doctor about getting a waterproof liner. Fiberglass casts with waterproof liners let kids continue bathing or even go swimming during the healing process. Although the liner allows for evaporation of water and sweat, it's still fragile. Also, only certain types of breaks can be treated with this type of cast. Your doctor will determine if the fracture may be safely treated with a waterproof cast. Cast Immobilization A plaster or fiberglass cast is the most common type of fracture treatment, because most broken bones can heal successfully once they have been repositioned and a cast has been applied to keep the broken ends in proper position while they heal. Functional Cast or Brace The cast or brace allows limited or "controlled" movement of nearby joints. This treatment is desirable for some, but not all, fractures. Traction Traction is usually used to align a bone or bones by a gentle, steady pulling action. External Fixation In this type of operation, metal pins or screws are placed into the broken bone above and below the fracture site. The pins or screws are connected to a metal bar outside the skin. This device is a stabilizing frame that holds the bones in the proper position while they heal. In cases where the skin and other soft tissues around the fracture are badly damaged, an external fixator may be applied until surgery can be tolerated. 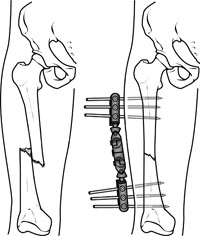 An external fixator applied to a broken thighbone. Open Reduction and Internal Fixation During this operation, the bone fragments are first repositioned (reduced) in their normal alignment, and then held together with special screws or by attaching metal plates to the outer surface of the bone. The fragments may also be held together by inserting rods down through the marrow space in the center of the bone. 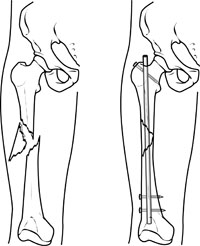 A specially designed metal rod, called an intramedullary nail, provides strong fixation for this thighbone fracture.  Recovery Fractures take several weeks to several months to heal, depending on the extent of the injury and how well you follow your doctor's advice. Pain usually stops long before the fracture is solid enough to handle the stresses of normal activity. Even after your cast or brace is removed, you may need to continue limiting your movement until the bone is solid enough for normal activity. During your recovery you will likely lose muscle strength in the injured area. Specific exercises will help you restore normal muscle strength, joint motion, and flexibility. Prevention Preventing Falls and Related Fractures Several factors can lead to a fall. Loss of footing or traction is a common cause of falls. Loss of footing occurs when there is less than total contact between one’s foot and the ground or floor. Loss of traction occurs when one’s feet slip on wet or slippery ground or floor. Other examples of loss of traction include tripping, especially over uneven surfaces such as sidewalks, curbs, or floor elevations that result from carpeting, risers, or scatter rugs. Loss of footing also happens from using household items intended for other purposes – for example, climbing on kitchen chairs or balancing on boxes or books to increase height. A fall may occur because a person’s reflexes have changed. As people age, reflexes slow down. Reflexes are automatic responses to stimuli in the environment. Examples of reflexes include quickly slamming on the car brakes when a child runs into the street or quickly moving out of the way when something accidentally falls. Aging slows a person’s reaction time and makes it harder to regain one’s balance following a sudden movement or shift of body weight. Improving Balance Do muscle-strengthening exercises. Obtain maximum vision correction. Practice using bifocal or trifocal glasses. Practice balance exercises daily. Changes in muscle mass and body fat also can play a role in falls. As people get older, they lose muscle mass because they have become less active over time. Loss of muscle mass, especially in the legs, reduces one’s strength to the point where she or he is often unable to get up from a chair without assistance. In addition, as people age, they lose body fat that has cushioned and protected bony areas, such as the hips. This loss of cushioning also affects the soles of the feet, which upsets the person’s ability to balance. The gradual loss of muscle strength, which is common in older people but not inevitable, also plays a role in falling. Muscle-strengthening exercises can help people regain their balance, level of activity, and alertness no matter what their age. Changes in vision also increase the risk of falling. Diminished vision can be corrected with glasses. However, often these glasses are bifocal or trifocal so that when the person looks down through the lower half