Attending physician issues.
|
Take a look at this. https://www.qureshiuniversity.org/physicians.html Take a look at this. https://qureshiuniversity.com/primarycarephysician.html If you were an attending physician: What would you add to these resources? How has the internet guidelines from Doctor Asif Qureshi (for example, https://www.qureshiuniversity.org/physicians.html) changed the definition and role of attending physician? In olden days, you would mention that you are an attending physician on your resume. Mentioning that you are an attending physician on your resume, in person, or on the internet is not enough. You must answer relevant questions at least through the Internet. What was and actually should be the role of an attending physician? Attending physicians are doctors who are responsible for supervising, teaching, and training interns, residents, fellows, and medical students. Take a look at this. https://www.qureshiuniversity.org/physicians.html Existing attending physicians cannot display guidelines the way Doctor Asif Qureshi has displayed them. Questions you need to answer at least through the Internet. Do not recognize any person claiming to be attending physician on their resume or in person without answering these questions. What types of physicians can you guide among the physicians listed at https://www.qureshiuniversity.org/physicians.html? Where are the guidelines on the internet that you have authored? Who has authored the guidelines that you are displaying? How long did it take to author these guidelines? Who assisted you when you authored these guidelines? What professions are the guidelines you authored that are available through the Internet relevant to? Careers in Medicine - Residency & Fellowship Program What have been the various findings? 12 entities in Chicago, Illinois 60640 did not display these guidelines on or before August 10, 2019, the way Doctor Asif Qureshi has displayed through the Internet at https://www.qureshiuniversity.org/primarycarephysician.html resources. Who all did not have a standard residency and fellowship program on or before August 10, 2019? University of Illinois College of Medicine at Chicago Program Code 1201621488 Program Type ACGME Swedish Covenant Hospital Program Code 1201600709 Swedish Covenant Hospital Program Code 1201631106 Presence Saints Mary and Elizabeth Medical Center Program Code 1201612693 Presence Saint Joseph Hospital (Chicago) Program Code 1201611103 Presence Resurrection Medical Center Program Code 1201611102 Norwegian American Hospital Program Code 1201600705 Mount Sinai Hospital Medical Center of Chicago Program Code 1201631618 McGaw Medical Center of Northwestern University Program Code 1201612701 Jackson Park Hospital Program Code 1201612363 Cook County Health and Hospitals System Program Code 1201611100 Advocate Health Care Program Code 1201621467 Who is responsible for reminding them to bring their residency and fellowship program up to existing requirements, including through internet the way Doctor Asif Qureshi has displayed (https://www.qureshiuniversity.org/primarycarephysician.html) on or before August 10, 2019? Advocate residency fellowship program. What is the mailing address? Advocate Illinois Masonic Family Medicine Residency 836 W. Wellington Ave Chicago, IL 60657 Phone: 773.296.8250 Fax: 773.296.3425 E-mail: ILMasonicFPR@advocatehealth.com Who must receive these facts? Advocate Health Care Program Code 1201621467 Catherine Plonka, MD Program Director, Family Medicine Residency Clinical Associate Professor, UIC College of Medicine Catherine.Plonka@advocatehealth.com Gina Schueneman, DO Program Director, Osteopathic Family Medicine Residency Gina.Schueneman@advocatehealth.com https://www.advocatehealth.com/education/residency-opportunities/advocate-illinois-masonic-medical-center/residency/family-medicine/ On or before August 1, 2019, the existing curriculum of the Advocate Illinois Masonic Family Medicine Residency Curriculum cannot help specific primary care physicians in the real world. On or before August 11, 2019, most of the Family Medicine Residency Curriculum was not relevant to the real world. ERAS and NRMP must circulate these facts to all. Where are genuine guidelines for specific primary care physicians from Doctor Asif Qureshi? Take a look at this. https://www.qureshiuniversity.org/physicians.html Take a look at this. https://www.qureshiuniversity.org/primarycarephysician.html Can you forward this to them? Take a look at this. https://www.qureshiuniversity.org/physicians.html Take a look at this. https://www.qureshiuniversity.org/primarycarephysician.html Doctor Asif Qureshi’s guidelines for existing primary care physicians and aspiring primary care physicians. Advocate Illinois Masonic Family Medicine Residency Curriculum has to be upgraded to follow the guidelines Doctor Asif Qureshi has provided. They must give recognition of this to the program director. Existing program directors do not need to worry. They will keep their jobs. I will be their guide. Why do you need to forward this to them? In 2005, Social Security and IDHS asked me to use my abilities and skills as a specific physician. For this, I was given some resources. Once I complete them and display them via the internet, this will be reinforced and recognized. I have communicated with Social Security and IDHS regarding these issues. They have not responded. Someone has to reinforce and recognize the guidelines that I have researched for so many years and now display via the internet. I conducted the research to develop these guidelines from June 1, 2005, to August 11, 2019, in Chicago, Illinois 60640. |
|
Primary health care: What is it? What will happen if you ignore nonemergency medical services (primary health care)? What is the role of guide to a primary care physician? What does a primary care physician do? Why are primary care physicians in high demand? What's a Primary Care Physician (PCP)? What are some benefits of being a primary care physician? When is it appropriate to seek assistance from your PCP? Is there a difference between a primary care physician and a primary care provider? What is the difference between a primary care physician and a primary care provider? What is a physician? What is an example of a primary care physician? What is the difference between a primary care physician training program and a primary care physician on duty at a location? What are categories of human healthcare in the state and outside the state? What are categories of medical emergencies? What are the categories of nonemergency medical services (primary health care)? What type of consultation is required for stable medical cases to be considered less serious than a medical emergency? How does a walk-in consultation with a physician work at community health centers in the state? What types of issues are handled at urgent care walk-in community health centers in the state? What is a Primary Care Physician? What is a Primary Care Doctor? Which doctors qualify as Primary Care Physicians? What is primary health care? Can so many residents be screened for so many medical conditions in one day by a few medical doctors? How many residents should be assigned to a medical doctor for primary health care? What should a health care resource be able to provide in primary health care? Should primary health care or hospitals organize health care discussions in communities? What are advantages of organizing health care discussions? What equipment and resources should ideally be in a primary health center? What equipment and resources should ideally be in a hospital emergency facility? Who nominates or recommends health care resources for the residents in the building and this area? Who has duty to provide and supervise such health care services in this area from the state department of health? Questions patient should answer What happens during a primary health care annual visit? What is an example of a primary care physician? What is the difference between a primary care physician training program and a primary care physician on duty at a location? What should a primary care physician know? |
|
Primary health care: What is it? Nonemergency medical services. There are some other definitions of primary healthcare you should be aware of. What will happen if you ignore nonemergency medical services (primary health care)? This can become medical emergency. If you completely ignore nonemergency medical services (primary health care), there can be many medical emergencies. What is the role of guide to a primary care physician? Guide from a distance. Supervise from a distance. What does a primary care physician do? 1. Primary care physicians (PCPs) are typically the first medical practitioners contacted by a patient. Where should you go if you develop a cough, if you’re feeling anxious and depressed, or if you are curious about a certain vaccine? The answer: your primary care doctor! Your primary care doctor focuses on holistic health care, meaning he or she is trained in treating a little bit of everything and coordinates patient health care in one central location. With a primary care doctor, you only need to make one appointment to discuss a variety of health issues you might be experiencing, whether they are physical, emotional or mental. 2. Better Manage Chronic Diseases Chronic health conditions like diabetes, arthritis and lupus are often difficult to monitor by yourself. A primary care doctor can help you stay organized and aware of how your chronic disease is affecting your body. Scheduling regular visits and performing routine tests are two ways your doctor can help you better maintain your chronic disease. 3. Higher Level of Comfort Most people don’t love talking to strangers, especially about their health care needs and concerns. Choosing a primary care doctor you trust is the first step. The next step is scheduling regular appointments with your doctor so that you can discuss your concerns and overall health. In addition, researchers at the Journal of Health Affairs found that patients with primary care doctors reported higher levels of satisfaction than patients without primary care doctors. The more you visit a doctor you trust, the better your relationship with him or her and the better your care. 4. Transparency of Entire Health History Routine visits with your primary care provider not only help with your comfort level, but they also build on your health history. Knowledge of your health history, as well as your family health history, is imperative for prevention of diseases and also helps your doctor catch early symptoms of serious conditions. 5. Lower Overall Health Costs Attending regular appointments with your primary doctor might seem tedious and like a waste of money at times, but research from the Journal of Health Affairs suggests that routine appointments with a primary care doctor cut overall health costs for patients. Regular screenings, open communication between you and your doctor, and a record of your health history all contribute to an overall lower cost of health care. 6. Routine Screenings Taking your blood pressure at every appointment might seem like a task, but screenings like these hold great importance when it comes to your health. Undergoing testing on a regular basis helps catch symptoms before they get worse or lead to debilitating health issues. 7. Catch Health Issues Early While routine screenings may find certain symptoms of health issues before they become larger problems, your primary care doctor also knows you well enough to ask the right questions and detect other health issues in their early stages. 8. Referrals to Other Medical Specialists Do you need a referral to see an ENT or a cardiologist? Start with an appointment with your primary care doctor. Chances are your doctor has helpful recommendations for specialists since he or she is familiar with how you prefer to participate in your health care. 9. Decrease in Hospital and ER Visits Research shows that patients who regularly visit their primary care physicians have fewer hospitalizations and emergency visits than those who do not utilize primary care doctors. Waiting too long to see a doctor or ignoring symptoms can lead to a hospitalization or an ER visit, two of the most expensive and overwhelming outcomes for patients. 10. Better Patient-provider Communication Communication is a two-way street, especially when it comes to your health. Communicating your health wants, needs and concerns are crucial for your doctor to address your health appropriately. Likewise, your primary care doctor should also feel comfortable holding honest conversations with you regarding their concerns and thoughts regarding your health. Why are primary care physicians in high demand? If you’re weighing your options for medical specialties, you’d be wise to include primary care at the top of your list — especially if employability is important to you. What's a Primary Care Physician (PCP)? A primary care physician is a physician who provides both the first contact for a person with an undiagnosed health concern as well as continuing care of varied medical conditions, not limited by cause, organ system, or diagnosis. What are some benefits of being a primary care physician? Studies show that having a primary care physician can help keep you healthy. When is it appropriate to seek assistance from your PCP? There are times when you should see your PCP and times when you should refer to other resources such as your state’s local Emergency Department or Urgent Care Center. DO see your PCP for: Non-Emergency needs Follow-ups Physicals Screenings Common illnesses (cold) Immunizations DO NOT see your PCP for: Emergencies/life or death situations (heart attack, stroke, severe allergic reactions); go to the emergency department for immediate care. If you feel your health issue can’t wait; go to urgent care Is there a difference between a primary care physician and a primary care provider? Yes. What is the difference between a primary care physician and a primary care provider? A primary care physician is a medical doctor who can provide a correct diagnosis and treatment of nonemergency healthcare problems. A primary care provider can be a doctor, but could be a physician’s assistant or a nurse practitioner. What is a physician? An individual who can diagnose and manage complex human medical problems in various healthcare setting. In America, all medical practitioners are physicians. In Australia and New Zealand, only specialists are referred to as physicians. This needs to be standardized. Physician belongs to activity sectors or academic discipline of medicine, human healthcare. What is an example of a primary care physician? On September 10, 2015, Doctor Munawara Sultana worked as a primary care physician at Uptown Community Health Center, 4867 N. Broadway Ave., Chicago, Illinois 60640-3603. This is an example of a primary care physician. What is the difference between a primary care physician training program and a primary care physician on duty at a location? Establishing a training program for primary care physicians and working at a specific location 9-5 as a primary care physician are two different services. What are categories of human healthcare in the state and outside the state?
What are categories of medical emergencies? 1.Critical medical emergencies. 2.Medical emergencies that are not critical but are medical emergencies. Take a look at this. Assessment in medical emergency situation. http://www.qureshiuniversity.com/emergencymedicalservices.html What are the categories of nonemergency medical services (primary health care)? Consultation required within 1 week. Consultation can be sought after a week within 3 months. Walk-in urgent care service at community health centers in the state. Walk- in nonurgent care service at community health centers in the state. Take a look at this. Assessment in medical nonemergency situation. What type of consultation is required for stable medical cases to be considered less serious than a medical emergency? Walk-in consultation with a physician at community health centers in the state. In some regions, this is known as urgent care walk-in community health center service in the state. Walk-in nonurgent care service at community health centers in the state is also possible if the caseload for the physician on duty at a community health center in the state allows it. How does a walk-in consultation with a physician work at community health centers in the state? A resident or patient walks into the community health center and approaches the receptionist or desk clerk and asks if specific physician consultation or any physician at community health center is available. The receptionist or desk clerk takes date of birth, name, mailing address, reason for consultation and records on computer. A specific physician or available physician gets a message that the patient has come in on a walk-in basis with the profile of the patient. The resident or patient has to wait until the physician completes consultations with other residents or patients who already had appointments. Walk-in waiting time at community health center can range from a few minutes to sometimes two or three hours. Every specific geographical location in the state or outside the state serves specific residents of the state. What types of issues are handled at urgent care walk-in community health centers in the state? Treating minor medical problems or injuries that require a health care provider's attention but are not life-threatening, such as: allergies, burns, colds, coughs, cuts, earaches, fevers, flu, fractures, infections, sore throats and sprains. In these situations, all vital signs are normal except there may be fever. There are no open fractures or loss of alignment of fractures. Burns are superficial only in epidermis of skin less than 1 percent without damage to any organ of human body. If cases are life threading, consultation at a medical emergency room by an emergency medical specialist is required. Which doctors qualify as Primary Care Physicians? There are 24 specialties in medicine but typically only three qualify as PCPs. Although some women may think their Obstetrician/Gynecologist qualifies as a PCP, in most cases only doctors with the following three specialties are considered PCPs: •Family Practice or General Practice: A family practitioner is qualified to care for the entire family. A family practitioner can be board-certified and have training in a variety of subjects including Obstetrics and Gynecology, Pediatrics, Internal Medicine and Psychiatry. This specialty was more common in years past but can still be found to treat the entire family. •Internal Medicine: An internist can diagnose and treat disease with medicine. An internist is not a surgeon. There are several sub-specialties an internist can have, including: specializing in a particular organ, like the lungs or the kidneys, a particular disease, like diabetes, or a particular age group, like the elderly. •Pediatrics: A pediatrician specializes in the overall well-being of children. Most pediatricians treat children from birth until adolescence or about 14 years old. Pediatricians can have sub-specialties such as surgery or pediatric cardiology. Primary Care In defining primary care, it is necessary to describe the nature of services provided to patients, as well as to identify who are the primary care providers. The domain of primary care includes the primary care physician, other physicians who include some primary care services in their practices, and some non-physician providers. However, central to the concept of primary care is the patient. Therefore, such definitions are incomplete without including a description of the primary care practice. The following five definitions relating to primary care should be taken together. They describe the care provided to the patient, the system of providing such care, the types of physicians whose role in the system is to provide primary care, and the role of other physicians, and non-physicians, in providing such care. Taken together they form a framework within which patients will have access to efficient and effective primary care services of the highest quality. Definition #1 - Primary Care Primary care is that care provided by physicians specifically trained for and skilled in comprehensive first contact and continuing care for persons with any undiagnosed sign, symptom, or health concern (the "undifferentiated" patient) not limited by problem origin (biological, behavioral, or social), organ system, or diagnosis. Primary care includes health promotion, disease prevention, health maintenance, counseling, patient education, diagnosis and treatment of acute and chronic illnesses in a variety of health care settings (e.g., office, inpatient, critical care, long-term care, home care, day care, etc.). Primary care is performed and managed by a personal physician often collaborating with other health professionals, and utilizing consultation or referral as appropriate. Primary care provides patient advocacy in the health care system to accomplish cost-effective care by coordination of health care services. Primary care promotes effective communication with patients and encourages the role of the patient as a partner in health care. Definition #2 - Primary Care Practice A primary care practice serves as the patient's first point of entry into the health care system and as the continuing focal point for all needed health care services. Primary care practices provide patients with ready access to their own personal physician, or to an established back-up physician when the primary physician is not available. Primary care practices provide health promotion, disease prevention, health maintenance, counseling, patient education, diagnosis and treatment of acute and chronic illnesses in a variety of health care settings (e.g., office, inpatient, critical care, long-term care, home care, day care, etc.). Primary care practices are organized to meet the needs of patients with undifferentiated problems, with the vast majority of patient concerns and needs being cared for in the primary care practice itself. Primary care practices are generally located in the community of the patients, thereby facilitating access to health care while maintaining a wide variety of specialty and institutional consultative and referral relationships for specific care needs. The structure of the primary care practice may include a team of physicians and non-physician health professionals. Definition #3 - Primary Care Physician A primary care physician is a generalist physician who provides definitive care to the undifferentiated patient at the point of first contact and takes continuing responsibility for providing the patient's care. Such a physician must be specifically trained to provide primary care services. Primary care physicians devote the majority of their practice to providing primary care services to a defined population of patients. The style of primary care practice is such that the personal primary care physician serves as the entry point for substantially all of the patient's medical and health care needs - not limited by problem origin, organ system, or diagnosis. Primary care physicians are advocates for the patient in coordinating the use of the entire health care system to benefit the patient. Definition #4 - Non-Primary Care Physicians Providing Primary Care Services Physicians who are not trained in the primary care specialties of family medicine, general internal medicine, or general pediatrics may sometimes provide patient care services that are usually delivered by primary care physicians. These physicians may focus on specific patient care needs related to prevention, health maintenance, acute care, chronic care or rehabilitation. These physicians, however, do not offer these services within the context of comprehensive, first contact and continuing care. The contributions of physicians who deliver some services usually found within the scope of primary care practice may be important to specific patient needs. However, the absence of a full scope of training in primary care requires that these individuals work in close consultation with fully-trained, primary care physicians. An effective system of primary care may utilize these physicians as members of the health care team with a primary care physician maintaining responsibility for the function of the health care team and the comprehensive, ongoing health care of the patient. Definition #5 - Non-Physician Primary Care Providers There are providers of health care other than physicians who render some primary care services. Such providers may include nurse practitioners, physician assistants and some other health care providers. These providers of primary care may meet the needs of specific patients. They should provide these services in collaborative teams in which the ultimate responsibility for the patient resides with the primary care physician. Primary care physician A primary care physician, or PCP, is a physician who provides both the first contact for a person with an undiagnosed health concern as well as continuing care of varied medical conditions, not limited by cause, organ system, or diagnosis. All physicians first complete medical school (MD, MBBS, or DO). To become primary care physicians, medical school graduates then undertake postgraduate training in primary care programs, such as family medicine (also called family practice or general practice in some ______), pediatrics or internal medicine. Some HMOs consider gynecologists as PCPs for the care of women, and have allowed certain subspecialists to assume PCP responsibilities for selected patient types, such as allergists caring for people with asthma and nephrologists acting as PCPs for patients on kidney dialysis. Emergency physicians are sometimes counted as primary care physicians. Emergency physicians see many primary care cases, but in contrast to family physicians, pediatricians and internists, are trained and organized to focus on episodic care, acute intervention, stabilization, and discharge or transfer or referral to definitive care, with less of a focus on chronic conditions and limited provision for continuing care. What is a Primary Care Physician? What is a Primary Care Doctor? A primary care physician is a specialist in Family Medicine, Internal Medicine or Pediatrics who provides definitive care to the undifferentiated patient at the point of first contact, and takes continuing responsibility for providing the patient's comprehensive care. Trained in every major area of medicine, primary care doctors serve as the primary source of your health care throughout life. Family Medicine Family medicine doctors provide continuing comprehensive primary care to your whole family. They see patients of all ages. Internal Medicine Internal medicine doctors, internists, specialize in the study, diagnosis and treatment of non-surgical diseases in adult patients. An internist is trained to diagnose and treat complex illnesses, as well as manage the prevention of illness. Some internists, geriatricians, specialize in the health-care needs of the elderly. Internal Medicine/Pediatrics (IM/Peds) Doctors who specialize in internal medicine and pediatrics have completed a combined residency program in internal medicine and pediatrics. They are able to provide preventive care as well as care for the complex medical problems of adults and children. Obstetrics and Gynecology General obstetricians and gynecologists specialize in providing health care to women. Obstetricians care for the woman before, during and after a pregnancy, while gynecologists deal with disorders and diseases of the female reproductive tract. Pediatrics Pediatricians specialize in the treatment of newborns, infants, children and adolescents. It is their role to plan and carry out a medical care program for children – from birth through adolescence. They provide preventive health care as well as care for acute and chronic illness. What is primary health care? A health care resource advertises capabilities of screening hypertension and diabetes. That is not primary health care. That is quackery. Such activities are planned on April 20, 2012, at Near North Center, Chicago, Illinois. Heartland Alliance Chicago, Illinois, also is involved in similar quackery. Asian Human Services has declared an annual health fair on April 25, 2012, in Chicago, Illinois, to screen specific medical conditions. Can so many residents be screened for so many medical conditions in one day by a few medical doctors? No, they cannot. How many residents should be assigned to a medical doctor for primary health care? One hundred patients per medical doctor. What should a health care resource be able to provide in primary health care? Annual health care assessment with screening of all medical conditions. Answer all relevant questions via e-mail, fax, postal mail, and face-to- face. Advise follow-up as per requirement. Advice counseling under the supervision of a medical doctor. Vision, hearing impairment, disability screening, blood cholesterol, blood glucose, blood pressure, bone density, body mass index, dental health, addiction screening, stress screening. Health care services for individuals in all stages of life. Maintain medical records of the residents. Update state department of health regularly. Assign 100 patients per medical doctor. Establish or connect to nearby biochemistry laboratory in case lab services are required (blood chemistry). Patient education. Research/investigate in case of any medical emergency and measures to prevent such medical emergencies. Update local medical emergency to place competent medical doctors with ability to reach correct diagnosis and treatment and answer all relevant questions. Every individual needs annual health care assessment. Should primary health care or hospitals organize health care discussions in communities? Yes, they should. What are advantages of organizing health care discussions? Discussion relevant to stress decreases stress. Patient education. What should a medical emergency or primary health care provider answer in case of medical emergency? Did the primary health care provider do a proper annual health care assessment? Did the primary health care provider miss anything in the annual health care assessment? Did the primary health care provider offer proper preventive health care advice? Most of the time, there are wrong referrals to medical emergency. Most of the time, any genuine medical emergency is due to improper primary health care. Existing resident services can be educated to be medical doctors and provide primary health care. What equipment and resources should ideally be in a primary health center? 1. Height measuring scale. 2. Weighing scale. 3. Snells chart for vision screening. 4. Blood biochemistry analyzer. 5. Computer with Internet connection. 6. Human thermometer. 7. Blood pressure equipment. 8. Competent medical doctors and staff. What equipment and resources should ideally be in a hospital emergency facility? 1. All equipment required in primary health center plus equipment elaborated below. 2. Crash cart. 3. Hospital emergency bed. 4. Electronic monitor 5. Competent medical doctors and staff. Who nominates or recommends health care resources for the residents in the building and this area? Who has duty to provide and supervise such health care services in this area from the state department of health? Those in primary health care should know you are in public service. You should know about state economy and state budget. Questions you need to answer How many medical doctors are expected to attend? Are they ready to answer relevant questions? Is there going to be any discussion? What is the time and duration of discussion? Are medical doctors who are likely to see the residents able to answer relevant questions? Where will residents go in case follow-up is required? How will state department of health be updated? Questions patient should answer Do you have a primary health care provider? Who is your primary health care provider? When did you last see a medical doctor? When did you last see your primary health care provider? How long has he or she been your primary health care provider? When did you first see him or her as primary health care provider? What happens during a primary health care annual visit? You present your identity card to the receptionist, who asks you a few questions. The receptionist will ask you to fill out a form with a few questions if required. You will be seated. A nurse will come and take you to the lab, where a technician will take blood samples for blood chemistry. You will be taken to another room to test your vital signs. A nurse will measure your height and weight for body mass index. You will be taken to the medical doctor’s office for diagnosis and treatment. If you get Internet health care, the routine is different. Here are further guidelines. |
Program Director: Doctor Asif Qureshi
Enhancing services of primary care physicians
|
What is the best method to enhance the quality of services of the primary care physician? Ask the patient to put all problems, issues, complaints, and/or conditions in writing. Verify the findings. Scan the document. Place the document in the patient’s medical records chart. Experience in America has shown that the patient says one thing and the primary care physician writes something else. The primary care physician has to do lots of research on his or her own to fix the issues. Seek help from others to fix the issues. Fix the underlying cause. Complaint about primary healthcare provider. On or before May 21, 2019, the entity mentioned below was found to be a substandard healthcare provider. The facility did not do anything to improve its healthcare services on or before May 21, 2019. Near North Health Service Corporation 1276 N. Clybourn Ave. Chicago, IL 60610 Phone: 312-337-1073 Fax: 312-337-7616 Website: https://www.nearnorthhealth.org/locations There primary care physicians were not competent either on or before May 21, 2019. Swedish Covenant Hospital Primary Care Physicians https://swedishcovenant.org/find-a-doctor Northwestern University https://www.feinberg.northwestern.edu/centers/index.html What describes the problems, issues, and/or complaints relevant to the quality of human healthcare? The patient complained of the substandard quality of primary care physicians in America on or before May 21, 2019. The primary care physician is not able to give a brief introduction of herself so that the patient has confidence in the primary care physician’s competence. The primary care physician cannot understand the problems, issues, and/or complaints. The primary care physician does not know the normal values of human biochemistry with proof presented from the FDA. The primary care physician has substandard knowledge and, thus, is pushing for non-required referrals. The primary care physician is only after a salary, with an utter disregard for the quality of human healthcare. The primary care physician is not able to answer questions via an online portal, even after a reminder, proving the incompetency of the primary care physician. The primary care physician is not able to answer relevant questions in person (face to face) or through the Internet relevant to the profession and/or services. This is not in ICD 10. Who has the answer? Who is willing to answer? Who has the duty and responsibility to answer? How do you plan to resolve these issues? What advice is there for existing in training and aspiring primary care physicians from Doctor Asif Qureshi? No primary care physicians should depend on ICD 10 coding for evaluation and treatment due to the fact that ICD 10 was still evolving as of May 2019. Every year there is some kind of revision. There are some serious medical issues that have not been included in ICD 10 as of May 22, 2019. Most important governments, like the government of Illinois and the government of California, have not nominated specific physicians to supervise progress on ICD 10 as of May 22, 2019. Primary care physicians must follow normal human biochemistry reference values. Take a look at this. https://qureshiuniversity.com/faculty.html#Debate Required |
Grants, funding, and remuneration for these resources.