of her or his glasses, depth perception is altered. This makes it easy to lose one’s balance and fall. To prevent this from happening, people who wear bifocals or trifocals must practice looking straight ahead and lowering their head. For many other older people, vision changes cannot be corrected completely, making even the home environment hazardous. Safety first to prevent falls: At any age, people can change their environments to reduce their risk of falling and breaking a bone. Outdoor safety tips: In nasty weather, use a walker or cane for added stability. Wear warm boots with rubber soles for added traction. Look carefully at floor surfaces in public buildings. Many floors are made of highly polished marble or tile that can be very slippery. If floors have plastic or carpet runners in place, stay on them whenever possible. Identify community services that can provide assistance, such as 24-hour pharmacies and grocery stores that take orders over the phone and deliver. It is especially important to use these services in bad weather. Use a shoulder bag, fanny pack, or backpack to leave hands free. Stop at curbs and check their height before stepping up or down. Be cautious at curbs that have been cut away to allow access for bikes or wheelchairs. The incline up or down may lead to a fall. Indoor safety tips: Keep all rooms free from clutter, especially the floors. Keep floor surfaces smooth but not slippery. When entering rooms, be aware of differences in floor levels and thresholds. Wear supportive, low-heeled shoes, even at home. Avoid walking around in socks, stockings, or floppy, backless slippers. Check that all carpets and area rugs have skid-proof backing or are tacked to the floor, including carpeting on stairs. Keep electrical and telephone cords and wires out of walkways. Be sure that all stairwells are adequately lit and that stairs have handrails on both sides. Consider placing fluorescent tape on the edges of the top and bottom steps. For optimal safety, install grab bars on bathroom walls beside tubs, showers, and toilets. If you are unstable on your feet, consider using a plastic chair with a back and nonskid leg tips in the shower. Use a rubber bath mat in the shower or tub. Keep a flashlight with fresh batteries beside your bed. Add ceiling fixtures to rooms lit by lamps only, or install lamps that can be turned on by a switch near the entry point into the room. Another option is to install voice- or sound-activated lamps. Use bright light bulbs in your home. If you must use a step-stool for hard-to-reach areas, use a sturdy one with a handrail and wide steps. A better option is to reorganize work and storage areas to minimize the need for stooping or excessive reaching. Consider purchasing a portable phone that you can take with you from room to room. It provides security because you can answer the phone without rushing for it and you can call for help should an accident occur. Don’t let prescriptions run low. Always keep at least 1 week’s worth of medications on hand at home. Check prescriptions with your doctor and pharmacist to see if they may be increasing your risk of falling. If you take multiple medications, check with your doctor and pharmacist about possible interactions between the different medications. Arrange with a family member or friend for daily contact. Try to have at least one person who knows where you are. If you live alone, you may wish to contract with a monitoring company that will respond to your call 24 hours a day. Watch yourself in a mirror. Does your body lean or sway back and forth or side to side? People with decreased ability to balance often have a high degree of body sway and are more likely to fall. Medications That May Increase the Risk of Falling Unfortunately, as you get older, you're more likely to need daily medications. And all medications have side effects, some of which can increase your risk of having a fall. Medications that can cause dizziness or lack of coordination are: •Sedatives or sleeping pills •Drugs that lower high blood pressure, which can sometimes cause hypotension, blood pressure that is too low • Antidepressants •Anticonvulsants, which are used to treat epilepsy and some psychological conditions •Muscle relaxants, which may be used for back pain or other problems •Some medicines for heart conditions Injury Prevention - Seat Belts Seat Belts Lap/shoulder safety belts, when used correctly, reduce the risk of death to front seat occupants by 45% and risk of moderate to critical injury by 50%. Food and Your Bones Proper diet and exercise may help in preventing some fractures. A diet rich in calcium and Vitamin D will promote bone strength. Weightbearing exercise also helps keep bones strong. Getting the calcium and vitamin D you need is easier than you think -- if you eat the right foods.
|
|
What is emergency surgery? Surgical emergency is a medical emergency which requires immediate surgical intervention (the only way to solve the problem successfully). How should emergency surgeries be classified? Extremely urgent emergency surgery
Urgent emergency surgeries Appendectomy Setting of a broken bone that needs internal setting What cases need emergency surgery? What cases need an emergency operating room (OR)? The following conditions are surgical emergencies: Acute trauma Amputation Acute appendicitis(Is acute appendicitis a surgical emergency? Urgent appendectomy has become the basis of management for acute appendicitis because of the disparity in morbidity and mortality rates between perforated and nonperforated appendicitis.) Abscesses Aortic dissection Acute subdural hematoma Acute airway obstruction Acute mesenteric ischemia Bleeding ectopic pregnancy Bowel obstruction Cardiac tamponade Cholecystitis (gallbladder infection) Diverticulitis Gastrointestinal perforation Incarcerated hernia Intestinal blockage/obstruction Intestinal volvulus Internal bleeding Limb ischemia Neuroendocrine tumors causing acute homeostatic imbalance unresponsive to medication (often due to decompensation) Pneumothorax Paraphimosis Peritonitis Ruptured intestine Ruptured aortic aneurysm Retinal detachment Retained abortion Spleen Removal Stercoral perforation Thrombosed hemorrhoids Testicular torsion Urinary retention (not respond to other medical treatment) |
Congenital Nontraumatic Pediatric Surgical Emergencies Pediatric Trauma Nontraumatic Pediatric Surgical Emergencies Cardiothoracic Gastrointestinal Genitourinary Gynaecological Neurological/Ophthalmic Vascular |
Diagnosis accuracy importance.
|
Why is diagnosis accuracy essential to any physician surgeon medical emergency, physician surgeon elective surgery? We will take an example of acute abdominal pain. There are more than 22 causes of acute abdominal pain. Acute abdominal pain can represent a spectrum of conditions from benign and self-limited disease to surgical emergencies. Out of more than 22 causes of acute abdomen, only two causes of acute abdomen need surgical intervention under verified conditions of seniors. Do not go ahead with surgery without second and third consultation from senior physicians for verification of diagnosis and appropriate treatment. |
Surgical Skills
|
Do you know various surgical skills? What are various surgical skills? What is a surgical technique? A systematic surgical procedure by which a medical condition is treated. Here are further guidelines. |
Seniority
|
What should other physicians who claim to be surgeons know? Physician surgeon medical emergency Physician surgeon elective surgery These are the only two types of entities of physicians with surgical abilities. How should seniority of physician surgeon medical emergency, physician surgeon elective surgery be categorized? Guide to physician surgeon medical emergency, physician surgeon elective surgery is most senior, for example the individual circulating these guidelines www.qureshiuniversity.com/surgeryworld.html Doctor Asif Qureshi. You must know Doctor Asif Qureshi guides at least 812 other various professions, for example www.qureshiuniversity.com/professionsworld.html Do not expect Doctor Asif Qureshi to reach out to your operating room and, for example, in cholecystectomy for gallstones do 8-inch Incision, clamp at two ends of gall bladder, cut, suture the stump, and close in 3 layers. Juniors have to perform these services. Do not expect Doctor Asif Qureshi to reach out to medical emergency room and, for example, trauma with head injury with scalp laceration that needs closure in 2 layers of two ends of lacerated scalp. Juniors have to perform these services. Doctor Asif Qureshi has done these services while he was a junior physician. If you do not understand anything from www.qureshiuniversity.com/surgeryworld.html you are encouraged to ask questions. Consultant physician surgeon medical emergency, physician surgeon elective surgery. Senior resident physician surgeon medical emergency, physician surgeon elective surgery. Junior resident physician surgeon medical emergency, physician surgeon elective surgery. How many subcategories of surgeries are there? 14 subcategories of surgical categories have to be recognized that can be emergency or elective. What should physician surgeon medical emergency know? You have to know everything of these entities. What should physician surgeon elective surgery know? You have to know everything of these entities. How are other regions categorizing surgical categories? In some regions, even anethesiologist is expected to have physician surgeon medical emergency, physician surgeon elective surgery abilities. Here are various subcategories of surgery in other regions that needs to be updated.