| Who is responsible for providing grants, funding, and remuneration for these resources? |
Assessment of patients in a non-emergency situation by a primary care physician.
|
Here are guidelines from Doctor Asif Qureshi for existing, in training, and aspiring primary care physicians. Start with these questions. Why are you seeking a consultation with a primary care physician at this point? A first-time consultation for this patient requires detailed profiling. Where is the profile of the patient? What is the profile of the patient? What should a patient profile look like? https://qureshiuniversity.com/patients.html What describes the issue or issues? Take a look at this.
What describes the problems, issues, complaints, and/or conditions of the patient at this point among ICD 10? What describes the symptoms, signs, issues, problems, and/or complaints among the list of issues? Code Search What describes the diagnoses or issues among the list of diagnoses and issues? Code Search There are some serious medical issues that have not been included in ICD 10 as of May 22, 2019. Most important governments, like the government of Illinois and the government of California, have not nominated specific physicians to supervise progress on ICD 10 as of May 22, 2019. What describes all problems, issues, complaints, and/or conditions of the patient at this point? What is the diagnosis at this point? What is the treatment at this point? |
Providing Clinical Summaries to Patients after Each Office Visit
|
Who should provide this document to the patient whether within or outside the state? The primary care physician provides this document to the patient during every clinical visit to the office. One copy remains in the computer systems/office records and one copy is given to the patient. |
What should be included in the Patient Clinical Summary during each office visit to a primary care physician?
|
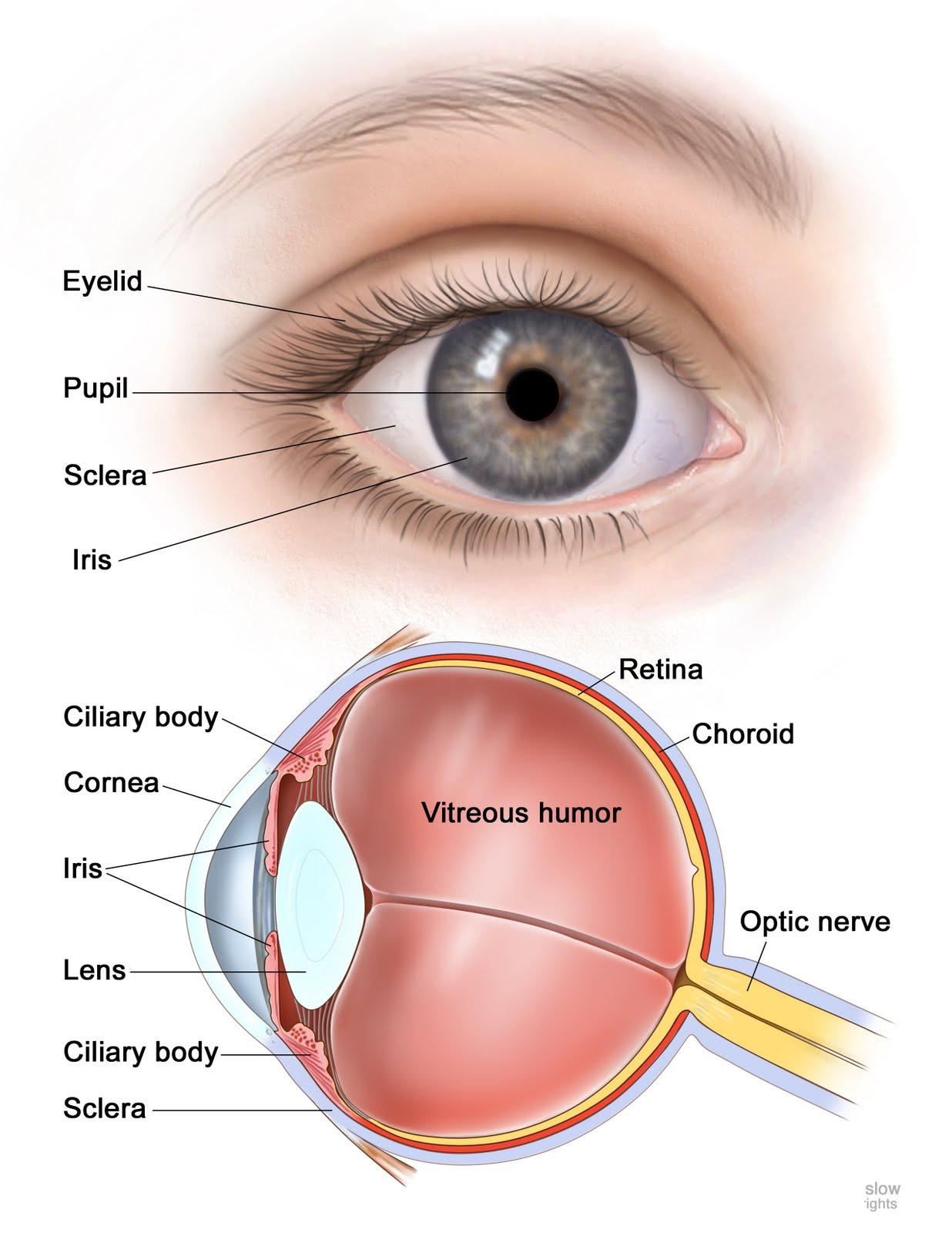
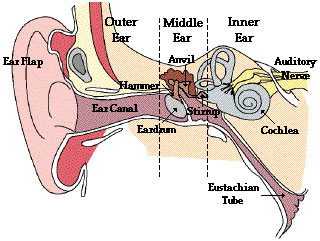
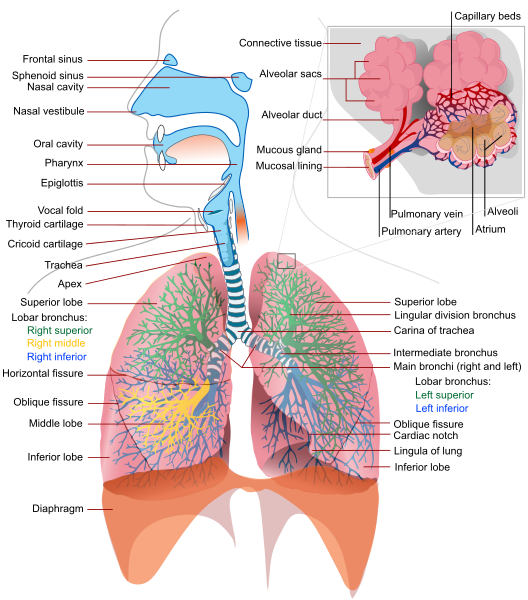
The purpose of the 11 organ systems is for the human body to maintain homeostasis. Organs and Functions What are the human organs and their function? Adrenal glands - Fight or flight emergency explosive action and mental clarity. Appendix - No longer in direct use, theorized to help Immune system. Bladder - Temporally collects liquids from food waste. Brain - A neural network of interdependent systems to send signals to muscles. Epidermis - protect against pathogens, oxidant stress (UV light) and chemicals. Esophagus - Muscular tube through which food travels to the stomach. Eyes - Conversion of photons into a data stream for the optic nerve. Gall bladder - Fat conversion/digestion with high powered chemicals. Heart - Pump to move blood around the body. Kidney - Regulate acidity, blood pressure, salt/water balance, signal hormones. Large intestine - Absorb water and last remaining nutrients from waste. Liver - Filter out the blood of impurities and toxins. Lungs - Absorption of Oxygen and release of Carbon Dioxide. Mouth - Temporary storage area for food while it is evaluated and crushed. Ovaries - In Females, secrete estrogen, progesterone and create ovums. Pancreas - Break down the carbohydrates, proteins, and lipids in food. Parathyroid - Control the amount of calcium in the blood and within the bones. Pleura - Lubricant and structure to convert muscle movements to inhale/exhale. Prostate gland - In Males, Assist in the preparation of semen. Rectum - About 12cm of temporary storage site for feces. Small intestine - Primary absorption of nutrients and minerals in food. Spine - Bendable support structure for upper body, protects wires from brain to lower body. Spleen - Secondary backup systems to regulate blood and immune system. Stomach - Dissolve and churn eaten foods with acids. Testes - In Males, create sperm containing the DNA code to build another human. Thyroid gland - Configuration for energy storage, dial in sensitivity to hormones. Tongue - Evaluate and reposition food in the mouth and push down esophagus. Uterus - Hold and supply nutrients to the ovum while it grows into a human. |
| Human |
| Adrenal glands |
| Appendix |
| Bladder |
| Blood |
| Blood vessels |
| Bones |
| Brain |
| Bronchi |
| Bronchial tubes |
| Cartilage |
| Diaphragm |
| Ears |
| Epidermis |
| Esophagus |
| Eyes |
| Gall bladder |
| Gonads |
| Hair |
| Heart |
| Intestines |
| Joints |
| kidneys |
| Large intestine |
| Ligaments |
| Liver |
| Lungs |
| Lymph |
| Lymph nodes |
| Lymph vessels |
| Mammary glands |
| Mouth |
| Muscles |
| Nails |
| Nasal passages |
| Nerves |
| Nose |
| Ovaries |
| Pancreas |
| Parathyroid |
| Penis |
| Pharynx |
| Pineal gland |
| Pituitary gland |
| Pleura |
| Prostate gland |
| Rectum |
| Scrotum |
| Skin |
| Pituitary gland |
| Small intestine |
| Spinal cord |
| Spine |
| Spleen |
| Stomach |
| Sweat glands |
| Teeth |
| Tendons |
| Testes |
| Thymus |
| Thyroid gland |
| Tongue |
| Tonsils |
| Trachea |
| Ureters |
| Urethra |
| Urinary bladder |
| Uterus |
| Vagina |
| Vas deferens |
|
Here are further guidelines. Osteology Here are further guidelines. |
Brain & Nervous System
|
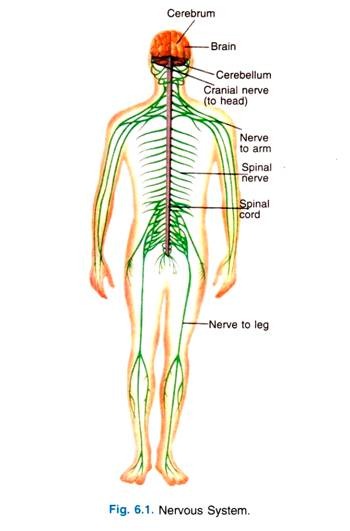
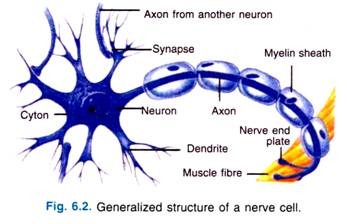
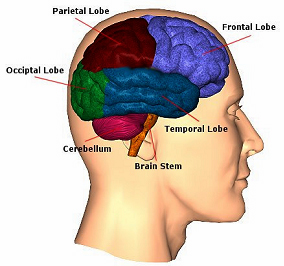
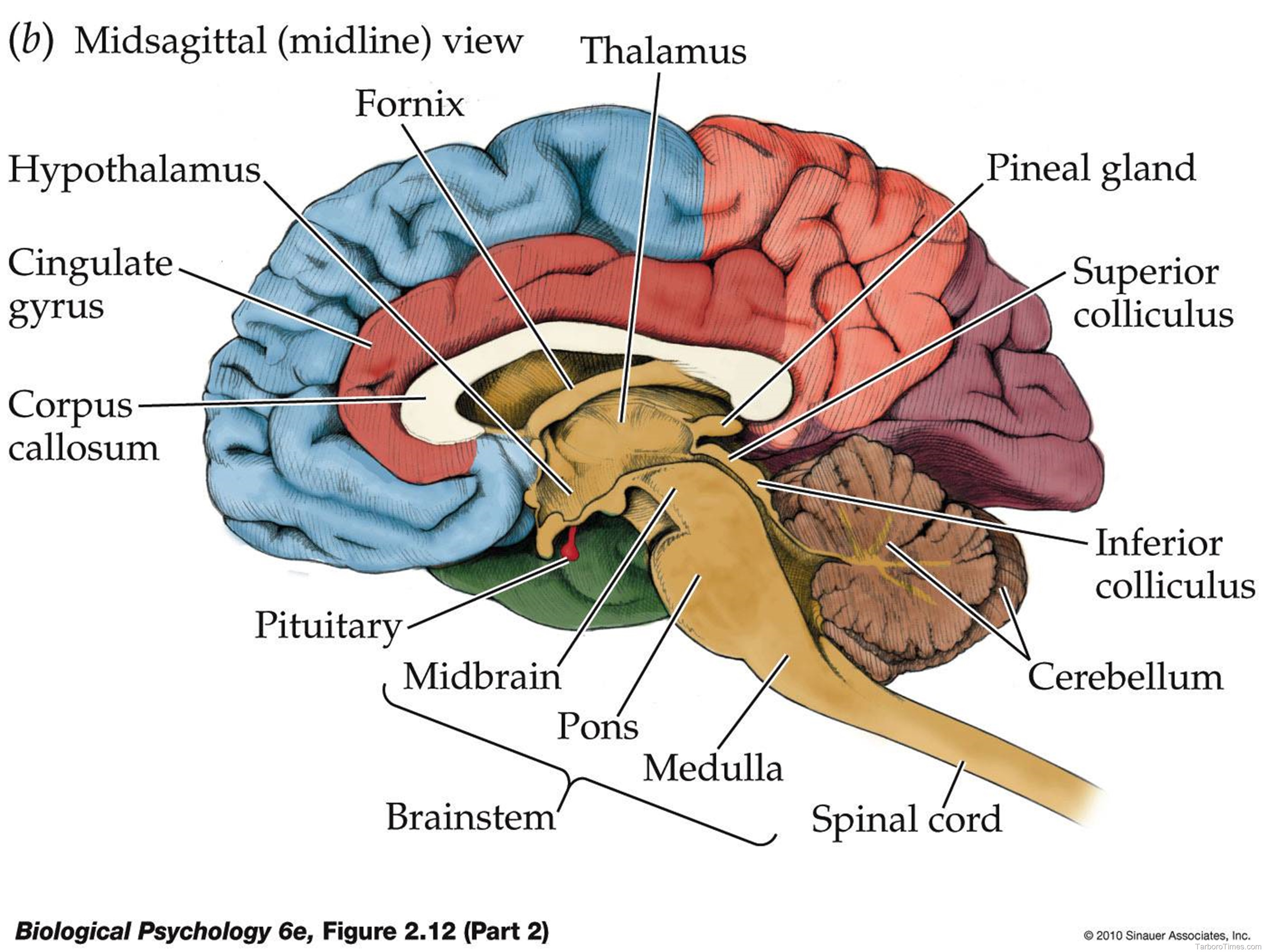
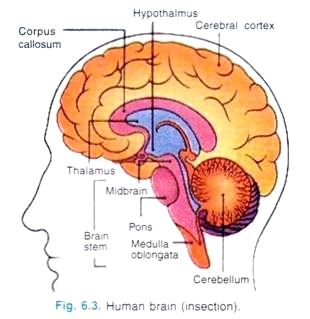
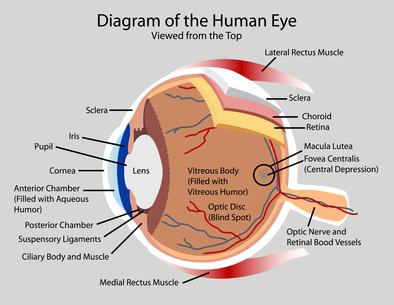
What is the nervous system? The nervous system is a complex, sophisticated system that regulates and coordinates body activities. It is made up of two major divisions, including the following: •Central nervous system. This consists of the brain and spinal cord. •Peripheral nervous system. This consists of all other neural elements. In addition to the brain and spinal cord, principal organs of the nervous system include the following: •Eyes •Ears •Sensory organs of taste •Sensory organs of smell •Sensory receptors located in the skin, joints, muscles, and other parts of the body What are some disorders of the nervous system? The nervous system is vulnerable to various disorders. It can be damaged by the following: •Trauma •Infections •Degeneration •Structural defects •Tumors •Blood flow disruption •Autoimmune disorders Disorders of the nervous system Disorders of the nervous system may involve the following: •Vascular disorders, such as stroke, transient ischemic attack (TIA), subarachnoid hemorrhage, subdural hemorrhage and hematoma, and extradural hemorrhage •Infections, such as meningitis, encephalitis, polio, and epidural abscess •Structural disorders, such as brain or spinal cord injury, Bell's palsy, cervical spondylosis, carpal tunnel syndrome, brain or spinal cord tumors, peripheral neuropathy, and Guillain-Barré syndrome •Functional disorders, such as headache, epilepsy, dizziness, and neuralgia •Degeneration, such as Parkinson's disease, multiple sclerosis, amyotrophic lateral sclerosis (ALS), Huntington's chorea, and Alzheimer's disease Any environmental change due to which any organism shows reaction is known as stimulus. The reaction shown by the organism is called response. The organism gets many stimuli from its environment, these are called external stimuli. The organism gets these stimuli from the other organisms or any other living things or heat, water, temperature, light and wind. Some stimuli come from the inside of the body of an organism, these are called internal stimuli. Nerve Impulse is an electrochemical change occurring in the membrane of a nerve fiber produced by a stimulus. What is Nervous System? The human body has quite a few systems. These systems work together but perform separate particular processes. All the systems are closely related to each other. So, it is necessary to keep co-ordination among all of them and among the organs of each system. This coordination is done by a system, called nervous system (Fig. 6.1), which is a network of various nerves. A nerve consists of a bundle of nerve fibre, a number of neurons make a nerve fibre, there are about 30,000 million nerves in human body. The speed of nerve impulse is 100 meters per second. Need of Nervous System: Nervous system is required in our body due to some factors: 1. Nervous system informs us about the outside world through the sense organs. 2. Nervous system helps us to think, to remember. 3. This system regulates involuntary activities like heart beat and breathing. 4. It controls and keep co-ordination among various system of the body. Structure of Neuron: A neuron is a structural and functional unit of nervous system. A neuron consists of the following parts (Fig. 6.2). (a) Cyton: The main part of neuron is a cell body, it is called cyton. Cyton contain nucleus and cytoplasm. (b) Dendrite: These are highly branched structures of cyton. Dendrite has specialized structured to receive message. (c) Axon: Axon is long specialized process aries from the cyton. It may be from few mm to up to more than one metre in length. Axon is surrounded by a sheath called myelin sheath. Places, where one neuron communicates with another are called synapses. There are three kinds of neurons. 1. Sensory neurons: These neurons carry impulses from the sense organs up to the brain. 2. Motor neurons: These are made up of motor nerve fibre and carry impulses from central nervous system to various organs. 3. Association neurons: These are located in the brain and spinal cord, which connect sensory and motor centres. There are three main divisions of the nervous system: 1. Central nervous system (CNS): Central nervous system includes the brain and the spinal cord. The Brain:
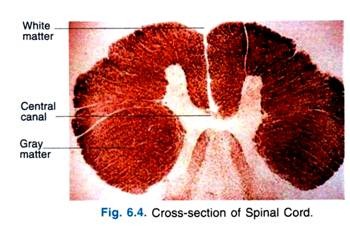
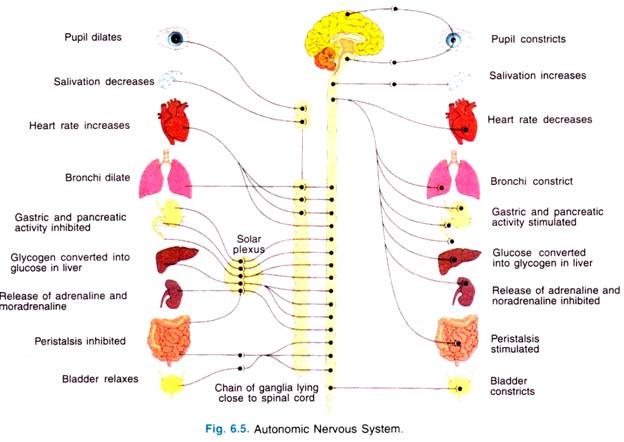
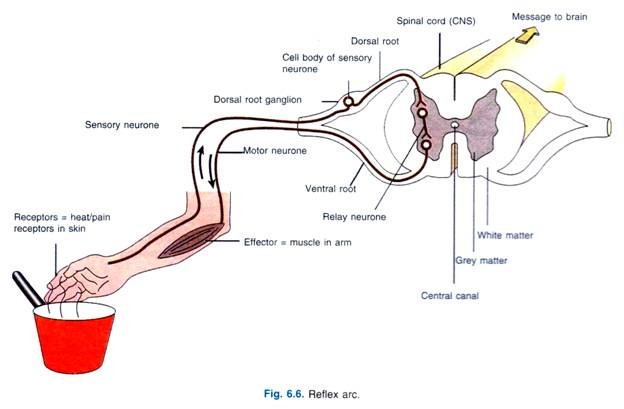
Brain is the most vital and delicate part of human body. It is enclosed inside the skull. Brain is protected by three membranous coverings called meninges. The dura mater is the outermost tough covering, arachnoid is the middle one contains blood vessels and the tender. Innermost layer is pia mater. The membranes contain a fluid between them is called cerebrospinal fluid. It nourishes the brain and absorb shocks. Brain has three main parts (Fig. 6.3). 1. The cerebrum 2. The cerebellum 3. Medulla oblongata. The Cerebrum: This is the largest part of the brain it is divided into right and left halves called cerebral hemisphere. This covers all the parts of the brain. The outer part of this is lightly convoluted with ridges and grooves, these increases the surface area of the brain. The two hemisphere are held together by a structure called corpus callosum. Surface of cerebrum is made up of grey matter and inner side is made up of white matter. It controls mental activities, like thinking and reasoning, it is seat of intelligence and centre for memory. It perceives the impulses such as pain, touch, smell, taste, hearing and light. The Cerebellum: This is smaller part of the brain, present just at the base and under the large cerebrum and above the medulla oblongata. It consists of two large lobes called cerebellar hemispheres. It has an inner core of white matter which is surrounded by grey matter. Its main function is to maintain body ‘balance’ and coordinate muscular activities. Medulla oblongata: This is triangular in shape and is the lowest part of the brain located at the base of the skull. It controls involuntary activities such as heart beat, respiratory system, coughing and sneezing. The Spinal Cord: The spinal cord (Fig. 6.4) is a long, un-segmented structure extends from the medulla oblongata. It runs down almost the whole length of the backbone to the end at the second lumbar vertebra. It is covered by three covering called meninges. Cerebrospinal fluid is filled between the meninges. Spinal cord is hollow from inside containing a cavity called central canal. Spinal cord is concerned with three functions, reflexes below the neck, carrying sensory impulses from the skin and muscles to the brain, conducting motor responses from the brain to the muscles of limbs and trunk. 2. Peripheral nervous system: (PNS): Includes the nerves that emerge from the brain and spinal cord. Cranial nerves emerge from the brain, there are twelve (12) pairs of cranial nerves. There are thirty one (31) pairs of spinal nerves emerge from the spinal cord. There are 8 pairs present in neck region, 12 pairs on the thorax region, 5 pairs in the lumbar region, 5 pairs are present in sacral and 1 pair in the coccygeal region. 3. Autonomic nervous system (ANS): The autonomic nervous system consists of a pair of chains of nerves and ganglia on either side of the back bone. It controls all the involuntary activities of various body viscera (means internal body organs, especially those in the abdomen) (Fig. 6.5). Reflex Action: Reflex action is involuntary, automatic action without the involvement of the brain. The path that an impulse takes in a reflex action is called a reflex arc (Fig. 6.6). All the reflexes taking place are of two types, unconditional reflexes and conditional reflexes. Pavlov is father of conditional reflexes. Closure of eyes on seeing very bright light, knee jerk, withdrawal of hand on touching fire, sneezing are the examples of unconditional reflexes.
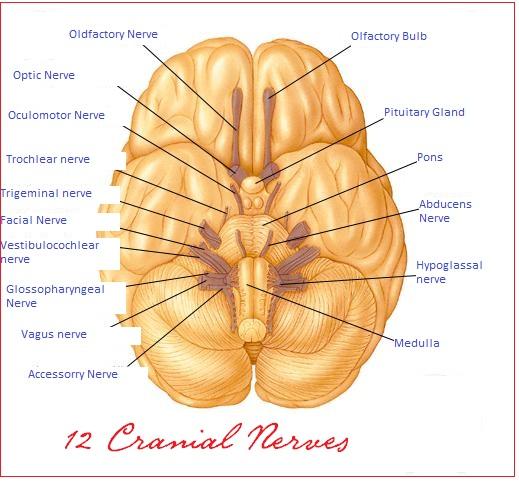
1. Olfactory This is a type of sensory nerve that contributes in the sense of smell in human being. These basically provide the specific cells that are termed as olfactory epithelium. It carries the information from nasal epithelium to the olfactory center in brain. 2. Optic nerve This again is a type of sensory nerve that transforms information about vision to the brain. To be specific this supplies information to the retina in the form of ganglion cells. 3. Oculomoter nerve This is a form of motor nerve that supplies to different centers along midbrain. Its functions include superiorly uplifting eyelid, superiorly rotating eyeball, construction of pupil on the exposure to light and operating several eye muscles. 4. Trochlear This motor nerve also supplies to the midbrain and performs the function of handling the eye muscles and turning the eye. 5. Trigeminal This is a type of largest cranial nerve in all and performs many sensory functions related to nose, eyes, tongue and teeth. It basically is further divided in three branches that are ophthalmic, maxillary and mandibular nerve. This is a type of mixed nerve that performs sensory and motor functions in brain. 6. Abducent This is again a type of motor nerve that supplies to the pons and perform function of turning eye laterally. 7. Facial This motor nerve is responsible for different types of facial expressions. This also performs some functions of sensory nerve by supplying information about touch on face and senses of tongue in mouth. It is basically present over brain stem. 8. Vestibulocochlear This motor nerve is basically functional in providing information related to balance of head and sense of sound or hearing. It carries vestibular as well as cochlear information to the brain and is placed near inner ear. 9. Glossopharyngeal This is a sensory nerve which carries sensory information from pharynx (initial portion of throat) and some portion of tongue and palate. The information sent is about temperature, pressure and other related facts. It also covers some portion of taste buds and salivary glands. The nerve also carries some motor functions such as helping in swallowing food. 10. Vagus This is also a type of mixed nerve that carries both motor and sensory functions. This basically deals with the area of pharynx, larynx, esophagus, trachea, bronchi, some portion of heart and palate. It works by constricting muscles of the above areas. In sensory part, it contributes in the tasting ability of the human being. 11. Spinal accessory nerve As the name intimates this motor nerve supplies information about spinal cord, trapezius and other surrounding muscles. It also provides muscle movement of the shoulders and surrounding neck. 12. Hypoglossal nerve This is a typical motor nerve that deals with the muscles of tongue. Cranial Nerves Spinal Nerves Nerves History Have you had a temporary loss of function? Yes Do you have a persistent nervous system problem, such as a tremor or lack of coordination? Yes Do you think your nervous system problem may be caused by a medicine? Yes Alzheimer's Disease Autism Bell’s Palsy Coma Concussion Creutzfeldt-Jakob Disease Deep Brain Stimulation Dementia Dizziness Encephalitis Epilepsy Essential Tremor Guillain-Barré Syndrome Hydrocephalus Lou Gehrig's Disease (ALS) Mad Cow Disease Meniere's Disease Multiple Sclerosis Myasthenia Gravis Nerve Pain Parkinson's Disease Peripheral Neuropathy Preventing Falls Reflex Sympathetic Dystrophy Syndrome Restless Legs Syndrome Seizure Disorders Speech and Language Disorders Stroke Tourette's Tremors Trigeminal Neuralgia Vertigo |
Circulation Symptoms
Circulatory System
|
Abnormal pulse Chest pain or pressure Cyanosis Difficulty breathing Sudden weakness or numbness on one side of the body Slurred speech Loss of vision Paralysis or inability to move a body part Poor wound healing Sudden, severe headache; or confusion or loss of consciousness, even for a brief moment What is circulatory system? On average, your body has about 5 liters of blood continually traveling through it by way of the circulatory system. The heart, the lungs, and the blood vessels work together to form the circle part of the circulatory system. The pumping of the heart forces the blood on its journey. How does the blood circulatory system work? The body's circulatory system really has three distinct parts: pulmonary circulation, coronary circulation, and systemic circulation. Or, the lungs (pulmonary), the heart (coronary), and the rest of the system (systemic). Each part must be working independently in order for them to all work together. Circulatory system: The system that moves blood throughout the body. The circulatory system is composed of the heart, arteries, capillaries, and veins. This remarkable system transports oxygenated blood from the lungs and heart throughout the body via the arteries. The blood goes through the capillaries which are situated between the arteries and veins. And the blood that has been depleted of oxygen by the body is then returned to the lungs and heart via the veins. What are the signs of circulation problems? Circulation symptoms occur when blood flow to a part of your body is reduced, usually as a result of a narrowing of the arteries, the blood vessels that carry blood rich in oxygen to all parts of the body. Typically this occurs due to the plaque buildup in the artery walls, a condition known as atherosclerosis. Risk factors for atherosclerosis include smoking, diabetes, obesity, and elevated blood lipid (fat) levels. It results in a narrowing of the arteries, and this narrowing prevents adequate blood flow. Circulation symptoms can also arise in the veins (blood vessels that carry blood back to the heart). Blood clots in the veins may cause local inflammation and swelling (thrombophlebitis), or the blood clots may break off and travel to other sites in the body, in a process known as embolization. Pulmonary embolism is a life-threatening condition caused by a blockage of an artery in the lung due to a blood clot that has traveled to this location. Circulation symptoms can occur in the head, arms, kidneys, stomach, and other organs. When blood flow to an organ is interrupted, especially over time, organ failure can result. Interruption of blood flow to the brain (stroke) or heart (heart attack) are serious causes of circulation symptoms. The legs are another common site for circulation symptoms. As the flow of blood is blocked or slowed significantly due to peripheral artery disease in the legs, you may feel pain, heaviness and numbness in your legs, especially during and after walking or climbing stairs, when your muscles need more blood and are not able to get enough. You may prevent or improve circulation symptoms by making important lifestyle changes, particularly by giving up smoking and limiting fats, cholesterol, and refined sugars in your diet, as well as asking your physician to recommend a good exercise program for you. The Circulatory System 1. What is circulation? Circulation is the movement of substances like nutrients and gases within blood vessels and cavities throughout the organism. 2. Do all animals have a circulatory system? Not all animals have a circulatory system. Poriferans, cnidarians, platyhelminthes and nematodes (in these there are the pseudocoelom fluid but no vessels) are avascular animals. Echinoderms do not have true circulatory systems either. 3. What is the alternative means for transport of substances in animals without a circulatory system? Why is blood important for larger animals? In animals that do not present the circulatory system the transport of substances occurs by cell to cell diffusion. The blood is a fundamental means of substance transport for larger animals since in these animals there are tissues distant from each other and from the environment thus making diffusion impossible. 4. What are the two types of circulatory systems? The circulatory systems can be classified into open circulatory system and closed circulatory system. 5. What is an open circulatory system? Open circulatory system is the one in which blood does not circulate only inside blood vessels but it also falls in cavities that irrigate tissues. In the open circulatory system the blood pressure is low and generally the blood (called hemolymph) has low cellularity. Arthropods, molluscs (the cephalopods are exception) and protochordates have open circulatory system. 