|
| Surgery: Is it really indicated? |
|
A statement mentions that the surgery department lacks equipments and infrastructure. What type of equipment do you need? If you audit existing surgeries, you will discover that most of them are not required, and there has been wrong clinical diagnosis. A diagnosis of appendicitis: on operation, no findings of appendicitis. A diagnosis of cholecystitis or cholelithiasis: on operation, no findings of cholecystitis or cholelithiasis. A medical doctor is required to make correct clinical diagnoses. A surgeon is basically a medical doctor. They ask for number of unwanted investigations but after that they still cannot reach a correct diagnosis and treatment. |
|
Q: Who is a surgeon? A: A surgeon is a medical doctor with additional training in specific medical procedures. Getting the title of surgeon does not mean he or she is a competent medical doctor. Not all surgeons can perform all medical procedures. Not all medical doctors can perform all medical procedures. Making an eight-inch incision and closing in three layers does not prove you are a surgeon or a medical doctor. Doing a burr hole and closing does not prove you are a surgeon. This is a medical or surgical procedure that can be taught in a few weeks. Doing medical or surgical procedures does not prove you are a competent medical doctor. The ability to reach to a correct diagnosis and provide treatment is a requirement of all medical doctors while maintaining good character and good behavior. |
| Surgical Skills |
|
A-Z Surgical Specialties What are the surgical specialties? |
| What type of suggestions should a medical doctor (MD) forward to improve training programs in health care and medical education? |
| What do you have to do in case you need to be a surgeon? |
| What questions should a medical doctor or surgeon ask an anesthetist? |
|
What are the different types of surgery? What are the surgical specialties? |
Neurosurgery
Q: What is a neurosurgeon? Q: Who sees a neurosurgeon? Q: What might neurological care involve? Q: What areas of care are available? Q: Who is a neurosurgeon? Q: What does neuroscience care involve? Q: Where is the neuroscience patient cared for? Q: What medical conditions require brain surgery? Q: What risks are associated with brain surgery? Q: How is brain surgery done? Q: What are other names for brain surgery? Here are further guidelines. |
Cardiothoracic surgery
Q: What is an MCh in cardiovascular and thoracic surgery? Q: How many MCh's in cardiovascular and thoracic surgery are required in the state? Q: What skills and knowledge are needed for an MCh in cardiovascular and thoracic surgery? Q: What are the duties and responsibilities of a person with an MCh in cardiovascular and thoracic surgery? Q: What equipment does cardiovascular and thoracic surgery need? Q: What other resources does cardiovascular and thoracic surgery need? Here are further guidelines. |
| Oral and maxillofacial surgery |
| Otolayrngology |
| Eye Surgery |
| OB/GYN Surgery |
| Paediatric surgery |
| Plastic Surgery |
| Orthopaedic surgery |
| Urology |
|
General surgery
Do all cases of appendicitis need surgery? Do all cases of cholecystitis or gallstones need surgery? Dr. Qureshi's technique Q: What are the advantages of laparoscopy? A: It is less invasive, cost effective, results in fewer infections, and shorter hospital stay. Also, early return to work, minimal postoperative complications, and cosmetic advantages, too. Can appendicitis be managed with endoscopic/Laparoscopy removal without general anesthesia? Q: What does the surgeon use to close the wound? Q: What is the difference between sutures, staples and Steri-Strips? Q: Do all sutures dissolve? Q: Is it painful to have sutures and staples removed? Q: How is the wound bandaged? Q: How should I care for my wound? Q: Is it normal for the wound to itch? Q: How do I take care of my wound at home? Q: When can I take a shower? Q: Does it take a long time for the wound to heal? Do you have a question? Can you make me wiser? How? Can you make us wiser? How? Would you like to add anything? Who among you has done laparoscopic surgery? How many surgeries have you done so far? What was the diagnosis? What were the indications? What were the results? Were there any post- procedure complications? What were these complications? What is been done to prevent these complications? Who is the manufacturer of the equipment? What is the material of the existing equipment? What is been done to enhance the efficiency of a laparoscopy? What is been done to train others? Who has the responsibility to fund this research and development? |
|
Surgical Skills
Do you know various surgical skills? What are various surgical skills? What is a surgical technique? A systematic surgical procedure by which a medical condition is treated. What questions should you answer in case you introduce new surgical technique? Is this a new surgical technique or already listed in surgical skills practiced by others on human beings? New Surgical Technique Is there any specific name for this new surgical technique? What is the name of this new surgical technique? Have you discussed with other doctors the benefits, complications, and harms due to this new surgical technique? For what type of patients is diagnosis and treatment with this new surgical technique useful? How is this surgical technique going to improve the condition of the patient? How is this surgical technique performed, from beginning to end? For what medical condition is this surgical technique the only option of treatment? What issues is this medical condition causing the patient? What complications can occur due to this surgical technique? Why was there a need to elaborate on these facts? On September 12, 2013, Department of Surgical Gastroenterology SKIMS started sophisticated pancreatic surgery, pancreaticoduodenectomy with portal venous resection and later reconstruction. A team of surgeons headed by Prof. Omar Javed Shah was the first of its kind in Kashmir. The above questions were not answered in the academic deliberations. Here are further guidelines. |
Surgical Emergencies
| In case of any surgical recommendations, get second and third consultation immediately from supervisors before any surgical recommendations. |
| Anesthesia |
Surgical Instruments
|
How many surgical instruments are there for human surgery? There are hundreds of surgical instruments for human surgery. Can you name various surgical instruments? Instruments used in general surgery. What are six classes of surgical instruments by functions? Six classes of surgical instruments by function. 1. Cutting surgical instruments 2. Grasping or holding surgical instruments 3. Haemostatic forceps surgical instruments (instruments used to stop blood flow) 4. Retractors surgical instruments 5. Clamps and distractors surgical instruments 6. Accessories and implants surgical instruments What minimum resources are required by physician surgeon medical emergency and physician surgeon elective surgery in general surgery emergency or elective surgery? 1. Surgical needle holder 2. Surgical needle with thread 3. Scalpel 4. Haemostatic forceps 5. Suction tips and tubes 6. Dressing (medical) 7. Surgical table 8. Physician for assistance 9. General anesthesia (anesthetist) 10. Guide, for example Doctor Asif Qureshi at www.qureshiuniversity.com/surgeryworld.html from a distance. If any juniors or students are around, this must be recorded. In various surgeries other than general surgery emergency or elective, these surgery resources are required plus some extra surgical instruments. Nowadays, computer and Internet with guidelines at www.qureshiuniversity.com/surgeryworld.html are essential. What are several classes of surgical instruments? There are several classes of surgical instruments: Graspers, such as forceps Clamps and occluders for blood vessels and other organs Retractors, used to spread open skin, ribs, and other tissue Distractors, positioners and stereotactic devices Mechanical cutters (scalpels, lancets, drill bits, rasps, trocars, Ligasure, Harmonic scalpel, surgical scissors, rongeurs etc.) Dilators and specula, for access to narrow passages or incisions Suction tips and tubes, for removal of bodily fluids Sealing devices, such as surgical staplers Irrigation and injection needles, tips and tubes, for introducing fluid Powered devices, such as drills, dermatomes Scopes and probes, including fiber optic endoscopes and tactile probes Carriers and appliers for optical, electronic, and mechanical devices Ultrasound tissue disruptors, cryotomes, and cutting laser guides Measurement devices, such as rulers and calipe Cardiothoracic surgery, neurosurgery, orthopedic surgery, plastic surgery, other categories have some extra instruments compared to general surgery emergency or elective surgery. |
| Inside operating room |
|
Is there a difference between operating room equipment and surgical instruments? Yes, there is. What are examples of operating room equipments? What are examples of surgical instruments? |
| Operating Room Equipment |
| Operating room management |
| Operating Room Skills |
| Operating Room Skills Checklist |
| Surgical instruments |
| Surgical Documentation |
| Patients |
| Surgery |
| Surgical Procedures |
| Elective surgery |
| Surgical Skills |
| Surgery |
|
What is emergency surgery? How should emergency surgeries be classified? What cases need emergency surgery? What cases need an emergency operating room (OR)? What cases need elective surgery? What cases need an elective operating room (OR)? What are examples of emergency surgeries? Is there a difference between operating room equipment and surgical instruments? What are examples of operating room equipments? What are examples of surgical instruments? |
Physician surgeon elective surgery
| What should physician surgeon elective surgery know? | ||
| Annotation or definition of elective surgeries. | ||
| Basic abilities of a physician primary care, physician medical emergency room. | ||
| Surgical skills. | ||
| Seniority | ||
| Questions that need answers before, during, and after surgical procedure. | ||
| Types of elective surgeries. | ||
| Operating room equipment | ||
| Operating room management | ||
| Operating room skills | ||
| Operating room skills checklist | ||
| Patients | ||
| Surgical instruments | ||
|
Annotation or definition of elective surgeries.