6. What is a closed circulatory system? A closed circulatory system is one in which blood circulates only inside blood vessels. For this reason the blood pressure is higher in animals with closed circulatory system. The cellularity of the blood is also higher with many specific blood cells. The closed circulatory system is a feature of annelids, cephalopod molluscs and vertebrates. 7. What are the advantages of the closed circulatory system over the open circulatory system? The closed circulatory system is more efficient. Since blood circulates only inside blood vessels it can do it with more pressure reaching farther distances between the organs where hematosis happens and the peripheral tissues. In addition the circulatory speed also heightens making possible more oxygen supply to great consuming tissues, like the muscle tissues that then can perform faster movements. Animals with an open circulatory system (with the exception of insects that do gas exchange independently from the circulation) are generally slower and have a low metabolic rate. 8. What is the difference between octopuses and mussels regarding their circulatory systems? How does that difference influence the mobility of these animals? Cephalopod molluscs, like octopuses and squids, have a closed circulatory system with blood pumped under pressure flowing within vessels. Bivalve molluscs, like mussels and oysters, have an open circulatory system (also known as lacunar circulatory system) where blood flows under low pressure since it falls in cavities of the body and does not only circulate within blood vessels. Molluscs with closed circulatory systems are larger, agile and can actively move; molluscs with open circulatory systems are smaller, slow and some are practically sessile. 9. Why, even thoough they have an open circulatory system, can flying insects like flies beat their wings with great speed? In insects the circulatory system is open but this system does not participate in the gas exchange process and in oxygen supply to the tissues. Gases go in and out through the independent tracheal system that allows direct contact of cells with the ambient air. Therefore an insect can supply the great oxygen demand of its fast-beating wing muscles even having open circulatory system. 10. What are the typical components of a closed circulatory system? The typical components of the closed circulatory system are the blood vessels within which blood circulates (arteries, veins and capillaries), a pumping organ (heart) and the blood or bloodlike fluid. 11. How does the heart impel the blood? The heart is a muscular organ that contains chambers (right atrium and right ventricle and left atrium and right ventricle) through which blood passes. The blood enters the heart in the atria, goes to the ventricles and then leaves the organ. The blood is pumped out of the heart by the contraction of the muscle fibers that form the ventricular walls. The contraction reduces the ventricle volume thus increasing the internal pressure and the blood then flows to the exit vessels (pulmonary artery for the right ventricle and aorta for the left ventricle). When ventricular muscle fibers distend the ventricles regain their original size and receive new blood flow coming from the atria. 12. What is the difference between systole and diastole Systole and diastole are the two stages into which the cardiac cycle is divided. Systole is the stage when the contraction of ventricular muscle fibers occurs and the ventricles are emptied. Diastole is the stage of the cardiac cycle when the ventricular muscle fibers distend and the ventricles are filled with blood. 13. What are arterial vessels, arteries and arterioles? Arterial vessels are every blood vessel that carries blood from the heart to the tissues. Arteries and arterioles are arterial vessels. Arterioles are thin arteries that end in capillaries. Not all arteries however contain arterial blood (highly oxygenated blood). The pulmonary artery and its ramifications, arteries that carry blood from the right heart ventricle to the lungs, contain venous blood. 14. What are venous vessels, veins and venules? Venous vessels are every blood vessel that carries blood from the tissues to the heart. Veins and venules are venous vessels. Venules are thin veins that are continuous to capillaries. In general venous vessels carry venous blood. The pulmonary veins that carry blood from the lungs to the left atrium of the heart however contain arterial blood. 15. What are the capillaries of the vascular system? Capillaries are small blood vessels that perform exchange of substances between the blood and the body tissues. Capillaries are neither arteries nor are they veins since they have distinct features. In capillaries the wall is made of a single layer of endothelial cells through which substances are exchanged. These vessels receive blood from the arterioles and drain to the venules. 16. What is the part of the vascular system that performs exchange of gases and other substances with the tissues? Only capillaries perform exchange of gases and other substances with the tissues. 17. Are the arteries or the veins constituted of more muscle tissue? How different are the walls of these two types of blood vessels? The arterial system has thicker muscle walls since within arteries the blood circulates under higher pressure. The veins are more flaccid than arteries. From the lumen to the external layer both types of vessels are made of endothelium, muscle tissue and connective tissue. In both the endothelium is a single layer of cells. In arteries the muscle tissue portion is thicker than in veins and in these vessels the external connective tissue is thicker than in arteries. Arteries are the pulsating blood vessels. The arterial pulse can be felt in a medical examination, for example, by the palpation of the radial artery in the internal and lateral face of the wrist near the base of the thumb. 18. What are the valves of the venous system? What is their function? The valves of the venous system are structures inside the veins that permit blood to flow only in the normal way (from the tissues to the heart) and forbid it to return in the reverse way in favor of gravity. The valves close when the pressure of the fluid column above (after, regarding normal flux) is higher than the fluid pressure before them. Valves are thus fundamental for the returning of blood to the heart. 19. How do the muscles of the legs and of the feet contribute to the venous return? The muscles of the legs, mainly the muscles of the calves, contract and compress the deep veins of the legs impelling the blood to the heart. The plantar portion of the feet retains blood and when it is compressed against the ground it impels its blood volume and aids venous return. 20. What are varices? Why are they more common in the inferior limbs? Varix means abnormal enlargement of veins. Varices occur when excessive pressure against the normal blood flux creates enlargement of the vein and thus insufficient functioning of its valves (venous insufficiency). Varices are more common in the veins of the inferior limbs since the fluid column above these vessels is higher. This is the reason why people that spend much time standing (e.g., surgeons) are more susceptible to varices. In general varices are not the apparent superficial veins that appear in the leg of varix patients. These apparent vessels are the consequences of internal varices (venous insufficiency) in the deep internal veins of the legs and they appear because the blood flux is diverted to superficial veins. (Popularly however apparent superficial veins are called varices.) 21. What is the lymphatic system? The lymphatic system is a network of specialized valved vessels that drain interstitial fluid (lymph). The lymphatic system is also responsible for the transport of chylomicrons (vesicles that contain lipids) made after the absorption of fats by the intestinal epithelium. In the way of the lymphatic vessels there are ganglial-like structures called lymph nodes that contain many cells of the immune system. These cells filter impurities and destroy microorganisms and cellular wastes. The lymphatic vessels drain to two major lymphatic vessels, the thoracic duct and the right lymphatic duct, that in their turns drain into tributary veins of the superior vena cava. 22. Why in inflammatory and infectious conditions may clinical signs related to the lymphatic system occur? The lymph nodes, or lymph glands, have lymphoid tissue that produces lymphocytes (a type of leukocyte). In inflammatory and infectious conditions the enlargement of lymph nodes of the lymphatic circuits that drain the affected region due to the reactive proliferation of leukocytes is common. This enlargement is known as lymphadenomegaly and sometimes it is accompanied by pain. The search for enlarged or painful lymph nodes is part of the medical examination since these findings may suggest inflammation, infection or other diseases. 23. Which are the heart chambers respectively where the entrance and the exit of blood occur? The heart chambers through which blood enters the heart are the atria. There are the right atrium and the left atrium. The heart chambers through which the blood exits the heart are the ventricles. There are the right ventricle and the left ventricle. 24. Concerning the thickness of their walls how different are the heart chambers? The ventricle walls are thicker than the atrium walls since ventricles are structures responsible for the pumping of the blood to the lungs or tissues. The muscular work of the ventricles is harder and their muscle fibers develop more. The left ventricle is more muscular than the right ventricle because pumping blood to the lungs (the right ventricle task) is easier (needs less pressure) than pumping blood to the other tissues of the body (the left ventricle task). 25. What is vena cava? Which type of blood circulates within the vena cava? The vena cava are either of two large veins that debouch into the right atrium. The superior vena cava drains all blood that comes from the head, the superior limbs, the neck and the superior portion of the trunk. The inferior vena cava carries blood drained from the inferior portion of the trunk and the inferior limbs. Venous blood circulates within the vena cava. 26. Which is the first (human) heart chamber into which blood enters? Where does the blood go after passing that chamber? What is the name of the valve that separates the compartments? Why is that valve necessary? The venous blood that comes from the tissues arrives in the right atrium of the heart. From the right atrium the blood goes to the right ventricle. The valve that separates the right ventricle from the right atrium is the tricuspid valve (a valvular system made of three leaflets). The tricuspid valve is necessary to prevent returning of blood to the right atrium during systole (contraction of ventricles). 27. What is the function of the right ventricle? To where does the right ventricle pump the venous blood? The function of the right ventricle is to get venous blood from the right atrium and pump the blood to be oxygenated in the lungs. The venous blood is carried from the right ventricle to the lungs by the pulmonary artery and their ramifications. 28. What is the valve that separates the right ventricle from the pulmonary artery? Why is that valve important? The valve that separates the right ventricle and the base of the pulmonary artery is the pulmonary valve. The pulmonary valve is important to prevent blood from the pulmonary circulation to flow back to the heart during diastole. 29. Do the arteries that carry blood from the heart to the lungs contain arterial or venous blood? What happens to the blood when it passes through the lungs? Arteries of the pulmonary circulation are arteries that carry venous blood and not arterial blood. When the blood passes within the alveolar capillaries of the lungs hematosis (oxygenation) occurs and carbon dioxide is released to the exterior. 30. What and how many are the pulmonary veins? The pulmonary veins are part of the pulmonary circulation. They are vessels that carry oxygen-rich (arterial) blood from the lungs to the heart. There are four pulmonary veins, two that drain blood from the right lung and other two that drain the left lung. The pulmonary veins debouch into the left atrium bringing arterial blood to the heart. Although they are veins they carry arterial blood and not venous blood. 31. To which heart chamber does the blood go after leaving the left atrium? What is the valve that separates these compartments? The arterial blood that has come from the lungs to the left atrium passes then to the left ventricle. The valve between the left ventricle and the left atrium is the mitral valve, a bicuspid (two leaflets) valve. The mitral valve is important because it prevents the regurgitation of blood to the left atrium during systole (contraction of the ventricles). 32. What is the function of the left ventricle? Where does the blood go after leaving the left ventricle? The function of the left ventricle is to get blood from the left atrium and to pump the blood under high pressure to the systemic circulation. After leaving the left ventricle the blood enters the aorta, the largest artery of the body. 33. What is the valve that separates the aorta from the heart? What is the importance of that valve? The valve between the left ventricle and the aorta is the aortic valve. The aortic valve prevents the retrograde flux of blood to the left ventricle during diastole. Besides, as the aortic valve closes during diastole, part of the retrograde blood flux is impelled through the coronary ostia (openings), orifices located in the aorta wall just after the valvular insertion and contiguous to the coronary circulation responsible for the blood supply of the cardiac tissues. 34. Is the ventricle lumen larger during systole or during diastole? Systole is the stage of the cardiac cycle on which the ventricles contract. So the lumen of these chambers is reduced and the pressure upon the blood within them is heightened. During diastole the opposite occurs. The muscle fibers of the ventricles relax and the lumen of these chambers enlarges helping the entrance of blood. 35. What is the stage of the cardiac cycle during which the ventricles are filled? The filling of the ventricles with blood occurs during diastole. 36. Of which type of tissue is the heart made? How is this tissue oxygenated and nutrified? The heart is made of striated cardiac muscle tissue. The heart muscle is called the myocardium and it is oxygenated and nutrified by the coronary arteries. The coronary arteries come from the base of the aorta and ramify around the heart penetrating the myocardium. Diseases of the coronary arteries are severe conditions. 37. Which are the two main metabolic gases transported by the blood? The main metabolic gases transported by the blood are molecular oxygen (O2) and carbon dioxide (CO2). 38. How do respiratory pigments act? Respiratory pigments are oxygen-carrying molecules present in the blood. When the oxygen concentration is high, for example, in the pulmonary alveoli, the respiratory pigments bind to the gas. In conditions of low oxygen concentration, e.g., in tissues, the respiratory pigments release the molecule. In the human blood the respiratory pigment is hemoglobin, present within the red blood cells. 39. How different are oxyhemoglobin and hemoglobin? Where is it expected to find a higher concentration of oxyhemoglobin, in peripheral tissues or in the lungs? Oxygen-bound hemoglobin is called oxyhemoglobin. In the lungs the oxygen concentration is higher and so there is a higher oxyhemoglobin concentration. In the peripheral tissues the situation is the reverse, the concentration of oxygen is lower and there is more free hemoglobin. 40. What is hemoglobin F? Why does the fetus need a different hemoglobin? Hemoglobin F is the hemoglobin found in the mammalian fetus and hemoglobin A is the normal hemoglobin. Hemoglobin F has higher affinity for oxygen. The fetus needs hemoglobin capable of extracting oxygen from the mother’s circulation. Therefore the fetus uses hemoglobin F since it has higher affinity for oxygen than the mother’s hemoglobin. 41. In high altitudes is it necessary for the blood to have more or less hemoglobin? In high altitudes the air is rarefied and oxygen concentration is lower than in low altitudes. In this situation the efficiency of the respiratory system must be greater and thus the organism synthesizes more hemoglobin (and more red blood cells) trying to get more oxygen. This phenomenon is known as compensatory hyperglobulinemia. The compensatory hyperglobulinemia is the reason why athletes that will compete in high altitudes need to arrive in the place some days before the event so there is time for their body to make more red blood cells and they will be less affected by the effects of the low atmospheric oxygen concentration (fatigue, reduced muscular strength). 42. What is the substance that stimulates the production of red blood cells? Which is the organ that secretes it? Under what conditions does this secretion increase? The substance that stimulates the production of red blood cells by the bone marrow is erythropoietin. Erythropoietin is a hormone secreted by the kidneys. Its secretion is increased when there is deficient tissue oxygenation (tissue hypoxia) caused either by reduced oxygen availability (as it occurs in high altitudes) or by internal diseases, as in pulmonary diseases. 43. Why is carbon monoxide toxic for humans? Hemoglobin “likes” carbon monoxide (CO) much more than it likes oxygen. When there is carbon monoxide in the inhaled air it binds to hemoglobin forming carboxyhemoglobin by occupying the binding site where oxygen would bind. Due to the higher hemoglobin affinity for carbon monoxide thus (e.g., in intoxication from car exhausts) there is no oxygen transport and the individual undergoes hypoxia, loses conscience, inhales more carbon monoxide and may even die. Intoxication by carbon monoxide is an important cause of death in fires and in closed garages. 44. What is the stage of cellular respiration during which carbon dioxide is liberated? In aerobic cellular respiration the release of carbon dioxide happens in the transformation of pyruvic acid into acetyl-CoA (two molecules) and in the Krebs cycle (four molecules). For each glucose molecule, six carbon dioxide molecules are made. 45. How is carbon dioxide released by cellular respiration transported from the tissues to be eliminated through the lungs? In vertebrates almost 70% of the carbon dioxide is transported by the blood in the form of bicarbonate, 25% bound to hemoglobin and 5% dissolved in the plasma. 46. What is the difference between double closed circulation and simple closed circulation? Double closed circulation, or closed circulation, is that in which the blood circulates through two associated and parallel vascular systems: one that carries blood to and takes blood from the peripheral tissues (the systemic circulation) and the other that carries blood to and takes blood from the tissues that perform gas exchange with the environment, e.g, the lungs (pulmonary circulation). Double circulation occurs in amphibians, reptiles, birds and mammals. Simple closed circulation, or simple circulation, is the one in which the tissues that perform gas exchange are associated in series with the systemic circulation, as in fishes. 47. How many chambers does the fish heart have? The fish heart is a tube made of two consecutive chambers: one atrium and one ventricle. 48. Does the fish heart pump venous or arterial blood? The venous blood coming from the tissues enters the atrium and passes to the ventricle that then pumps the blood towards the gills. After oxygenation in the gills the arterial blood goes to the tissues. So the fish heart pumps venous blood. 49. Why is the fish circulation classified as a simple and complete circulation? Complete circulation is that in which there is no mixture of venous blood and arterial blood. Simple circulation is that in which the blood circulates only in one circuit (as opposed to the double circulation that have two circuits, the systemic circulation and the pulmonary circulation). In fishes the circulatory system is simple and complete. 50. How many chambers does the human heart have? The right ventricle pumps the blood back to the lungs where it is oxygenated and sent to the left atrium. From there it heads over to the left ventricle. The left ventricle is responsible for sending the blood to the aorta, which then sends oxygenated blood throughout the entire body. With each pump of the heart, between 60 and 70 milliliters of blood are sent throughout the body. This equals around four to five liters per minute. How many heart chambers does the amphibian heart have? The amphibian heart has three heart chambers: two atria and one ventricle. 51. Why can the amphibian circulation be classified as double and incomplete? The amphibian circulation is double because it is composed of systemic and pulmonary circulations: respectively, heart-tissues-heart and heart-lungs-heart. Since amphibians have only one ventricle in the heart, venous blood taken from the tissues and arterial blood coming from the lungs are mixed in the ventricle that then pumps the mixture back to the systemic and to the pulmonary circulations. The amphibian circulation is classified as incomplete because venous and arterial blood mix in the circuit. The blood oxygenation in amphibians occurs also in the systemic circulation since their skin is a gas exchange organ. 52. What is the difference between the amphibian heart and the reptile heart? The reptiles have double and incomplete circulation too, three heart chambers (two atria and one ventricle). The reptile heart however presents the beginning of a ventricular septation that partially separates a right and left region of the chamber. With the partial ventricular septation the mixture of arterial with venous blood in the reptile heart is less than in amphibians. 53. How many chambers do the bird heart and the mammalian heart have? Concerning temperature maintenance what is the advantage of the double and complete circulation of these animals? The bird and the mammalian hearts are divided into four chambers: right atrium, right ventricle, left atrium and left ventricle. Birds and mammals are homeothermic, i.e., they control their body temperature. The four-chambered heart and the double circulation provide the supply of more oxygenated blood to the tissues making possible a higher metabolic rate (mainly cellular respiration rate). Part of the energy produced by the cellular respiration is used to maintain the body temperature. 54. Concerning the mixture of arterial with venous blood what is the difference between the human fetal circulation and the adult circulation? In the human fetal circulation there are two communications between arterial and venous blood characterizing an incomplete circulation. One of them is the oval foramen, an opening between the right and the left atria of the fetal heart. The other is the arterial duct, a short vessel connecting the pulmonary artery to the aorta. These communications close a few days after birth and so they are not present in the adult heart. 55. How is heart contraction triggered? Heart contraction is independent from neuronal stimulus (although it can be modulated by the autonomous nervous system). In the heart there are pacemaker cells that trigger by themselves the action potentials that begin the muscle contraction. These cells are concentrated at two special points of the heart: the sinoatrial node (SA node) located in the superior portion of the right atrium and the atrioventricular node (AV node) located near the interatrial septum. The action potentials generated by depolarization of the SA node cells propagate cell to cell throughout the atria producing the atrial contraction. The atrial depolarization also propagates to the AV node that then transmits the electric impulse to the ventricles through specialized conduction bundles of the interventricular septum (the bundle of His) and then to the Purkinje fibers of the ventricle walls causing ventricular contraction. (The atrial contraction precedes the ventricular contraction for blood to fill the ventricles before the ventricular contraction.) The repolarization of the SA node makes the atria relax and then the ventricles relax too Here are further guidelines. |