Elective surgery
|
Surgical incision
|
Alert for all physicians.
In what situations in surgical emergencies or elective procedures is incision not required? If there is any stab wound that caused prolapse of intestines, do not do any incision. Do not do any laparotomy. Do not cut any site or location in this situation. Relocate the intestines to their original location and suture the stab wound. Critical monitoring of the individual is required. In what situation is surgical incision required? See surgical incisions details. What are the types of surgical incisions? Head and neck Chest Abdomen and pelvis Eye Head and neck Wilde's incision Descriptions of Common Neurosurgical Operations Burr Holes and Craniotomy Anterior Cervical Discectomy and Fusion Lumbar Microdiscectomy Lumbar Decompressive Laminectomy Carpal Tunnel Release Ulnar Nerve Decompression or Transposition Chest I do not recommend Median sternotomy procedures unless the likely advantage to patient is discussed and verified. Median sternotomy - This is the primary incision used for cardiac procedures. It extends from the sternal notch to the xiphoid process. The sternum is divided, and a finochietto retractor used to keep the incision open. Thoracotomy - A division of the ribs from the side of the chest. Abdomen and pelvis Midline incision or midline laparotomy - The most common incision for laparotomy is the midline incision, a vertical incision which follows the linea alba. The upper midline incision usually extends from the xiphoid process to the umbilicus. A typical lower midline incision is limited by the umbilicus superiorly and by the pubic symphysis inferiorly. Sometimes a single incision extending from xiphoid process to pubic symphysis is employed, especially in trauma surgery. Typically, a smooth curve is made around the umbilicus. Pfannenstiel incision - The Pfannenstiel incision, a transverse incision below the umbilicus and just above the pubic symphysis. In the classic Pfannenstiel incision, the skin and subcutaneous tissue are incised transversally, but the linea alba is opened vertically. It is the incision of choice for Caesarean section and for abdominal hysterectomy for benign disease. Chevron incision - This incision a cut is made on the abdomen below the rib cage. The cut starts under the mid-axillary line below the ribs on the right side of the abdomen and continues all the way across the abdomen to the opposite mid-axillary line thereby the whole width of the abdomen is cut to provide access to the liver. The average length of the incision is approximately 24 to 30 inches. Cherney incision - Cherney described a transverse incision that allows excellent surgical exposure to the space of Retzius and the pelvic sidewall. The curvilinear skin and rectus fascial incision is made 2 finger breadths above the symphysis pubis and carried in Langer's lines from 2 fingerbreadths medial to one anterior superior iliac spine to the corresponding position medial to the opposite anterior superior iliac spine. The anterior rectus fascia is mobilized distally off the underlying rectus muscle bodies. The pyramidalis muscles are dissected free and sharply excised to expose the underlying rectus tendons. With an index finger, a plane is developed between the fibrous tendons of the rectus muscle and the underlying transversalis fascia. Using a sharp no.10 scalpel blade, the rectus tendons are transected transversely 1–2 cm distal to the superior edge of the pubic bone. Rectus muscle should never be cut. The rectus muscles are retracted and the peritoneum opened.The inferior epigastric vessels may need division. Closure is accomplished with 5 to 6 horizontal mattress sutures of permanent braided suture approximating the anterior rectus tendons to the intact distal anterior rectus fascia. Continuous monofilament suture closure of lateral edges of the rectus muscle to the anterior rectus fascia prevents hernia. Patients should wear a binder for at least 2 weeks. No incision provides wider pelvic exposure, and is relatively painless compared to midline incisions. Result is the most pleasing cosmetic result of any abdominal incision. Gridiron's incision (Mc Burney's incision) - Described in 1894 by McBurney, used for appendectomy. An oblique incision made in the right lower quadrant of the abdomen, classically used for appendectomy. Incision is placed perpendicular to the spinoumblical line at Mc Burney's point, i.e. at the junction of lateral one-third and medial two-third of spino-umblical line. Kocher’s incision - An oblique incision made in the right upper quadrant of the abdomen, classially used for open cholecystectomy. Named after Emil Theodor Kocher. It is appropriate for certain operations on the liver, gallbladder and biliary tract. This shares a name with the Kocher