Human Body Quiz
|
1. How many total human skeletal bones are there? 2. The colored part of the human eye that controls how much light passes through the pupil is called the? 3. What is the name of the substance that gives skin and hair its pigment? 4. The muscles found in the front of your thighs are known as what? 5. True or false? The two chambers at the bottom of your heart are called ventricles. 6. What substance are nails made of? 7. What is the human body’s biggest organ? 8. The innermost part of bones contains what? 9. True or false? An adult human body has over 500 bones. 10. How many lungs does the human body have? 11. Another name for your voice box is the? 12. The two holes in your nose are called? 13. Your tongue is home to special structures that allow you to experience tastes such as sour, sweet, bitter and salty, what is their name? 14. The bones that make up your spine are called what? 15. The shape of DNA is known as? 16. The flow of blood through your heart and around your body is called? 17. The bones around your chest that protect organs such as the heart are called what? 18. What is the name of the long pipe that shifts food from the back of your throat down to your stomach? 19. True or false? Your ears are important when it comes to staying balanced. 20. The outside layer of skin on the human body is called the? 21. The largest and heaviest bone in the body is the: 22. How many types of muscles are there in the human body and what are they? 23. What is the name of the biggest part of the human brain? Human Body Quiz Answers 1. There are 206 named bones a normal, complete, adult human skeleton. 2. Iris 3. Melanin 4. Quadriceps 5. True 6. Keratin 7. The skin 8. Bone marrow 9. False (there are 206) 10. 2 11. Larynx 12. Nostrils 13. Taste buds 14. Vertebrae 15. A double helix 16. Circulation 17. Ribs 18. The esophagus 19. True 20. Epidermis 21. The femur, or thigh bone, is the longest, heaviest, and strongest bone in the entire human body. 22. Three.
Smooth Cardiac 23. The cerebrum Questions you need to answer. How many muscles are there in the human body? How many days does it take for your body to rid itself of an alcoholic beverage? How many identifiable bones are there in the human body? What type of nerves send signals to the brain? Triceps, biceps and quadriceps are examples of what kind of muscle? There are how many Cervicle discs? There are how many Thoracic discs? There are how many Lumbar discs? The Sternum holds how many ribs together? |
Dermatology
Integumentary system
A to Z All Skin Conditions
A|B|C|D|E|F|G|H|I|J|K|L|M|N|O|P|Q|R|S|T|U|V|W|X|Z
Acne- Full term is 'Acne Vulgaris' and this is one of the commonest conditions which Dermatologists are asked to see. More Details >>Actinic Keratosis- Also known as Solar Keratosis or sometimes "AKs". More Details >>Allergy- Allergic rashes, hives, urticaria, etc are a major problem world wide. More Details >>Alopecia- This is the medical term for hair loss - there are many different types of hair loss resulting from a wide variety of different conditions. More Details >>Androgenetic Alopecia- This means hair loss due to male-pattern baldness and is seen in both men but also in post menopausal women . More Details >>Alopecia Areata- Very smooth patches of hair loss affecting the scalp or beard areas and often moving from site to site. More Details >>Age Spots- Also known as Solar Lentigos or Liver Spots -Exaggerated brown freckles typically occuring on the face or the backs of the hands More Details >>Athletes Foot- Scaly itchy rash often between the toes sometimes known as "Tinea" which represents a fungal infection of the skin. More Details >>Atopic- The disorders of asthma, eczema and hay fever More Details >>Balanitis- Sore redness or shinyness of the tip of the penis. More Details >>Basal Cell Carcinoma- This condition also known as a rodent ulcer is the commonest skin cancer. It is usually not very serious and can be treated. More Details >>Benign- This medical term means innocent or non seriousBlister- A superficial balloon of skin on the surface containing clear fluid. Usually these are single lesions but in rare diseases there can be many blisters on the skin for example in pemphigoid. More Details >>Bowens Disease- Usually seen on sunshine exposed areas of skin (backs of the hands, forearms, upper shoulders etc). Usually a slightly thickened red and scaly patch of skin which fails to repond to simple moisturisers. More Details >>Candida- Commonly known as "thrush" - depending on which area of the body is involved eg vagina, mouth, etc (the condition can look very different)Cold Sores (Herpes)- Medically known as "herpes" and is due to the herpes simplex virus causing tingling or painful blisters recurring in the same body position eg the lips time after time. More Details >>Crabs- Also known as "body lice" or "pubic lice" - can be seen small black dots on the skin or hairs.Mo re Details >>Cysts- Smooth 1-2 centimetre swellings just below the skin surface usually on the upper trunk and commonly on the scalp. More Details >>Darker Skin PatientsEven common disorders can look very different in darker skinned patients compared with white skin patients. More Details >>Dermatitis- This means precisely the same as eczema to Dermatologists - see Eczema More Details >>Dermatofibroma- Quite common small very firm 0.6 centimetre skin lesions sometimes also known medically as Histio Cytomas.Drug Reactions(to medications) - Usually a very widespread red irritable rash resuls from taking oral medication for example antibiotics. Many different drugs and medications can be responsible. More Details >>Eczema- Itchy inflammation of the skin for any reason but most typically atopic (genetically linked). More Details >>Folliculitis- This can occur on any area of the body and is due to bacteria down inside the hair follicles. More Details >>Fungus- Fungal infections can take many forms on the skin including athletes foot and is often medically known as Tinea. More Details >>Genital Fungal Infections- More Details >>Genital Skin Disease- Many common skin diseases can affect the genitals for example eczema and psoriasis. However, other common infections can also affect the genitals. More Details >>Genital Molluscum. More Details >>Genital Warts -these can look very different. More Details >>Herpes Simplex (Cold Sores)- This viral discorder causing small painful blisters can affect any area of the skin but most typically the mouth and lips and also the genital skin - see Cold Sores. More Details >>Herpes Zoster (Shingles)- A potentially very painful blistering condition affecting the face or body and caused by a virus affecting the nerve endings in the skin. More Details >>Histo Cytomas- also known medically as Dermatofibroma.Hives- see Urticaria. More Details >>Hyperhidrosisalso known as excessive sweating. More Details >>Impetigo- A bacterial infection of the skin often around the nose and mouth but can spread. More Details >>Intertrigo- A red discharging rash affecting hot sweaty skin. More Details >>Kaposis Sarcoma- One centimetre purple nodules on the skin, sometimes associated with HIV infection. More Details >>Keratosis- There are many types of Keratosis which simply means scaly skin condition and these include Actinic Keratosis or Seborrhoeic Keratosis.Keratoacanthoma- A rapidly growing exaggerated warty lesion suggesting squamous cell carcinoma in some patients. More Details >>Kerion- a severe fungal infection of the scalp causing inflammation and hair loss. More Details >>Leg Ulcers (Stasis Dermatitis)- A very common cause of skin break down around the ankles and lower legs often due to obvious or alternatively, hidden, varicose veins. More Details >>Lentigo- An exaggerated freckle which is larger or darker than a standard freckle.. More Details >>Lesion/Lump- A part or swelling of the skin that has suffered through injury or disease. More detailsLichen Planus- An itchy skin rash which can mimick any of the common diseases - eczema, psoriasis, scabies, etc. More Details >>Lichen Sclerosus- A rare but important skin disease becaue it can affect the genital skin and look very unusual at other sites. More Details >>Liver spots- also known as age spots or solar lentigos. More Details >>Malignant-This medical term means cancerous or having the potential to spread or be serious.Mask of pregnancy- See Melasma. More Details >>Melasma- Exaggerated grey-brown pigmentation across the forehead and face. More Details >>Melanoma- Irregular pink brown, black or purple skin growths often arising from a pre-existing mole. More Details >>Molluscum- Small shiny warty lesions showing in groups anywhere on the skin. More Details >>Mole- See Naevus. More Details >>Naevus- Medical term for Mole - flat or elevated, pink brown or darker skin lesions usually growing during the first, second and third decades of life. Patients with many naevi (for example over 50) do need to be highly self-observant about the possibility of malignant melanoma development. More Details >>Nail Disease- The two commonest conditions causing nail disorders are fungal infections and psoriasis. More Details >>Pemphigoid- Pemphigoid/Pemphigus - rare conditions of the skin causing unexplained blisters More Details >>Photo Sensitivity- Means an irritation by sunlight or an exaggerated tendency to very easy sunburn. More Details >>Pityriasis Rosea- A widespread rapidly developing skin eruption sometimes resembling psoriasis. More Details >>Pityriasis Versicolor- A non-troublesome widespread eruption usually on the upper body and around the armpits. More Details >>Pompholyx- A blistering kind of eczema typically affecting the palms of the hands or the soles of the feet. More Details >>Pruritus- The medical term for "itch" - there are very many causes. More Details >>Psoriasis- A widespread scaly eruption affecting any area of the body and often running in families . More Details >>Pubic Lice- Commonly known as crabs - tiny insects affecting the hairs of the body. More Details >>Pyogenic Granuloma- A rapidly growing fragile and bleeding pink/purple nodule. More Details >>Rash- Use the Body Map to narrow your searchRodent Ulcer- Please see basal cell carcinoma. More Details >>Rosacea- This is a very common condition of adult life. The face and nose are the commonest sites. More Details >>Scabies- A widespread itchiness of the skin usually associated with patchy tiny red irritated lesions scattered widely around the body. More Details >>Seborrhoeic Dermatitis- A type of red irritated dermatitis usually affecting the centre of the body from the eyebrows down the nose and sometimes on to the centre of the upper face and body. More Details >>Seborrhoeic Keratosis- Benign Warty Brown marks on the skin . More Details >>Shaving rash- See Follicitis. More Details >>Shingles- A potentially very painful blistering condition affecting the face or body and caused by a virus affecting the nerve endings in the skin. See Herpes Zoster. More Details >>Skin Allergy- This comes in many different forms and can be generated by either outside skin contact or internal eating or drinking of something creating the allergy. More Details >>Skin Cancer-Please see the 3 commonest - Melanoma >>, Basal Cell Carcinoma>>, Squamous Cell Carcinoma >>.Skin Tags- Tiny little growths of skin often under the armpits or beneath the breasts. More Details >>Solar Lentigo- Also known as Age Spots or liver spots - Exaggerated brown freckles typically occuring on the face or the backs of the hands More Details >>Spots-See Folliculitis. More Details >>Squamous Cell Carcinoma- Irregular thickened red scaly lesions usually on sunshine exposed areas. More Details >>Stasis Eczema- Itchy or sore redness of the ankles or lower legs often associated some years later with varicose veins. More Details >>Sunbeds- Artificial ultra violet light cabinets giving suntans. More Details >>Sun Exposure- The sun gives benefits but also can damage the skin if exposed excessively for example skin cancer. More Details >>Sunshine & Protection- See Photo Sensitivity. More Details >>Sunshine Sensitivity- See Photo Sensitivity. More Details >>Telogen Effluvium- Reduced hair loss across the whole scalp following pregnancy or an illness. More Details >>Thread Veins- Visible blood vessels running through the surface of the skin usually affecting the legs but also across the nose and face. More Details >>Thrush- See Candida. More Details >>Tinea- Tinea refers to a fungal infection of the skin the most common of which is athletes foot but this can occur on other body sites as well - tinea can also affect the scalp where it is known as Kerion. More Details >>Urticaria (Hives)- An itchy condition. Blotchy, red and sometimes elevated skin rash moving from site to site and changing each day. More Details >>Verruca- A wart affecting the toes and soles of the feet More Details >>Warts- Usually on the fingers but can occur anywhere. More Details >>Zoster- See Herpes Zoster and Shingles. More Details >> |
Endocrinology
Endocrine System
Endocrine organs and known secreted hormones
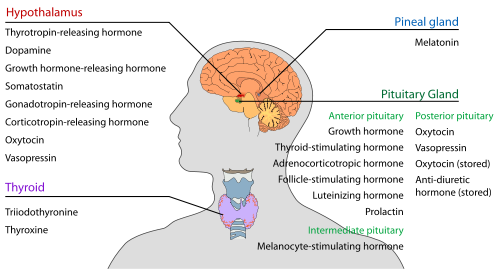 Endocrine glands in the human head and neck and their hormones Alimentary system 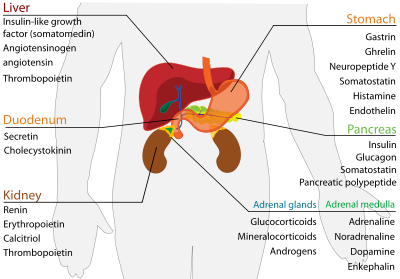 Reproductive Woman 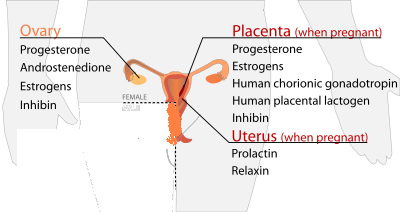 Man 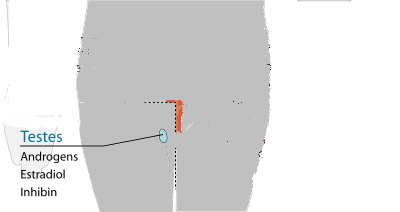 Calcium regulation 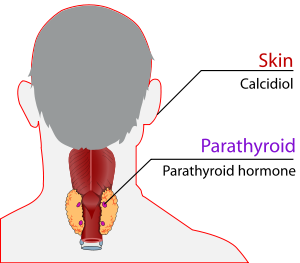 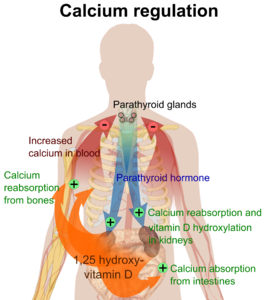 Targets 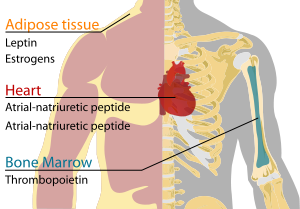 An Introduction to the Endocrine System 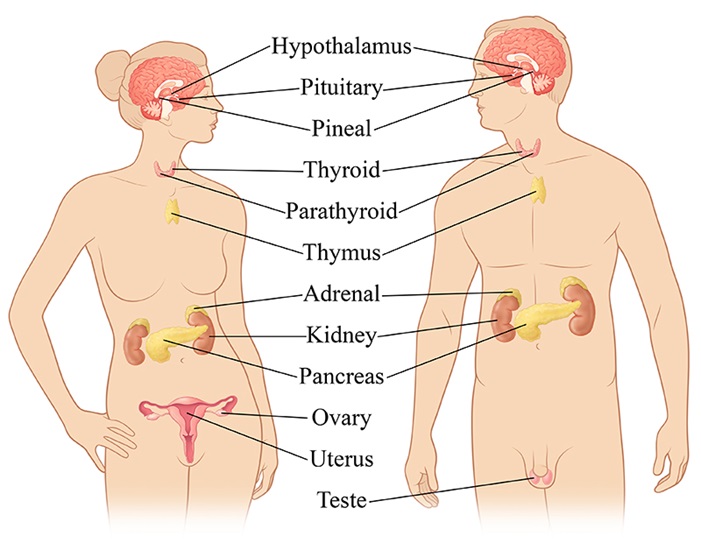 The endocrine system controls the way your body functions. It produces hormones that travel to all parts of your body to maintain your tissues and organs. Here are a few of the areas governed by the endocrine system: Reproduction Responses to stress and injury Growth and sexual development Body energy levels Internal balance of body systems Bone and muscle strength Your endocrine system produces, stores and releases hormones. When everything goes smoothly, your body functions properly. The Glands of the Endocrine System Your endocrine system is made of many glands and organs. They have different functions, and work together to keep you healthy. These are the glands of your endocrine system: Adrenal glands - influence the way your body uses energy, they also release a hormone called adrenaline when you are under stress Hypothalamus - part of your brain that controls hormone production by releasing different chemicals to the pituitary gland Ovaries - produce estrogen and progesterone in women, and also release egg cells Pancreas - releases the insulin your body needs to metabolize sugar; problems with the pancreas can lead to diabetes Parathyroid - located behind the thyroid gland, they are essential for proper bone development Pineal gland - connects the endocrine system with the nervous system; produces several important hormones, including melatonin, important to sleep/wake cycles and sexual development Pituitary gland – likely the most important gland in your body, it is crucial to growth, mental development and reproduction; influences or controls the rest of your endocrine system Testes - produce the hormone testosterone; in men, testosterone maintains sperm production and bone mass Thymus - crucial to normal immune function in childhood; once a child reaches puberty, its tissue is replaced by fat Thyroid gland – located in the front of your neck, it releases hormones that control your metabolism and govern the way your body uses energy Endocrine Organs Several organs are vital to your endocrine system. They produce, store and excrete hormones to maintain the proper function of your body. The placenta is the organ that provides the connection between a pregnant mother and the infant in her womb. It makes changes to a woman's body to better nourish her baby and prepare the mother for delivery. Your skin, liver and kidneys work together to produce vitamin D. Vitamin D is produced when your skin is exposed to ultraviolet light. In the liver and kidneys, it becomes a chemical known as calcitriol, which maintains proper levels of calcium and phosphorus in your body. Your stomach and small intestine secrete many hormones tied to eating and digestion. Disorders in the system can cause you to eat too little or too much food, and may lead to weight disorders. Diabetes Symptoms Urinating often Symptoms of Hypothyroidism Here are further guidelines. |
Gastroenterology
Digestive System
|
Mouth Disorders | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Mouth Disorders | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Oral human symptoms | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Oral health services or dental services and role of primary care physician. | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Oral Health | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Parts of the Mouth | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Questions a primary care physician should ask an individual claiming to be a dentist before any referral. | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Teeth Numbers Chart | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Toothpaste | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Teeth Conditions | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Oral health services or dental services and role of primary care physician. What type of physician takes care of oral health? Ideally, a primary care physician has to take care of oral health. In certain situations, a referral to a highly competent dentist may be required, depending on the diagnosis, recommended treatment and expertise of dentist. What is the human mouth made up of? 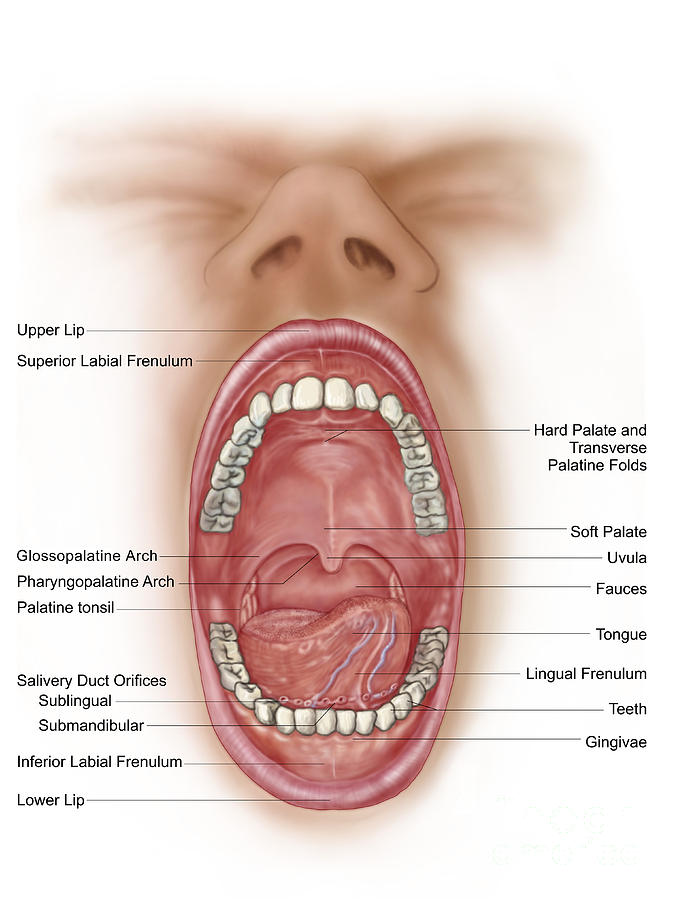
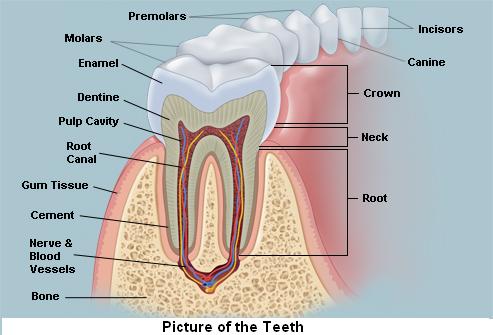
Human mouth is made up of lips, tongue, gums, teeth, cheek lining, mouth floor, hard palate, soft palate, uvula, and tonsils. Parts of the Mouth
How does your mouth help you? Your mouth helps you breathe, talk, swallow, taste, and chew. Symptoms involving the mouth are extremely common and affect people in all age groups. Oral human symptoms What can be oral symptoms of a human being? | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Bad breath | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Dry mouth or xerostomia | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Eroded enamel | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Eroded teeth | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Frictional keratosis | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Loose teeth | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Lichen planus | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Mouth sore | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Oral thrush (fungal infection in the mouth) | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Puffy gums | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Smoker's keratosis | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Sour taste in your mouth | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Swollen gum | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Toothache | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Toothache with swelling and/or fever (Abscess toothache) | ||||||||||||||||||||||||||||||||||||||||||||||||||
| White patches in the mouth | ||||||||||||||||||||||||||||||||||||||||||||||||||
| White or brown lines on childrens' teeth | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Oral human symptoms are focused around lips, teeth, gums, tongue, and buccal cavity.
Throat symptoms are categorized separately. Bad breath What causes bad breath? Some types of bad breath, such as "morning mouth," are considered to be fairly normal, and they usually are not health concerns. The "morning mouth" type of bad breath occurs because the saliva that regularly washes away decaying food and odors during the daytime diminishes at night while you sleep. Your mouth becomes dry, and dead cells adhere to your tongue and to the inside of your cheeks. Bacteria use these cells for food and expel compounds that have a foul odor. In addition, bad breath can be caused by the following: Poor dental hygiene — Infrequent or improper brushing and flossing can leave food particles to decay inside the mouth. Infections in the mouth — Periodontal (gum) disease Respiratory tract infections — Throat infections, sinus infections, lung infections External agents — Garlic, onions, coffee, cigarette smoking, chewing tobacco Dry mouth (xerostomia) — This can be caused by salivary gland problems, medications or by "mouth breathing." Systemic illnesses — Diabetes, liver disease, kidney disease, lung disease, sinus disease, reflux disease and others Psychiatric illness — Some people may perceive that they have bad breath, but it is not noticed by oral-health-care professionals or others. This is referred to as "pseudohalitosis." Symptoms A person may not always know that he or she has bad breath. This phenomenon is because odor-detecting cells in the nose eventually become accustomed to the constant flow of bad smells from the mouth. Others may notice and react by recoiling as you speak. Other associated symptoms depend on the underlying cause of bad breath: Poor dental hygiene — Teeth are coated with film or plaque, food debris trapped between teeth, pale or swollen gums Infections in the mouth — Gums may be red, swollen and bleed easily, especially after brushing or flossing; pus may drain from between teeth; a pocket of pus (abscess) at the base of a tooth; loose teeth or a change in "fit" of a denture; painful, open sores on the tongue or gums Respiratory tract infections — Sore throat, swollen lymph nodes ("swollen glands") in the neck, fever, stuffy nose, a greenish or yellowish nasal discharge, a mucus-producing cough External agents — Cigarette stains on fingers and teeth, a uniform yellow "coffee stain" on teeth Dry mouth — Difficulty swallowing dry foods, difficulty speaking for a prolonged period because of mouth dryness, a burning sensation in the mouth, an unusually high number of dental caries, dry eyes (in Sjögren's syndrome) Systemic (bodywide) illnesses — Symptoms of diabetes, lung disease, kidney failure or liver disease Diagnosis A dentist or physician may notice the patient's bad breath while the patient is discussing his or her medical history and symptoms. In some cases, depending on the smell of the patient's breath, the dentist or physician may suspect a likely cause for the problem. For example, "fruity" breath may be a sign of uncontrolled diabetes. A urine-like smell, especially in a person who is at high risk of kidney disease, can sometimes indicate kidney failure. Your dentist will review your medical history for medical conditions that can cause bad breath and for medications that can cause dry mouth. Your dentist also will ask you about your diet, personal habits (smoking, chewing tobacco) and any symptoms, including when the bad breath was noticed and by whom. Your dentist will examine your teeth, gums, oral tissues and salivary glands. He or she also will feel your head and neck and will evaluate your breath when you exhale from your nose and from your mouth. Once the physical examination is finished, your dentist may refer you to your family physician if systemic problems are the most likely cause. In severe cases of gum disease, your dentist may recommend that you be seen by a periodontist (dentist who specializes in gum problems). You will need diagnostic tests if the doctor suspects a lung infection, diabetes, kidney disease, liver disease or Sjögren's syndrome. Depending on the suspected illness, these tests may include blood tests, urine tests, X-rays of the chest or sinuses, or other specialized testing. Here are further guidelines. http://www.qureshiuniversity.com//badbreath.html Oral thrush (fungal infection in the mouth) 

Oral thrush is an infection in the mouth caused by a yeast germ called Candida. It is not usually serious and can generally be cleared with treatment. What is oral thrush? Thrush is an infection caused by a yeast germ called Candida. The mouth is a common site where Candida causes infection. Candidal infection in the mouth is called oral thrush. Other common sites for thrush to develop are the vagina, nappy area, and nail folds. (See separate leaflets called Vaginal Thrush, Candidal Skin Infection and Nappy Rash for more details about these other types of thrush.) In adults, thrush can cause an uncomfortable burning sensation in the mouth and throat. Oral thrush is an infection of yeast fungus, Candida albicans, in the mucous membranes of the mouth. Strictly speaking, thrush is only a temporary candida infection in the oral cavity of babies. But we have, for this purpose, expanded the term to include candida infections occurring in the mouth and throat of adults, also known as candidiasis or moniliasis. Who develops oral thrush? Small numbers of Candida commonly live on healthy skin and in a healthy mouth. They are usually harmless. Healthy people do not normally develop oral thrush. However, certain situations or conditions may cause an overgrowth of Candida which can lead to a bout of oral thrush. These include: •Being a baby. Oral thrush is quite common in young babies. •Wearing dentures, especially if they are not taken out at night, not kept clean, or do not fit well and rub on the gums. •A course of antibiotic medicine. Antibiotics will kill harmless germs (bacteria) which live in the mouth. They do not kill Candida which may multiply more easily if there are fewer bacteria around. •Excessive use of antibacterial mouthwash (for similar reasons to above). •Taking steroid tablets or inhalers. •Having a dry mouth due to a lack of saliva. This may occur as a side-effect from certain medicines (such as antidepressants, antipsychotics, chemotherapy medicines), following radiotherapy to the head or neck, or as a symptom of Sjögren's syndrome. •Having diabetes. •Having severe anaemia. •Lacking iron, folate or vitamin B12. •Having a poor immune system. •Being frail or in generally poor health. •Smoking. Smokers are more likely to develop oral thrush. Oral thrush is not contagious. You cannot pass on oral thrush to other people. How do you get oral thrush? Candida is present in the oral cavity of almost half of the population. Everyone who wears dentures will have candida, without necessarily suffering any ill effects. Candida doesn't become a problem until there's a change in the chemistry of the oral cavity that favours candida over the other micro-organisms that are present. These changes can occur as a side-effect of taking antibiotics or drug treatment, such as chemotherapy. These changes can also be caused by certain conditions – such as diabetes, drug abuse, malnutrition – and as a consequence of immune deficiencies relating to old age or infection. Furthermore, people whose dentures don't fit well can sustain breaks in the mucous membranes in their mouth, which can act as a gateway for candida. People who suffer from this problem often have moist, pale pink spots on their lips, known as angular cheilitis, which is an indication of a candida infection. What are the symptoms of oral thrush? •The classical symptom is white spots that develop in your mouth. The spots may join together to form larger spots called plaques. They may become yellow or grey. If you wipe off a spot, the underlying tissue may be red but it is not usually sore or painful. •Often there are no white spots. Areas in your mouth may just become red and sore. This more typically occurs if you develop thrush after taking antibiotics or steroids. •Denture wearers may develop an area of persistent redness under a denture. •You may develop sore, cracked, red areas just outside your mouth. This mainly affects the angle where the upper and lower lips meet (angular stomatitis). •Some mild oral thrush infections are painless. However, sometimes oral thrush is quite sore and can make eating and drinking uncomfortable. Some babies with oral thrush may drool saliva, or not be able to feed properly because of soreness. •Taste can be affected in some people with oral thrush. White, cream-coloured, or yellow spots in the mouth. The spots are slightly raised. There is normally no pain in the area underneath the spots. If you scrape off these spots, they leave small wounds that bleed slightly. In adults, thrush can cause an uncomfortable burning sensation in the mouth and throat. Who is at special risk? Newborn babies. Denture users. Adults with diabetes or other metabolic disturbance. People with a dry mouth relating to side-effects of their medication (eg anti-psychotics) or medical conditions (eg Sjogren’s Syndrome). People undergoing antibiotic or chemotherapy treatment. People prescribed oral steroid medication or steroid metered dose inhalers. Drug users. People with poor nutrition. People with an immune deficiency. How does the doctor diagnose oral thrush? How is oral thrush diagnosed? In babies, thrush is usually diagnosed on the basis of the clinical picture. Occasionally, in order to make a diagnosis, the doctor will scrape the baby's tongue and send the sample for analysis. In adults, your doctor will usually diagnose oral thrush by your typical symptoms and the typical appearance in your mouth. No investigations are usually needed to diagnose oral thrush. However, your doctor may sometimes suggest a blood test to look for certain conditions that may make you more likely to develop oral thrush. For example, a blood test to see if you are lacking iron, vitamin B12 or folate. If oral thrush does not respond to treatment (see below), your doctor may suggest that they take a sample (swab) from inside your mouth. The swab is then sent to the laboratory to be examined under a microscope. They can also try to grow the Candida in the laboratory. Occasionally, a biopsy is needed to confirm a diagnosis of oral thrush. A small sample is taken from the white patches inside your mouth and this can be examined under a microscope. What is the treatment for oral thrush? In Babies, oral thrush may clear spontaneously without treatment and may be prevented by sterilising all feeding equipment and mouth toys. It's been suggested that by giving the child sterilised water immediately following a milk feed, residual milk in the mouth is rinsed away, reducing the population of candida within the oral cavity. In other circumstances, the condition that caused the thrush must be brought under control. Once the condition that caused the oral thrush has been treated, the thrush itself can be cured. Treatment is with antifungal medicines, in the form of pastilles that are sucked or oral suspensions that are held in the mouth before swallowing. These allow the antifungal agent to act locally in the mouth. Examples include nystatin (eg Nystan oral suspension), or miconazole (eg Daktarin oral gel). In certain complicated cases, or if the infection spreads, systemic treatment will be necessary in the form of antifungal tablets, or perhaps in the form of injections. Coping with the symptoms of oral thrush Thrush can make the mouth so sensitive that it's impossible to perform regular oral hygiene. Use a very soft toothbrush. It can often help to rinse the mouth with a diluted solution of 3 per cent hydrogen peroxide. Locally applied treatment For mild oral thrush, the usual treatment that is tried first is miconazole mouth gel for seven days. Sometimes a two-week course is needed. Nystatin drops are another option if miconazole gel cannot be used (for example, if you are known to be allergic to it). Follow the instructions in the packet: •The gel or drops should be used after you have eaten or drunk. •Smear a small amount of gel on to the affected areas, with a clean finger, four times a day. •With the drops, you use a dropper to place the liquid inside your mouth on to the affected areas four times a day. •Ideally, you should not eat or drink for about 30 minutes after using either the gel or the drops. This helps to prevent the medicine from being washed out of your mouth too soon. Anti-thrush tablets Tablets that contain a medicine called fluconazole can also help to clear fungal and thrush infections from the body. Tablets tend to be used in more severe or serious cases. For example, for people with a poor immune system who develop extensive oral thrush. Tablets are usually prescribed for seven days and this will usually clear oral thrush. Adjustment of other medication If you are taking other medication that may have caused oral thrush, such as steroids or antibiotics, your doctor may need to change this medication or reduce the dose to help clear up your thrush. Referral to a specialist Your doctor may suggest that he or she refer you to (or ask the advice of) a specialist if: •The above measures do not help to clear your oral thrush infection. •You have particularly severe infection or other health problems (for example, you are undergoing chemotherapy or are taking other medicines that weaken your immune system). The specialist may suggest other treatments for oral thrush. For example, medicines such as itraconazole, ketoconazole or amphotericin. Can oral thrush be prevented? It may be possible to alter one or more of the situations mentioned above to help prevent further bouts of oral thrush. For example: •If you have diabetes - good control of your blood sugar level reduces the risk of thrush and other infections. •If you use steroid inhalers - having a good inhaler technique and using a spacer device may reduce the risk of thrush. Also, rinse your mouth after using the inhaler, to help remove any medicine particles left in your mouth. Ask your doctor about reducing your dose of steroid in your inhaler to the lowest level needed to control your asthma. •If you wear dentures: •Leave your dentures out overnight, or for at least six hours daily. Constant wearing of dentures, and not taking them out at night, is thought to be one of the most common causes of oral thrush. •Clean and disinfect dentures daily. To clean, use soapy water and scrub the dentures with a soft nailbrush on the fitting surface - that is, the non-polished side. Then soak them in a disinfecting solution. The type of solution and the time they should be soaked for will be advised by your dentist. Rinse the dentures after disinfecting them, and then allow the dentures to air dry before wearing them again. Drying like this helps to kill any Candida that might be stuck to the dentures. •Clean the inside of your mouth (where the dentures sit) with a soft brush. •See a dentist if the dentures do not fit well. •If you take medication which causes a dry mouth - take frequent sips of water. (See separate leaflet called Dry Mouth for more details.) •Tips to prevent oral thrush in babies are included in the separate leaflet called Oral Thrush in Babies. •If you are found to have anaemia or low levels of vitamin B12, folate or iron, treating this may help to prevent oral thrush in the future. •If you are a smoker, quitting smoking may help to prevent further bouts of oral thrush. (See separate leaflet called Tips to Help You Stop Smoking for more details.) •Certain groups of people may be given anti-thrush tablets to help to prevent oral thrush. For example, people who are on medication to suppress their immune system or who are receiving chemotherapy. Toothache What causes a toothache? While tooth decay is often the primary cause of a toothache, it's important for you to have a complete oral examination to determine the cause. Other causes of a toothache can include the following: •Infection •Gum disease •Grinding teeth (bruxism) •Tooth trauma •An abnormal bite •Tooth eruption (in babies and school-age children) TMJ/TMD (Temporomandibular Joint Disorder), sinus or ear infections, and tension in the facial muscles can cause discomfort that resembles a toothache, but often these health problems are accompanied by a headache. Pain around the teeth and the jaws can be symptoms of heart disease such as angina. If your dentist suspects a medical illness could be the cause of your toothache, he or she may refer you to a physician. If you have a toothache, you may have a cavity or advanced gum disease. The first sign of decay may be the pain you feel when you eat something sweet, very cold or very hot. If the pulp – the inside of the tooth that has tissue and nerves – has become irritated, this can cause pain in your tooth. What symptoms accompany a toothache? Because the symptoms of a toothache may resemble other medical conditions or dental problems, it can be difficult to diagnose the cause without a complete evaluation by your dentist. If you notice pus near the source of the pain, your tooth may have become abscessed, causing the surrounding bone to become infected. Or the pus could indicate gum disease, which is usually characterized by inflammation of the soft tissue, bleeding gums and abnormal loss of bone surrounding the teeth. Contact your dentist immediately if you have any of the following symptoms: •Fever •Difficulty breathing or swallowing •Swelling around the tooth area •Pain when you bite •A foul-tasting discharge •Continuous lasting pain How do I alleviate the pain if I cannot see my dentist right away? Anyone with a toothache should see a dentist at once for diagnosis and treatment. If left untreated, a toothache and the condition that is causing it can worsen. However, if you are unable to schedule an emergency appointment, the following self-care treatment can temporarily alleviate pain and inflammation from a toothache: •Rinse with warm salt water •Gently floss teeth to dislodge any food particles trapped between teeth. •Take an over-the-counter pain reliever such as ibuprofen (Advil®) or acetaminophen (Tylenol®) to relieve pain. •Never put aspirin or any other painkiller against the gums near the aching tooth, as it may burn the gum tissue. •Apply an over-the-counter antiseptic containing benzocaine directly to the irritated tooth and gum to temporarily relieve pain. Direct application of oil of cloves (eugenol) may also help to numb the gums. The oil may be rubbed directly on the sore area, or soak a small piece of cotton and apply it to the sore tooth. •If there has been some trauma to the tooth, a cold compress may be applied on the outside cheek to relieve pain or swelling. How can my dentist help? Your dentist will conduct a complete oral examination to determine the location and cause of the toothache, looking for signs of swelling, redness and obvious tooth damage. He or she may also take x-rays to look for evidence of tooth decay between teeth, a cracked or impacted tooth or a disorder of the underlying bone. Your dentist also may prescribe pain medication or antibiotics to speed the healing of your toothache. If by the time you see your dentist your tooth has become infected, then treatment could require removal of the tooth or a root canal procedure, which involves removing the damaged nerve tissue from the middle of a tooth. Is there a way to prevent a toothache? The key to preventing toothaches is establishing a regular oral hygiene routine and sticking to it. For example, failure to brush and floss regularly after meals can significantly increase your risk of developing cavities, which can cause toothaches. Here are a few tips to help reduce your risk for developing a toothache: •Brush at least twice a day, preferably after meals and snacks. •Floss at least once a day to prevent gum disease. •Visit your dentist regularly for oral examinations and a professional cleaning. Why should a primary care physician be able to diagnose and treat all nonemergency medical conditions? There are thousands of medical conditions. It is impossible to have a separate physician for every medical condition. A primary care physician should be able to diagnose and treat all oral health medical conditions, in addition to other medical conditions. Dental services are actually oral health care services. A primary care physician can provide these services. Mouth disorders. What are other names of oral medical conditions? Mouth disorders. What are examples of mouth disorders? Take a look at this.