incision used for thyroid surgery: a transverse, slightly curved incision about 2 cm above the sternoclavicular joints; Kustner’s incision - A transverse incision is made 5 cms above the symphysis pubis but below the anterior iliac spine. The subcutaneous tissue is then separated in the midline and the linea alba is exposed. A vertical midline incision is made through the linea alba. Care is taken to control and ligate any branches of the superficial epigastric vessels. This step of the incision is usually time consuming and is one of the limitations associated. This type of incision offers little extensibility and less exposure than a Pfannestiel incision. Lanz incision - A variation of the traditional Mc Burney's incision, which was made at McBurney's point on the abdomen: The Lanz incision is made at the same point along the transverse plane and deemed cosmetically better. It is typically used to perform an open appendectomy. Variations exist on the method used to locate the incision. Some surgeons advocate that the incision is made approximately 2 cm below the umbilicus centered on mid clavicular-midinguinal line. Others imply use of McBurney's point to center the incision (1/3rd of the distance from the anterior superior iliac spine to the umbilicus). Maylard incision - A variation of Pfannenstiel incision is the Maylard incision in which the rectus abdominis muscles are sectioned transversally to permit wider access to the pelvis.[4] The Maylard incision is also called the Mackenrodt incision. The incision in the rectus muscles is performed with the help of cautery, scalpel or surgical stapler. It is important to identify the inferior epigastric vessels on the lateral surface of these muscles and ensure their isolation and ligation if the incision will span more than half the rectus muscle width. It is advisable not to separate the rectus muscles from the anterior rectus sheath to prevent their retraction, which in turn facilitates closure at the end of the procedure. Among the complications associated with this type of incision is delayed bleeding from the cut edges of the rectus muscles as well as the deep epigastric vessels. Furthermore depending on the patient's body habitus, this incision may not offer adequate exposure to the upper abdomen. McBurney incision - This is the incision used for open appendectomy, it begins 2 to 5 centimeters above the anterior superior iliac spine and continues to a point one-third of the way to the umbilicus (McBurney's point). Thus, the incision is parallel to the external oblique muscle of the abdomen which allows the muscle to be split in the direction of its fibers, decreasing healing times and scar tissue formation. This incision heals rapidly and generally has good cosmetic results, especially if a subcuticular suture is used to close the skin. McEvedy's incision - McEvedy's original incision was a lateral paramedian incision which used to incise the rectus sheath along its lateral margin and gain access by pulling the rectus medially. This incision became obsolete because of very high incisional hernia rate. A modification was introduced by Nyhus which used a transverse (oblique) skin incision 3 cm above the inguinal ligament and a transverse incision (oblique) to divide the anterior rectus sheath. The rectus muscle was then pulled medially. This modification prevented the high incisional hernia rate. Turner-Warwick's incision - This type of incision is placed 2 cm above the symphysis pubis and within the lateral borders of the rectus muscles. The sheath overlying the rectus muscles at the symphysis pubis is released, 4 cm transversely, and the incision angled up to the lateral borders of the rectus muscles. The lateral edges of the incisions remain medial to the internal oblique muscles. The sheath may be released off the aponeurosis with the help of traction applied using Kocker clamps. The pyramidalis muscles are typically left attached to the aponeurosis. The rectus muscles are separated and the incision is made in the midline. This type of incision is good for exposure of the retropubic space but offers limited access to the upper pelvis and abdomen. Eye I do not recommend Mini Asymmetric Radial Keratotomy and Radial keratotomy procedures unless the likely advantage to patient is discussed and verified. Mini Asymmetric Radial Keratotomy -Used in eye surgery to cure keratoconus and correct astigmatism. It consists of a series of microincisions of variable depth, with a length between 1.75 and 2.25 millimeters, always made with a diamond knife, designed to cause a controlled scarring of the cornea, which changes its thickness and shape. Radial keratotomy - Used in eye surgery: corneal microincisions made to flatten the cornea and correct myopia. |
|
What are the types of surgical tables?