Cold Sores  Also called fever blisters, you don't get cold sores from fevers or colds but they can be triggered by them. The virus that causes cold sores is usually passed via a kiss, shared utensils, or other close contact. Over-the-counter creams and ointments may help discomfort and speed healing. Frequent sores may require a prescription. Cold sores are a top mouth problem. Other problems include canker sores, TMJ, bad breath, and mouth cancer. Thrush  Caused by candida yeast, thrush is most common in older adults or babies. But a weakened immune system, antibiotics, diabetes, or certain medications -- such as inhaled corticosteroids -- can give candida a chance to grow wild. Wiping away the patches will cause soreness. See a doctor for a firm diagnosis. Black Hairy Tongue  This painless condition occurs when the little bumps on your tongue grow long and trap bacteria that live in your mouth -- making the tongue look black and hairy. Causes can include antibiotic use, poor oral hygiene, smoking, drinking a lot of tea or coffee, and not producing enough saliva. Brushing the tongue and using a tongue scraper is usually all you need to treat it, though sometimes medication is necessary. Canker Sores  No one knows what causes these small, painful blisters inside your mouth. Triggers include hypersensitivity, infection, hormones, stress, and not getting enough of some vitamins. Also called aphthous ulcers, canker sores can show up on the tongue, cheek, even your gums. They usually last a week or two. Persistent, severe canker sores can be treated with numbing creams, prescription drugs, or dental lasers. Leukoplakia  Leukoplakia is a reaction to an irritant, like rough teeth, badly fitting dentures, smoking, and smokeless tobacco. It can show up as white patches or plaques in the mouth, is usually painless, and can't be scraped off. Leukoplakia can also be a precancerous condition. Persistent patches or other changes in your mouth need a dentist's evaluation. Lichen Planus  A rare rash that shows up as lacy, white patches or red shiny bumps on the inside of the cheeks or tongue could be lichen planus. No one knows what causes it. Generally, mild lichen planus doesn't need any treatment. If it causes pain or ulcers, it can be treated with oral and topical medication. Oral lichen planus can be chronic and may increase the risk for oral cancer. Lichen planus can also affect skin, scalp, nails, and genitals. Geographic Tongue  When parts of your tongue are missing some of their small bumps, you end up with raised and lowered spots, giving your tongue a map-like appearance. The spots can change location, pattern, and size within minutes to hours. Geographic tongue is harmless and can come and go. It usually doesn't need any treatment. If there's pain, over-the-counter pain relievers and anti-inflammatory medications can help. Oral Cancer A mouth sore that doesn't go away. Unexplained numbness in the face, mouth, or neck. Problems chewing, speaking or swallowing. These are a few symptoms of oral cancer. Causes can include smoking cigarettes and using smokeless tobacco, drinking heavily, overexposure to the sun, and a family history of cancer. Oral cancer has also been linked to the human papillomavirus, or HPV. Don't let fear keep you from the doctor -- oral cancer that is caught early is treatable and curable. TMJ 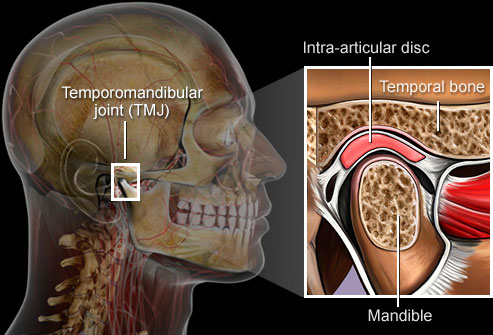 A problem with the jaw called temporomandibular joint syndrome can cause severe pain in the jaw, face, ear, or neck. Clenching, tooth grinding, or injury can all cause TMJ syndrome, but the results are often the same: pain, headaches, dizziness, even trouble swallowing. Treatment may involve rest, moist heat, a mouth guard, medication, or surgery. Chipped Teeth  Munching on ice or hard candies, grinding or clenching teeth, even exposing teeth to heat and cold can lead to chips, cracks, and breaks in your teeth. Tiny chips or cracks may not be a bother. But anything more could lead to pain or permanent tooth damage. Your dentist can offer dental bonding, tooth contouring, porcelain veneers, and crowns to fix badly damaged teeth. Amalgam Tattoo  Ever notice a small blue-gray "stain" in a soft part of your mouth after dental work? Called amalgam tattoos, they occur when a tiny piece of amalgam filling gets embedded in your cheek or gum. The silver in the amalgam leaches into your mouth's soft tissue, resulting in what looks a bit like a tiny tattoo. Amalgam tattoos pose no harm. But if the blue-gray spot grows or changes color, there is a good possibility it may not be an amalgam tattoo. Ask your dentist to check it out. Gum Disease  When periodontal (gum) disease develops, bacteria in plaque accumulate along the gum line. Gingivitis is the first stage of gum disease. Symptoms include red, puffy, and bleeding gums. Proper oral hygiene can help prevent periodontal disease. Smoking, poor diet, and stress can make it worse. Periodontitis The next stage of gum disease is periodontitis, or gum infection. Increased inflammation causes the gums to recede, forming pockets between the teeth and gums. These pockets trap tartar, plaque, and food debris that eventually lead to infection and abscesses. Advanced gum disease damages the bone that supports teeth and is one of the leading causes of tooth loss in adults. See your dentist to treat receding gums. www.qureshiuniversity.com/periodontist.html Aspirin Burn  Ever let an aspirin nestle in your cheek, near an aching tooth? While you may hope this relieves pain faster, instead the acid in the aspirin burns a white, rough lesion into your gums or cheek. Preventing aspirin burn is simple -- swallow those pain relievers! Treatment for aspirin burn is just as basic: Time. Simple burns should heal in about two weeks. Cavities, Abscesses, Discoloration 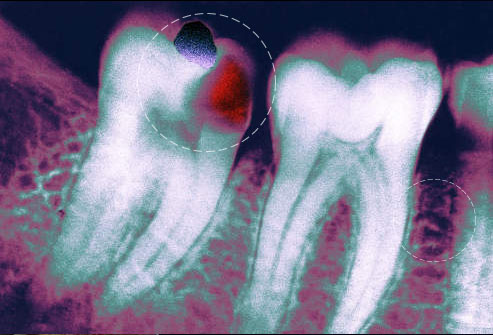 Flossing and brushing daily and regular dental checkups help prevent problems like cavities, abscesses, and tooth discoloration. Don't mess around with a severe toothache. Dental infections can spread to the face, skull, and even to the bloodstream. See your dentist as soon as possible if your tooth aches or if you have a fever, earache, or pain when you open your mouth wide. Bad Breath  Unbrushed teeth have food particles around them that promote bacteria and cause bad breath. Persistent bad breath or a bad taste in your mouth may be from continuous breathing through your mouth, dry mouth, tooth decay, a sign of gum disease, or even diabetes. Fight bad breath by brushing your teeth and tongue, drinking water, and avoiding food triggers. See your dentist if bad breath persists. "Lie" Bumps  According to an old wives' tale, telling a lie causes a bump on the tongue. So-called "lie bumps" or transient lingual papillitis are common even if you tell only the truth. These small, harmless bumps go away on their own after a few days, but they may be uncomfortable. Their cause is a mystery -- it could be a reaction to a food or a minor trauma like biting the tongue. You don't need to treat them, although oral anesthetics may relieve discomfort.
Medical conditions and oral health Dental caries (tooth decay) Gum conditions Symptoms of Gum conditions (Gum disorders) Gum pain Gum swelling Gum mass Gum ulceration Gum bleeding Gum conditions Gingivitis Periodontitis Plaque Tartar Calculus Dental scaling Root planing Oral hygiene Swollen gums Bleeding gums Red gums inflamed gums Cleft lip and palate Oral and facial pain Gum disease What is gum disease? Gum disease is described as swelling, soreness or infection of the tissues supporting the teeth. There are two main forms of gum disease: gingivitis and periodontal disease. What is gingivitis? Gingivitis means ‘inflammation of the gums'. This is when the gums around the teeth become very red and swollen. Often the swollen gums bleed when they are brushed during cleaning. What is periodontal disease? Long-standing gingivitis can turn into periodontal disease. There are a number of types of periodontal disease and they all affect the tissues supporting the teeth. As the disease gets worse the bone anchoring the teeth in the jaw is lost, making the teeth loose. If this is not treated, the teeth may eventually fall out. Am I likely to suffer from gum disease? Probably. Most people suffer from some form of gum disease, and it is a major cause of tooth loss in adults. However, the disease develops very slowly in most people, and it can be slowed down to a rate that should allow you to keep most of your teeth for life. What is the cause of gum disease? All gum disease is caused by plaque. Plaque is a film of bacteria which forms on the surface of the teeth every day. Many of the bacteria in plaque are completely harmless, but there are some that have been shown to be the main cause of gum disease. To prevent and treat gum disease, you need to make sure you remove all the plaque from your teeth every day. This is done by brushing and cleaning in between the teeth with ‘interdental' brushes or floss. See our leaflet ‘Tell me about Caring for my teeth and gums' for how to do this. How will smoking affect my gums and teeth? Smoking can also make gum disease worse. People who smoke are more likely to produce bacterial plaque, which leads to gum disease. The gums are affected because smoking causes a lack of oxygen in the bloodstream, so the infected gums don't heal. Smoking causes people to have more plaque and the gum disease to get worse more quickly than in non-smokers. Gum disease is still a major cause of tooth loss in adults. What happens if gum disease is not treated? Unfortunately, gum disease does not usually cause pain as it gets worse so you do not notice the damage it is doing. However, the bacteria are sometimes more active and this makes your gums sore. This can lead to gum abscesses, and pus may ooze from around the teeth. Over a number of years, the bone supporting the teeth can be lost. If the disease is left untreated for a long time, treatment can be more difficult. How do I know if I have gum disease? The first sign is blood on your toothbrush or in the rinsing water when you clean your teeth. Your gums may also bleed when you are eating, leaving a bad taste in your mouth. Your breath may also become unpleasant. What do I do if I think I have gum disease? The first thing to do is visit your dental team for a thorough check-up of your teeth and gums. They will measure the 'cuff' of gum around each tooth to see if there is any sign that periodontal disease has started. X-rays may also be needed to see the amount of bone that has been lost. This assessment is very important, so the correct treatment can be prescribed for you. What treatments are needed? Your dental team will remove all plaque and tartar from your teeth. You will also be shown how to remove plaque successfully yourself, cleaning all the surfaces of your teeth thoroughly and effectively. This may take a number of sessions with the dental team. A good oral care routine at home with brushing and interdental cleaning is the most important thing you can do to help prevent gum disease getting worse. What else may be needed? Once your teeth are clean, your dental team may need to treat the roots of the teeth to make sure that the last pockets of bacteria are removed. This is called ‘root planing'. You'll probably need the treatment area to be numbed before anything is done. Afterwards, you may feel some discomfort for up to 48 hours. Once I have had periodontal disease, can I get it again? There is no cure for periodontal disease, but it can be controlled as long as you keep up the home care you have been taught. Any further loss of bone will be very slow and it may stop altogether. However, you must make sure you remove plaque every day, and go for regular check-ups by the dental team. I have heard gum disease is linked with other health conditions – is this true? In recent years gum disease has been linked with general health conditions such as diabetes, strokes, cardiovascular disease, poor pregnancy outcomes and even dementia. More research is needed to understand how these links work but there is more and more evidence that having a healthy mouth and gums can help improve your general health and reduce the costs of medical treatment. Teeth Treatments Brushing teeth: Daily brushing of the teeth removes plaque and prevents cavities. Flossing teeth: Using floss or an approved dental gum cleaner cleans teeth below the gum line, where brushing cannot reach. Teeth cleaning: Professional teeth cleaning every six months may help prevent teeth and gum disease. Tooth filling: Drilling out the diseased part of a tooth and packing the space with a mineral filling can prevent a cavity from destroying the tooth. Root canal: The deep pulp of a tooth is drilled out, cleaned, and filled. A root canal is done when damage to the teeth has affected the deep pulp. Tooth extraction: If a tooth is too damaged to repair with a filling or root canal, it may be removed. Wisdom teeth are often extracted to prevent displacement of the other teeth. Braces: An artificial device or system that places teeth under tension for a long period of time. Eventually, braces can help crooked teeth become realigned. Mouth guard: A plastic mouthpiece can provide protection from teeth grinding and injury during sports. Dental sealants: A plastic sealant applied to the teeth can help block bacteria from hiding in crevices on teeth surfaces. Sealants can help prevent cavities. Teeth whitening: Over-the-counter and professional chemical treatments can bleach teeth to a brighter white. Tooth sensitivity is the most common side effect. Toothpaste What is Toothpaste? : Guide to Toothpaste Toothpaste is a gel or paste type of substance which is applied to a toothbrush to clean the teeth. This mainly white substance removes particles of food and plaque from your teeth and prevents bad breath (halitosis) as well. Toothpaste contains a range of ingredients, for example fluoride which helps to protect the teeth against tooth decay and gum disease. Toothpaste is an important part of a daily dental care routine and dentists recommend that people use it twice a day. Ideally, you would brush your teeth after every meal but failing that, twice a day will do. If you visiting this guide with the intention of finding out which is the best toothpaste to buy then you will find it helpful to start by looking at what toothpaste is made from. What is the role of toothpaste manufacturers in enhancing oral health? On May 1, 2015, Colgate toothpaste manufacturer did not know there are four stages of gum disease. What are the stages of gum disease? Gingivitis Early periodontitis Moderate periodontitis Advanced periodontitis You can manufacture quality oral health products if you know everything about human healthcare, including oral health. Here are further facts. What is in your toothpaste? You will find that a great many toothpastes contain the same ingredients but some will have an added emphasis on a particular ingredient. One example is a particular flavouring such as mint. Toothpaste is comprised of several ingredients which include: •A ‘binder’ (holds the ingredients together) such as sodium alginate. •Chalk or baking soda •A foam based compound which helps to remove food debris from the teeth, e.g. sodium lauryl sulphate. •An ingredient called a ‘humectant’ which ensures that the toothpaste is moist. •A flavouring such as mint •Fluoride •Water •Anti-bacterial agent (prevent gum disease) These ingredients are weighed, mixed together in a large vat and passed through a filling machine and into tubes. You may be interested to learn that toothpaste has a long history; one that goes back 4,000 years to be exact! People then used a wide variety of substances to clean their teeth which include sand, ground up fish bones and salt! It wasn’t until the late nineteenth century that toothpaste first appeared in tubes and the mid twentieth century when fluoride was added to toothpaste for the first time. Toothpaste has certainly moved on since then and is available as a gel, paste, with ‘stripes’ etc. Nowadays there is a brand of toothpaste to cater for everyone’s needs. Mouthrinses Mouthrinses are used for a variety of reasons: to freshen breath, to help prevent or control tooth decay, to reduce plaque (a thin film of bacteria that forms on teeth), to prevent or reduce gingivitis (an early stage of gum disease), to reduce the speed that tartar (hardened plaque) forms on the teeth, or to produce a combination of these effects. Most mouthrinses are available without a prescription. What ingredients are commonly found in mouthrinse? Basic ingredients include water, alcohol, cleansing agents, flavoring ingredients and coloring agents. Active ingredients vary depending on the type of mouthrinse, but they can be placed into four general groups: •Antimicrobial agents act directly on oral bacteria to help reduce plaque, decrease the severity of gingivitis and control bad breath. •Fluoride helps reduce tiny lesions (tooth decay) on tooth enamel and make teeth more resistant to decay. •Astringent salts can serve as temporary deodorizers that mask bad breath. •Odor neutralizers act by chemically inactivating odor causing compounds. What’s the difference between cosmetic and therapeutic mouthrinses? Cosmetic mouthrinses may temporarily control or reduce bad breath and leave the mouth with a pleasant taste. But they don’t deal with the causes of bad breath. They don’t kill the bacteria that cause bad breath or chemically inactivate odor causing compounds. Also, none of the cosmetic mouthrinses helps reduce plaque, gingivitis or cavities. Therapeutic mouthrinses, on the other hand, can help reduce plaque, gingivitis, cavities and bad breath. Some fight the bacteria present in plaque, a sticky film that forms on teeth and gums. Plaque bacteria create toxins that can damage the gums. Plaque that is not removed with daily brushing and flossing can cause gingivitis, an early stage of gum disease. If plaque is allowed to continue to accumulate, gingivitis can progress to advanced gum disease, called periodontitis, which only a dentist can treat. Plaque can also turn into tartar (or calculus), a hard substance that can only be removed during a professional cleaning. Some therapeutic mouthwashes contain agents that either fight bad breath bacteria or that chemically inactivate odor causing compounds. Therapeutic mouthrinses that contain fluoride help prevent or reduce tooth decay. Do I need a mouthrinse? Your dentist can advise you whether you need a mouthrinse depending on your oral health needs. Rinsing helps remove debris from the mouth. It can be done before or after brushing, but it is not a substitute for brushing or flossing. You may consider, or your dentist may recommend, using a mouthrinse with fluoride or antimicrobial agents as part of your daily oral hygiene routine. If you have difficulty brushing and flossing, a mouthrinse may provide additional protection against cavities and periodontal (gum) disease. Anti-cavity rinses with fluoride help protect tooth enamel. Dentists may prescribe special rinses for patients who have had periodontal surgery. What is an “anti-gingivitis or anti-plaque” mouth rinse? Anti-plaque, anti-gingivitis, antibacterial, antimicrobial or chemotherapeutic mouthrinses reduce bacterial count and inhibit bacterial activity that can cause gingivitis, a form of periodontal (gum) disease. Can a mouthrinse eliminate bad breath? Therapeutic mouthrinses can help reduce bad breath. However, if you must constantly use a mouthrinse or breath freshener to hide unpleasant mouth odor, it would be a good idea to visit your dentist to see if there is some underlying cause that can be corrected. How does a mouthrinse get the ADA Seal? A company earns the ADA Seal for its product by submitting scientific evidence that the product is safe and effective. The ADA Council on Scientific Affairs carefully evaluates the evidence according to objective guidelines. In the case of a mouthrinse, the Council may use any of the following guidelines, depending on the product’s intended use: •Chemotherapeutic Products for the Control of Gingivitis •Products Used in the Management of Oral Malodor A mouthrinse that claims to control gingivitis must substantiate that claim by demonstrating a statistically significant reduction in gingival inflammation. A mouthrinse that claims to control bad breath must substantiate that claim by showing that it works to reduce odors over a prolonged time frame. A mouthrinse that contains fluoride for reducing decay must either demonstrate effectiveness in clinical studies, or show that the formula is the same as a similar product that has been clinically proven. With any type of mouthrinse, a manufacturer must show that the product is safe and that it does not damage oral tissues or cause any internal problems. Should I brush, floss or rinse first? The sequence in which you brush, floss and rinse makes no difference as long as you do a thorough job and use quality products. Check the mouthrinse manufacturer’s label for recommendations on how and when to use the product, and look for products that have the ADA’s Seal of Acceptance. At what age can a child use a fluoride mouthrinse? The use of fluoride mouthrinses is not recommended for children six and younger because they may swallow the rinse. Always check the manufacturer’s label for precautions and age recommendations and talk to your dentist. Clinical studies indicate that regular use of a fluoride mouthrinse (daily or weekly, depending on the rinse) can provide additional protection against cavities over that provided by a fluoride toothpaste. White patches in the mouth What is a white patch in the mouth? A white patch is an area of thickening in the lining of the mouth (mucosa) and has a white appearance (also called leukoplakia). Why do people get white patches? Your mouth (and tongue) are lined with a special type of skin (mucosa), which looks (mostly) pink because it is thinner than your other skin (eg on your arms and legs). Some changes to your mouth lining can change its color to white: •It is common for people to have a line of white along the inside of their cheeks, this is where their teeth rub against the cheek (and is quite normal). •If you burn your mouth (eg after hot drinks or food) you can get white blisters, which usually peel off soon afterwards. •If you have been ill for a while or haven't moved your tongue around much, you can get a furry white tongue. This is because the skin on the taste buds has not been rubbed off normally. You can usually gently rub/scrape this off with a toothbrush. •Mouth ulcers can be white because of thicker layers of skin cells forming that are trying to heal the injury. •If people have poorly fitting dentures they can get ulcers or sometimes white patches forming. Dentists and doctors are most concerned about the white patches that can't be rubbed or scraped away. These show areas of thicker mouth lining, which can be signs of mouth conditions. Where are white patches found? A white patch can be situated anywhere in the mouth. How big are white patches? A white patch can be of any size. What causes mouth white patches? White patches in the mouth result from infections caused by bacteria, viruses and fungi. Infections of the skin around the mouth, mucous membranes inside the mouth, gums, and tongue are common causes of mouth white patches. White patches are almost always due to some form of irritation including infection: Alcohol use (long-term use) Bacterial infections Behcet’s syndrome (disease characterized by widespread inflammation of blood vessels) Candidiasis (fungal infection) Canker sores Celiac disease (severe sensitivity to gluten from wheat and other grains that causes intestinal damage) Chemical irritation: eg aspirin burns, smoking (smoker's keratosis); Chewing on the inside of cheeks Crohn’s disease (inflammatory bowel disease that can affect any part of the intestine) Dental appliances Herpes simplex virus Human Papilloma Virus infections Immune system diseases, such as systemic lupus erythematosus (disorder in which the body attacks its own healthy cells and tissues) Infection: eg fungal (candida) Keratosis pharyngis Koplik's spots Leukoplakia (precancerous condition of the mouth) Lichen planus Measles Oral candidiasis Salivary duct stone Trauma and friction: eg poorly fitting dentures, cheek biting, sharp teeth or fillings (frictional keratosis) Tonsillitis Tobacco use (chewing or smoking) Ulcerative colitis Questions for diagnosing the cause of mouth white patches To diagnose your condition, your doctor or licensed health care practitioner will ask you several questions related to your mouth white patches including: How long have you had the mouth white patches? Why: to determine if acute or chronic. Where exactly are the mouth white patches? Why: e.g. lips, gums, tongue, lining of the mouth, tonsils. Medications What medications has the patient been taking for the past week? What medication is the patient taking every day in recent months? Why: some medications increase the risk of oral Candida infection including steroids (including inhaled steroids), broad spectrum antibiotics and tumor chemotherapy; some medications may induce a lichen planus like eruption including ACE inhibitors, gold, streptomycin, tetracycline, quinine, penicillamine, hydrochlorothiazide and chlorpropamide. Does the patient have a fever? Pain Do You Have Pain? Where is the Pain? Is there more than one site? When did your pain start? How often does it occur? Has its intensity changed? How long does it last? What makes your pain worse? What makes your pain better? What previous treatment have you tried to relieve your pain? Were they effective? What does your pain feel like? What words would you use to describe your pain? Does the pain move anywhere? On a scale of 0 to 10 with O being no pain and 10 being the worst pain you can imagine, how much does it hurt right now? How much does it hurt at it’s worst? How much does it hurt at it’s best? If your medicine helps with the pain, how many hours of relief do you get? Is this acute or chronic pain? Pain Evaluation and Treatment Here are further guidelines. http://www.qureshiuniversity.com/pain.html Do you have dentures? Why: Poorly fitting dentures may cause white, raised folds of tissue in the mouth. Symptoms of lichen planus? Why: e.g. raised flat topped purple colored shiny itchy patches on the skin and milky white raised patches in the mouth. Mouth lesions may be painful if ulcers are present. Mouth lesions may occur on the lining of the mouth, lips, tongue or gums. Symptoms of measles? Why: e.g. fever, malaise, red watery eyes, runny nose, blotchy bright red rash, cough, Koplik's spots ( bluish white spots on a red base opposite the premolars inside the mouth). Symptoms of tonsillitis? Why: e.g. fever, sore throat, difficulty with swallowing due to pain, malaise, white pus spots on tonsils, enlarged neck lymph nodes. Symptoms of Chronic mucocutaneous candidiasis? Why: a distinct syndrome usually occurring in children comprising of recurrent or persistent oral thrush, finger or toe bed infection and skin infection. Symptoms of diabetes Why: e.g. frequent urination, excessive thirst, weight loss, fatigue - can cause recurrent mouth infections especially Candida (thrush). Symptoms of oral candidiasis? Why: e.g. creamy white curd-like patches in the mouth which are removed only with difficulty and leave a bleeding surface. If the infection spreads to the esophagus it may cause pain with swallowing. Sexual history Are you currently receiving care for other health problems? Do you smoke or use smokeless tobacco products? When did you first notice the white patches in your mouth? Have you recently been on antibiotic therapy? Do you have any other symptoms? What medications are you taking? How are white patches diagnosed? Often an experienced dentist or doctor can tell what kind of white patch you have by its appearance, position and by asking you questions about how long you have had it etc. Sometimes they will wish to take a biopsy of a white patch to make sure it is not something that requires more involved treatment. What will a biopsy involve? A biopsy is a sample of mouth tissue (eg lip, cheek, gum, tongue) that enables us to look at it under a microscope. We will use local anaesthetic to numb the area and sew it up afterwards using dissolvable stitches (sutures). The biopsy area might be a little sore for a couple of days afterwards and you should rinse your mouth with warm salted water for a week to keep the area clean. What can be done to help white patches heal? As described above, there are many causes of white patches. Your dentist (or doctor) might offer you the following advice: •Stop (or greatly reduce) smoking (smoker's keratosis); Or will offer you the following treatment to help it heal up (or prevent it forming): •Smoothing sharp edges on teeth (frictional keratosis); •Remaking or relining dentures; •Eradicating infection (such as fungal infections: candida); I have a sore white patch, what can I do to make it more comfortable? Occasionally, white patches can become sore. If this is the case, it is important to avoid anything that might make it worse, such as spicy or abrasive foods and alcohol. If it remains a problem, your dentist or doctor can prescribe special mouthwashes or ointments. Should I be worried about white patches? Most white patches are a reaction to an irritation and are not a cause for concern. Very rarely, they can be an early sign of more serious mouth conditions (including mouth cancer). This is why it is important to seek advice from an experienced professional (your dentist or doctor) so they can help you remove possible reasons for them forming and follow up on any unusual ones. I have a white patch that is being 'watched', how often will I need to return and what should I do between appointments? Some people have white patches that we have some concerns about and are not sure if they will repair on their own (or after we have removed some of the possible causes of irritation). We will explain that we are 'watching' the patch and would like you to return for a follow-up appointment (usually after 3-12 months). It is important that you attend these appointments so we can check that the white patch has not changed. Do heed any advice you are given about stopping smoking, and reducing a heavy alcohol intake, or cleaning the area. Do keep an eye on the patch yourself and if you think that it has changed, or if it becomes painful or forms an ulcer or lump, please ring the dentist or doctor who is caring for you. Explain to them what you have noticed and they might decide to bring your appointment forwards. It is better that they take a look at it to stop you worrying about it. What is leukoplakia? Leukoplakia just means white patch in Greek. It is a term used for white patches that do not fit into any of the above categories, most of which have causes that can be avoided or treated. If we are not sure of the cause and type of white patch we will often want to find out what is happening in the mouth or skin by taking a biopsy. Depending on the biopsy result, we might recommend that the white patch is completely removed or carefully watched by an experienced professional to make sure that it doesn't develop into anything more serious. These options will be discussed with you carefully. . What Is the Treatment for Leukoplakia? Treatment for leukoplakia, if needed, involves removing the source of irritation. For example, if leukoplakia is caused by a rough tooth or an irregular surface on a denture or a filling, the tooth will be smoothed and dental appliances repaired. If leukoplakia is caused by smoking, you will be asked to minimize or stop smoking or using other tobacco products. Leukoplakia is usually harmless, and lesions usually clear in a few weeks or months after the source of irritation is removed. If eliminating the source of irritation is ineffective in reducing leukoplakia, the lesion may need to be surgically removed. The lesion can be removed either by your general dentist or by an oral surgeon. Hairy leukoplakia requires treatment with an antiviral medication. Here are further guidelines. http://www.qureshiuniversity.com/Whitepatchesinthemouth.html GENERAL DENTISTRY General Dentistry Dental Hygiene Perio Protect Dental Floss Toothpaste Mouthwash COSMETIC DENTISTRY Smile Makeover Teeth Whitening Dental Veneers Dental Crowns Dental Bridges Dental Restorations Dental Implants Cerec dentistry Cosmetic Bonding Tooth Reshaping Full Mouth Reconstruction Cost of Cosmetic Dentistry COSMETIC ORTHODONTICS Orthodontics Teeth Straightening Invisalign Inman Aligner 6 month smiles Damon Braces Lingual braces Here are further guidelines. Here are further guidelines. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Digestive system diagram Human Anatomy Digestive System 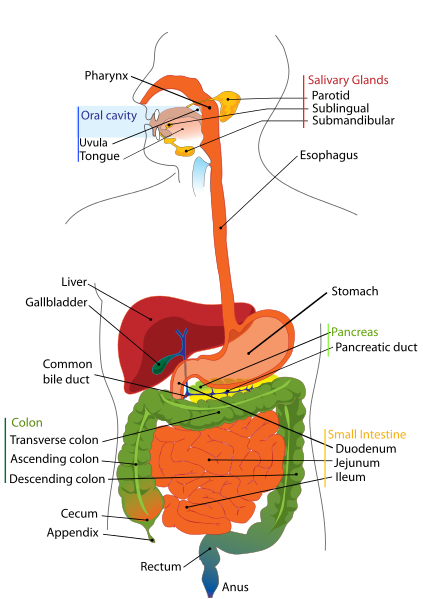 Mouth Esophagus Stomach Small intestine Pancreas Liver Gallbladder Colon (large intestine) Rectum Anus
Digestive System 1. Which organs of the body are part of the human digestive system? The digestive system, also known as “systema digestorium”, or gastrointestinal system, is composed of the digestive tube organs plus the digestive adnexal glands. The digestive tube is composed of mouth, pharynx, esophagus, stomach, small intestine (duodenum, jejunum, ileum), large intestine (caecum, colon, rectum) and anus. 2. Which are the three parts of the small intestine? The small intestine is divided into three portions: duodenum, jejunum and ileum. 3. How is extracellular digestion related to cellular and tissue specialization? A variety of specialized cells and tissues appeared with extracellular digestion to provide enzymes and special structures for the breaking down of dietary macromolecules. This phenomenon allowed other cells to be liberated for other tasks and differentiations while benefiting from nutrients distributed through the circulation. 4. What is the difference between a complete digestive system and an incomplete digestive system? How are these types of digestive tubes associated or not to extracellular digestion? Animals with an incomplete digestive system are those in which the digestive tube has only one opening (cnidarians, platyhelminthes). Animals with a complete digestive system are those in which the digestive tube has two openings, mouth and anus (all other animal phyla, with the exception of poriferans, that do not have any digestive tube). In animals with incomplete digestive tubes the digestion is mixed, it begins in the extracellular space and finishes in the intracellular space. In animals with complete digestive systems extracellular digestion within the digestive tube predominates. 5. What are some evolutionary advantages of animals with complete digestive tube? The complete digestive tube allows animals to continuously feed themselves without waiting for residuals to be eliminated before beginning the digestion of new foods. In this way the absorption of larger amount of nutrients is possible and therefore bigger and more complex species can develop. Digestive tubes with two openings also make digestion more efficient since they provide different sites with different physical and chemical conditions (mouth, stomach, bowels) for the action of different complementary digestive enzymatic systems. 6. What is mechanical digestion? In molluscs, arthropods, earthworms, birds and vertebrates, in general, which organs respectively participate in this type of digestion? Mechanical digestion is the fragmentation of food aided by specialized physical structures, such as teeth, previous to extracellullar digestion. The mechanical fragmentation of food helps digestive enzymatic reactions because it provides a larger total area for the contact between enzymes and their substrates. In some molluscs, the mechanical fragmentation is done by the radula (a teeth-like structure). Some arthropods, like lobsters and dragonflies, have mouthparts that make mechanical digestion of food. In earthworms and birds, the mechanical digestion is made by an internal muscular organ. In mandibulate vertebrates there are mandibles and chewing muscles to triturate food previous to the chemical digestion. 7. Concerning extracellular digestion what is meant by chemical digestion? Chemical digestion is the series of enzymatic reactions to break macromolecules into smaller ones. 8. Which type of chemical reaction is the breaking of macromolecules into smaller ones that occurs in digestion? What are the enzymes that participate in this process called? The reactions of the extracellular digestion are hydrolysis reactions, i.e., breaking of molecules with the help of water. The enzymes that participate in digestion are hydrolytic enzymes. 9. What is digestion? Digestion is the breaking down of larger organic molecules obtained from the diet, e.g. carbohydrates, fats, proteins, into smaller ones, like glucose, fatty acids, glycerol and amino acids. 10. What are peristaltic movements? What is their role in human digestion? Peristalsis is the process of synchronized contractions of the muscular wall of the digestive tube. Peristaltic movements may occur from the esophagus until and including the bowels. The peristaltic movements are involuntary and they have the function of moving and mixing food along the digestive tube. Peristaltic movement deficiency, for example, in case of injuries of the innervation of the muscular wall of the digestive tube caused by Chagas’ disease, can lead to the interruption of the food traffic inside the bowels and to severe clinical consequences like megacolon (abnormal enlargement of the colon) and megaesophagus (enlargement of the esophagus). 11. From the lumen to the external surface what are the tissues that form the digestive tube wall? From the internal surface to the external surface, the digestive tube wall is made of mucosa (epithelial tissue responsible for the intestinal absorption), submucosa (connective tissue beneath the mucous membrane and where blood and lymphatic vessels and neural fibers are located), muscle layers (smooth muscle tissue, two layers, one interior circular and other exterior longitudinal, structures responsible for the peristaltic movement), serous membrane (associated epithelial and connective tissue forming the external surface of the organ). In the bowels the serous membrane prolongs to form the mesentery, a serosa that encloses blood vessels and supports the bowels within the abdominal cavity. 12. What is the location of the salivary glands in humans? There are 6 major salivary glands and they are located one in each parotid gland, two beneath the mandibles (submandibular) and two in the base of the tongue (sublingual). More than 700 other minor salivary glands exist dispersed on the lip mucosa, gingiva, palate and pharynx. 13. What is the approximate pH of the salivary secretion? Is it an acid or basic fluid? What are the main functions of saliva? The saliva pH is approximately 6.8. It is thus a slightly acid pH. Saliva lubricates the food bolus and initiates the enzymatic extracellular digestion of food. It also works as a buffer for the mouth pH and it has an important role of having IgA antibodies (also present in tears, colostrum, mother’s milk and in the mucosae of the intestine and airways) that protect the organism against pathogens. 14. What is the salivary digestive enzyme? Which type of food does it digest and into which smaller molecules does it transform the food? The salivary hydrolase is known as salivary amylase, or ptyalin. Ptyalin digests carbohydrates breaking starch and glycogen, glucose polymers, into maltose (a glucose disaccharide) and dextrin. 15. Why doesn't the food enter the trachea instead of going to the esophagus? When food is swallowed the swallow reflex is activated and the larynx elevates and closes to avoid portions of the food bolus entering the trachea causing aspiration of strange material to the bronchi. 16. Is the esophagus a muscular organ? Why even in a patient lying totally flat on a hospital bed can the swallowed food reach the stomach? The esophagus is a predominantly muscular organ so the assertion is correct. The esophagus is a muscular tube formed in its superior third of striated muscle tissue, in its middle third of mixed muscle tissue (striated and smooth) and in its lower third of smooth muscle tissue. The peristalsis of the esophagus provides the movement of the food towards the stomach even without gravitational help. 17. What is the route of the ingested food from swallowing until the duodenum? Until reaching the duodenum the food enters the mouth, passes the pharynx, goes down the esophagus and passes the stomach. 18. what is the valve that separates the stomach from the esophagus called? What is its function? The valve that separates the stomach from the esophagus is the cardia. It has the function of preventing acid gastric content from entering back into the esophagus. Insufficiency of this valve causes gastroesophageal reflux, a disease in which patients complain of bloating and heartburn (retrosternal burning). 19. What is the valve that separates the duodenum from the stomach called? What is its function? The valve that separates the stomach from the duodenum is the pylorus. It has the function of keeping the food bolus within the gastric cavity for enough time to allow the gastric digestion to take place. It also has the function of preventing the intestinal content from going back into the stomach. 20. What is the pH inside the stomach? Why is there a need to keep that pH level? How is it maintained? Which are the cells that produce that pH? The normal pH of the gastric juice is around 2. So it is an acid pH. It is necessary for the gastric pH to be kept acid for the activation of pepsinogen (a proenzyme secreted by the gastric chief cells) into pepsin, the digestive enzyme that acts only under low pH. This pH level is attained by the secretion of hydrochloric acid (HCl) by the parietal cells. 21. Besides being fundamental for the activation of the main gastric digestive enzyme how does HCl also directly participate in digestion? With its corrosive effect, HCl also helps the rupture of the adhesion between food particles, facilitating the digestive process. 22. How is the gastric mucosa protected from the acid pH of the stomach? The gastric epithelium is mucus secretory, i.e., it produces mucus. The mucus covers the stomach wall preventing corrosion by the gastric juice. 23. What is the digestive enzyme that acts within the stomach? Which type of food does it digest? What are the cells that produce that enzyme? The digestive enzyme that acts in the stomach is pepsin. Pepsin has the function of breaking proteins into smaller peptides. The gastric cells that produce pepsinogen (the zymogen precursor of pepsin) are the chief cells. 24. What name does the food bolus that passes from the stomach to the duodenum get? The partially digested and semifluid food bolus that leaves the stomach and enters the duodenum is called chyme. 25. How different are intracellular and extracellular digestion? What is the evolutionary advantage of extracellular digestion? Intracellular digestion is that in which the breaking down of macromolecules takes place within the cell. Extracellular digestion is that in which macromolecules are broken down in places outside the cell (in the extracellular space, in the surrounds, in the lumen of digestive tubes, etc.) The advent of extracellular digestion in evolution allowed organisms to benefit from a greater variety of food. The breaking down of larger molecules into smaller ones outside the cell permitted the use of other foods than those that, due the size of their molecules, could not be interiorized by diffusion, phagocytosis or pinocytosis. 26. By generally dividing food into carbohydrates, fats and proteins and considering the digestive process until the pylorus (exit of stomach), which of these mentioned types of food have already undergone chemical digestion? Until the exit of the stomach, carbohydrates, in the mouth, and proteins, in the stomach, have already undergone chemical breaking by digestive enzymes. Carbohydrates have suffered action of the salivary amylase (ptyalin) and proteins have suffered action of the enzyme pepsin of the gastric juice. Fats, until reaching the duodenum, do not undergo chemical digestion. 27. What is the substance produced in the liver that acts in the small intestine during digestion? How does that substance act in the digestive process? Bile, an emulsifier liquid, is made by the liver and later stored within the gallbladder and released in the duodenum. Bile is composed of bile salts, cholesterol and bile pigments. Bile salts are detergents, amphiphilic molecules, i.e., molecules with a polar water-soluble portion and a non-polar fat-soluble portion. This feature allows bile salts to enclose fats inside water-soluble micelles in a process called emulsification for them to be in contact with intestinal lipases, enzymes that break fats into simpler fatty acids and glycerol. 28. What is the adnexal organ of the digestive system in which bile is stored? How does this organ react to the ingestion of fat rich food? Bile is concentrated and stored in the gallbladder. When fat rich foods are ingested the gallbladder contracts to release bile inside the duodenum. (This is the reason why patients with gallstones must not ingest fatty food, the reactive contraction of the gallbladder may move some of the stones to the point of blocking the duct that drains bile into the duodenum, causing pain and possible severe complications.) 29. What are the digestive functions of the liver? Besides making bile for release in the duodenum, the liver has other digestive functions. The venous network that absorbs nutrients from the guts, called mesenteric circulation, drains its blood content almost entirely to the hepatic portal vein. This vein irrigates the liver with absorbed material from the digestion. So the liver has the functions of storing, processing and inactivating nutrients. Glucose is polymerized into glycogen in the liver; this organ also stores many vitamins and the iron absorbed in the intestine. Some important metabolic molecules, like albumin and clotting factors, are made in the liver from amino acids of the diet. In the liver ingested toxic substances, like alcohol and drugs, are inactivated too. 30. Besides the liver which is the other adnexal gland of the digestive system that releases substances in the duodenum participating in extracellular digestion? The other adnexal gland of the digestive system is the pancreas. This organ makes digestive enzymes that digest proteins (proteases), lipids (lipases) and carbohydrates (pancreatic amylases). Other digestive enzymes, like gelatinase, elastase, carboxipeptidase, ribonuclease and deoxyribonuclease are also secreted by the pancreas. 31. How does the pancreatic juice participate in the digestion of proteins? What are the involved enzymes? The pancreas secretes trypsinogen that, undergoing action of the enzyme enterokinase secreted by the duodenum, is transformed into trypsin. Trypsin in its turn catalyzes the activation of pancreatic chymotrypsinogen into chymotrypsin. Trypsin and chymotrypsin are proteases that break proteins into smaller peptides. The smaller peptides are then broken into amino acids by the enzyme carboxipeptidase (also secreted by the pancreas in a zymogen form and activated by trypsin) helped by the enzyme aminopeptidase made in the intestinal mucous membrane. 