There are at least nine types of surgical tables. C-arm tables Examination table Examination table powered Lithotripsy tables Operating room tables Procedure Chairs Ultrasound tables Urology tables Surgical table with table accessories What type of surgical table is required for this surgery procedure? |
|
What are the types of surgical positions?
Supine Lithotomy (stirrups) Prone Jackknife (3500 or 6001) Right lat decubitus (bean bag) Left lat decubitus (bean bag) There are at least 14 positions on a surgical table. Here are further facts.
What should be the position of the patient on the surgical table? |
|
What is the date and time of surgery?
Date: ____________ Time of Surgery: ___________ What is the name, date of birth, identification mark of the patient? -------------------------------------------------------------------- Before anesthesia and surgery, ask patient name, date of birth, and identification mark. What is name of physician surgeon medical emergency or physician surgeon elective surgery? -------------------------------------------------------------------- What best describes the surgery? Emergency Urgent Elective -------------------------------------------------------------------- Who all are included during surgery in surgical procedure? Physician surgeon medical emergency or physician surgeon elective surgery Physician anesthetist medical emergency or elective. Operating room nurse Administrator Guide to all of them for example, Doctor Asif Qureshi www.qureshiuniversity.com/surgeryworld.html. Others. Surgical tables What type of surgical table is required for this surgery procedure? There are at least nine types of surgical tables. -------------------------------------------------------------------- Position on Surgical Table: What should be position of patient on the surgical table? Supine Lithotomy (stirrups) Prone Jackknife (3500 or 6001) Right lat decubitus (bean bag) Left lat decubitus (bean bag) There are at least 14 positions on surgical table. -------------------------------------------------------------------- Surgical incisions. Alert for all physicians. Is there any directive not to give surgical incision? In what situations can surgical incision be or not be given? See situations surgical incision cannot be given or should not be given. What should be the postoperative bed location? Surgical intensive care unit. Postoperative ward. Other location; specify. -------------------------------------------------------------------- How long will the surgical procedure last? Case length (add 15 min for intubated patient): ____________ -------------------------------------------------------------------- What resources are required for this surgical procedure, including surgical instruments? -------------------------------------------------------------------- What best describes pain block for this patient? Pain block: No block Consult Epidural Nerve block Nerve catheter Femoral block Intrascalene block Popliteral block Sciatic block -------------------------------------------------------------------- What is the diagnosis of the patient? --------------------------------------------------- What are the medical or surgical procedure details? --------------------------------------------------- |
Surgical procedure
Questions that need answers before, during, and after surgical procedure.
What questions should be answered before, during and after surgical procedure?
| Questions to be answered before the surgery. |
| Preoperative instructions |
| Questions to be answered in postoperative notes. |
| Questions to be answered in follow-up consultations. |
| If the expected procedure or surgery is likely to harm the patient, do not go ahead with surgery. If all the questions are not answered, do not go ahead with surgery. |
Questions to be answered before the surgery.
|
Preoperative instructions
| Preoperative instructions |
Questions to be answered in postoperative notes.
| Inside operating room |
| Operative notes |
| Postoperative complications |
Questions to be answered in follow-up consultations.
|
How did the patient improve or was helped by the specific procedure or surgery?
In general, how is your physical and mental health? Postoperative follow-up |
Last Updated: January 18, 2016