32. How does the pancreatic juice resume the digestion of carbohydrates? What is the involved enzyme? Carbohydrate digestion begins with the action of the salivary amylase (ptyalin) in the mouth and it continues in the duodenum by the action of the pancreatic juice. This juice contains the enzyme pancreatic amylase, or amylopsin, that breaks starch (amylum) into maltose (a disaccharide made of two glucose molecules). 33. How does the pancreatic juice help the digestion of lipids? What is the involved enzyme? The enzyme pancreatic lipase is present in the pancreatic juice. This enzyme breaks triacylglycerol (triglyceride) into fatty acids and glycerol. 34. Besides the pancreatic juice in the intestine there is the releasing of the enteric juice that contains digestive enzymes too. What are these enzymes and which type of molecule do each of these enzymes break? The enteric juice is secreted by the small intestine mucosa. The enzymes of the enteric juice and their respective functions are described as follows: Enterokinase: enzyme that activates trypsinogen into trypsin. Saccharase: enzyme that breaks sucrose (saccharose) into glucose and fructose. Maltase: enzyme that breaks maltose into two glucose molecules. Lactase: enzyme that breaks lactose into glucose and galactose. Peptidases: enzymes that break oligopeptides into amino acids. Nucleotidases: Enzymes that break nucleotides into its components (nitrogen-containing bases, phosphates and pentoses). 35. Coming from the acid pH of the stomach which pH level does the chyme find when it enters the duodenum? Why is it necessary to maintain that pH level in the small intestine? What are the organs responsible for that pH level and how is it kept? Entering the duodenum the chyme meets the pancreatic juice under a pH of approximately 8.5. The neutralization of the chyme acidity is necessary to keep adequate pH level for the functioning of the digestive enzymes that act in the duodenum. Without the neutralization of the chyme acidity the mucous membrane of the intestine would be injured. When stimulated by the chyme acidity the duodenum makes a hormone called secretin. Secretin stimulates the pancreas to release the pancreatic juice and also the gallbladder to expel bile in the duodenum. The pancreatic secretion, rich in bicarbonate ions, is released in the duodenum and neutralizes the chyme acidity; this acidity is also neutralized by the secretion of bile in the duodenal lumen. 36. What are the five human digestive secretions? Which of them is the only one that does not contain digestive enzymes? The human digestive secretions are: saliva, gastric juice, bile, pancreatic juice and enteric juice. Among these secretions only the bile does not contain digestive enzymes. 37. Why do protease-supplying cells of the stomach and of the pancreas make only precursors of the active proteolytic enzymes? The stomach and the pancreas make zymogens of the proteases pepsin, chymotrypsin and trypsin and these zymogens are released into the gastric or duodenal lumen for activation. This happens to prevent the digestion of these organs' (stomach and pancreas) own cells and tissues by the active form of the enzymes. So the production of zymogens is a protective strategy against the natural effects of the proteolytic enzymes. 38. After digestion the next step is absorption done by cells of the mucous membrane of the intestine. For this task a large absorption surface is an advantage. How is it possible in the small internal space of the body of a pluricellular organism to present a large intestinal surface? Evolution tried to solve this problem in two ways. The simplest is the long and tubular shape of the bowels (approximately eight meters in extension), making possible that numerous small intestine loops fold closely. More efficient solutions are the intestinal villi and the microvilli of the mucosal membrane cells. The intestinal wall is not smooth. The mucous membrane, together with its submucosa, projects inside the gut lumen like glove fingers forming invaginations and villi that multiply the available surface for absorption. In addition the epithelial cells that cover these villi have themselves numerous hairlike projections called microvilli on the external face (lumen face) of their plasma membrane. The absorptive area of the intestines is thus increased hundreds of times with these solutions. In the jejunum and ileum there are folds that have the function of increasing the absorption surface too. 39. In which part of the digestive tube is water is chiefly absorbed? What about the mineral ions and vitamins? Most part of water, vitamins and mineral ions are absorbed by the small intestine. The large intestine, however, is responsible for the reabsorption of nearly 10% of the ingested water, an important amount that gives consistency to feces (colon diseases can cause diarrhea). 40. From the intestinal lumen through to the tissues - what is the route of nutrients after digestion? Monosaccharides, amino acids, mineral salts and water are absorbed by the intestinal epithelium and collected by capillary vessels of the intestinal villi. From the capillaries, nutrients go to the mesenteric circulation, a system of vessels that drains the intestinal loops. The blood of the mesenteric circulation is drained to the portal hepatic vein and some nutrients are processed by the liver. From the liver, nutrients are gathered by the hepatic veins that discharge its blood content into the inferior vena cava. Blood from the inferior vena cava then gains the right chambers of the heart and is pumped to the lungs for oxygenation. From the lungs the blood then returns to the heart where it is pumped to the tissues distributing nutrients and oxygen. 41. What is the special route that lipids follow during digestion? What are chylomicrons? Triglycerides emulsified by the bile within micelles suffer the action of lipases that break them into fatty acids and glycerol. Fatty acids, glycerol and cholesterol are absorbed by the intestinal mucosa. In the interior of the mucosal cells fatty acids and glycerol form again triglycerides that together with cholesterol and phospholipids are packed in small vesicles covered by proteins and called chylomicrons. The chylomicrons are released in minuscule lymphatic vessels not in blood vessels and they gain the lymphatic circulation. So the lymphatic system plays an important role in the absorption of lipids. The lymphatic circulation drains its content to the venous blood circulation. In that manner chylomicrons reach the liver where their lipid content is processed and released in the blood under the form of protein-containing complexes called lipoproteins, like HDL, VLDL and LDL. 42. What are the so-called “good” and “bad” cholesterol? Lipoproteins are complexes made of lipids (triglycerides and cholesterol) and proteins. The lipoproteins present different densities according to the relationship between their protein and lipid quantities since lipids are less dense than proteins. Low-density lipoproteins (LDL) are those with a low protein/lipid relation; high-density lipoproteins (HDL) have a high protein/lipid relation; another group is the very low-density lipoproteins (VLDL) with very low protein/lipid relation. LDL is known as “bad cholesterol” because it transports cholesterol from the liver to the tissues and so induces the formation of atheroma plaques inside blood vessels, a condition called atherosclerosis (do not confuse with arteriosclerosis) that can lead to severe circulatory obstructions like acute myocardial infarction, cerebrovascular accidents and thrombosis. HDL is known as “good cholesterol” since it transports cholesterol from the tissues to the liver (to be eliminated with the bile) and elevation of the HDL blood level reduces the risk of atherosclerosis. (VLDL transforms into LDL after losing triglycerides in the blood). 43. Why does the ingestion of vegetable fibers improve the bowel habit in people that suffer from hard stools? Some types of plant fibers are not absorbed by the intestine but play an important role in the functioning of the organ. They retain water inside the bowels and thus contribute to the softening of the fecal bolus. A softer fecal bolus is easier to be eliminated during defecation. People that eat less dietary fiber may suffer from hard stools and constipation. 44. What are the main functions of the bacterial flora within the human gut? Bacteria that live inside the gut have great importance in digestion. Some polysaccharides like cellulose, hemicellulose and pectin are not digested by the digestive enzymes secreted by the body, instead, they are broken by enzymes released by bacteria of the gastrointestinal tract. The intestinal bacterial flora also make vital substances for the functioning of the bowels facilitating or blocking the absorption of nutrients and stimulating or reducing peristalsis. Some gut bacteria are the main source of vitamin K for the body and so they are essential for the blood clotting process. In the intestinal flora there are utile but also potentially harmful bacteria. It is estimated that more than 100 trillion bacteria live in a human gut. Some bacteria are useful too because they compete with other species preventing excessive proliferation of these bacteria. 45. The releasing of digestive secretions is controlled by hormones. What are the hormones that participate in this regulation? The hormones that participate in the regulation of digestion are gastrin, secretin, cholecystokin and enterogastrone. 46. How is it produced and what is the function of gastrin in the digestive process? The presence of food in the stomach stimulates the secretion of gastrin that in its turn triggers the releasing of the gastric juice. 47. Where is it produced and what is the function of secretin in the digestive process? Secretin is made in the duodenum. The chyme acidity causes the duodenum to release this hormone that in its turn stimulates the secretion of the pancreatic juice. 48. How is it produced and what is the function of cholecystokin in the digestive process? The fat level of the chyme detected in the duodenum stimulates the secretion of cholecystokin (CCK). CCK acts by stimulating the secretion of the pancreatic juice also, and the releasing of bile by the gallbladder. 49. Where is it produced and what is the function of enterogastrone in the digestive process? When the chyme is too fatty there is a secretion of enterogastrone by the duodenum. This hormone reduces the peristalsis of the stomach thus slowing the entrance of food into the duodenum (as the digestion of fats takes more time). 50. What are the special structures of the avian digestive tube and their respective functions? The digestive tube of birds has special structures, in this sequential order: the crop, the proventriculus and the gizzard. The crop has the function of temporary storage of ingested food and it is a more dilated area of the avian esophagus. The proventriculus is the chemical stomach of the birds where food is mixed with digestive enzymes. The gizzard is a muscular pouch that serves as a mechanical stomach where the food is ground to increase the exposure area of the food particles for the digestive enzymes to act. 51. Compared to mammals do birds absorb more or less water in their digestive system? Why is this phenomenon an adaptation to flight? Bird feces are more liquid than mammal feces, i.e., less water is absorbed in the avian digestive system. The more frequent elimination of feces in birds due to their less solid feces is an adaptation to flight since their body weight is kept lower. 52. What is meant by “mutualist exploration of cellulose digestion”, a phenomenon that occurs in some mammals and insects? Herbivorous animals eat great amounts of cellulose, a substance not digested by their digestive enzymes. In these animals regions of the digestive tube are colonized by microorganisms that digest cellulose. This mutualist ecological interaction between animals and microorganisms occurs, e.g., in horses, cows, rabbits and in some insects such as termites. 53. Cows swallow their food once and then this food goes back to the mouth to be chewed again. How can this phenomenon be explained? The food ingested by cows and other ruminant animals passes first within two compartments of the digestive tube called the rumen and the reticulum. Within them the food suffers the action of digestive enzymes released by microorganisms that live there in mutualist ecological interaction. In the reticulum the food is divided in some food bolus too. After passing the reticulum the food (cud) is regurgitated to the mouth to be again chewed and swallowed in a process called rumination. The digesting food then enters the omasum where it is mechanically mixed. After that the food goes to the abomasum, the organ where the chemical digestion takes place. After leaving the abomasum (the true stomach) the food bolus gains the intestine. Mouth The mouth is the beginning of the digestive tract; and, in fact, digestion starts here when taking the first bite of food. Chewing breaks the food into pieces that are more easily digested, while saliva mixes with food to begin the process of breaking it down into a form your body can absorb and use. Esophagus Located in your throat near your trachea (windpipe), the esophagus receives food from your mouth when you swallow. By means of a series of muscular contractions called peristalsis, the esophagus delivers food to your stomach. Stomach The stomach is a hollow organ, or "container," that holds food while it is being mixed with enzymes that continue the process of breaking down food into a usable form. Cells in the lining of the stomach secrete a strong acid and powerful enzymes that are responsible for the breakdown process. When the contents of the stomach are sufficiently processed, they are released into the small intestine. Small intestine Made up of three segments — the duodenum, jejunum, and ileum — the small intestine is a 22-foot long muscular tube that breaks down food using enzymes released by the pancreas and bile from the liver. Peristalsis also is at work in this organ, moving food through and mixing it with digestive secretions from the pancreas and liver. The duodenum is largely responsible for the continuous breaking-down process, with the jejunum and ileum mainly responsible for absorption of nutrients into the bloodstream. Contents of the small intestine start out semi-solid, and end in a liquid form after passing through the organ. Water, bile, enzymes, and mucous contribute to the change in consistency. Once the nutrients have been absorbed and the leftover-food residue liquid has passed through the small intestine, it then moves on to the large intestine, or colon. Pancreas The pancreas secretes digestive enzymes into the duodenum, the first segment of the small intestine. These enzymes break down protein, fats, and carbohydrates. The pancreas also makes insulin, secreting it directly into the bloodstream. Insulin is the chief hormone for metabolizing sugar. Liver The liver has multiple functions, but its main function within the digestive system is to process the nutrients absorbed from the small intestine. Bile from the liver secreted into the small intestine also plays an important role in digesting fat. In addition, the liver is the body’s chemical "factory." It takes the raw materials absorbed by the intestine and makes all the various chemicals the body needs to function. The liver also detoxifies potentially harmful chemicals. It breaks down and secretes many drugs. Gallbladder The gallbladder stores and concentrates bile, and then releases it into the duodenum to help absorb and digest fats. Colon (large intestine) The colon is a 6-foot long muscular tube that connects the small intestine to the rectum. The large intestine is made up of the cecum, the ascending (right) colon, the transverse (across) colon, the descending (left) colon, and the sigmoid colon, which connects to the rectum. The appendix is a small tube attached to the cecum. The large intestine is a highly specialized organ that is responsible for processing waste so that emptying the bowels is easy and convenient. Stool, or waste left over from the digestive process, is passed through the colon by means of peristalsis, first in a liquid state and ultimately in a solid form. As stool passes through the colon, water is removed. Stool is stored in the sigmoid (S-shaped) colon until a "mass movement" empties it into the rectum once or twice a day. It normally takes about 36 hours for stool to get through the colon. The stool itself is mostly food debris and bacteria. These bacteria perform several useful functions, such as synthesizing various vitamins, processing waste products and food particles, and protecting against harmful bacteria. When the descending colon becomes full of stool, or feces, it empties its contents into the rectum to begin the process of elimination. Rectum The rectum (Latin for "straight") is an 8-inch chamber that connects the colon to the anus. It is the rectum's job to receive stool from the colon, to let the person know that there is stool to be evacuated, and to hold the stool until evacuation happens. When anything (gas or stool) comes into the rectum, sensors send a message to the brain. The brain then decides if the rectal contents can be released or not. If they can, the sphincters relax and the rectum contracts, disposing its contents. If the contents cannot be disposed, the sphincter contracts and the rectum accommodates so that the sensation temporarily goes away. Anus The anus is the last part of the digestive tract. It is a 2-inch long canal consisting of the pelvic floor muscles and the two anal sphincters (internal and external). The lining of the upper anus is specialized to detect rectal contents. It lets you know whether the contents are liquid, gas, or solid. The anus is surrounded by sphincter muscles that are important in allowing control of stool. The pelvic floor muscle creates an angle between the rectum and the anus that stops stool from coming out when it is not supposed to. The internal sphincter is always tight, except when stool enters the rectum. It keeps us continent when we are asleep or otherwise unaware of the presence of stool. When we get an urge to go to the bathroom, we rely on our external sphincter to hold the stool until reaching a toilet, where it then relaxes to release the contents. Gastroenterology |
Emergency medicine specialist training programs and relevance to primary care physician.
|
Why should primary care physicians know about emergency medicine specialist training programs?
Medical emergency room can report to you that because of the negligence of a primary care physician, a resident has to face a preventable medical emergency. You may occasionally have to work as emergency medical specialist depending on the needs of the healthcare system in the state. Here are further guidelines. http://www.qureshiuniversity.com/emergencymedicalservices.html |
|
What is primary health care? A health care resource advertises capabilities of screening hypertension and diabetes. That is not primary health care. That is quackery. Such activities are planned on April 20, 2012, at Near North Center, Chicago, Illinois. Heartland Alliance Chicago, Illinois, also is involved in similar quackery. Asian Human Services has declared an annual health fair on April 25, 2012, in Chicago, Illinois, to screen specific medical conditions. Primary Care In defining primary care, it is necessary to describe the nature of services provided to patients, as well as to identify who are the primary care providers. The domain of primary care includes the primary care physician, other physicians who include some primary care services in their practices, and some non-physician providers. However, central to the concept of primary care is the patient. Therefore, such definitions are incomplete without including a description of the primary care practice. The following five definitions relating to primary care should be taken together. They describe the care provided to the patient, the system of providing such care, the types of physicians whose role in the system is to provide primary care, and the role of other physicians, and non-physicians, in providing such care. Taken together they form a framework within which patients will have access to efficient and effective primary care services of the highest quality. Definition #1 - Primary Care Primary care is that care provided by physicians specifically trained for and skilled in comprehensive first contact and continuing care for persons with any undiagnosed sign, symptom, or health concern (the "undifferentiated" patient) not limited by problem origin (biological, behavioral, or social), organ system, or diagnosis. Primary care includes health promotion, disease prevention, health maintenance, counseling, patient education, diagnosis and treatment of acute and chronic illnesses in a variety of health care settings (e.g., office, inpatient, critical care, long-term care, home care, day care, etc.). Primary care is performed and managed by a personal physician often collaborating with other health professionals, and utilizing consultation or referral as appropriate.Primary care provides patient advocacy in the health care system to accomplish cost-effective care by coordination of health care services. Primary care promotes effective communication with patients and encourages the role of the patient as a partner in health care. Definition #2 - Primary Care Practice A primary care practice serves as the patient's first point of entry into the health care system and as the continuing focal point for all needed health care services. Primary care practices provide patients with ready access to their own personal physician, or to an established back-up physician when the primary physician is not available. Primary care practices provide health promotion, disease prevention, health maintenance, counseling, patient education, diagnosis and treatment of acute and chronic illnesses in a variety of health care settings (e.g., office, inpatient, critical care, long-term care, home care, day care, etc.). Primary care practices are organized to meet the needs of patients with undifferentiated problems, with the vast majority of patient concerns and needs being cared for in the primary care practice itself. Primary care practices are generally located in the community of the patients, thereby facilitating access to health care while maintaining a wide variety of specialty and institutional consultative and referral relationships for specific care needs. The structure of the primary care practice may include a team of physicians and non-physician health professionals. Definition #3 - Primary Care Physician A primary care physician is a generalist physician who provides definitive care to the undifferentiated patient at the point of first contact and takes continuing responsibility for providing the patient's care. Such a physician must be specifically trained to provide primary care services. Primary care physicians devote the majority of their practice to providing primary care services to a defined population of patients. The style of primary care practice is such that the personal primary care physician serves as the entry point for substantially all of the patient's medical and health care needs - not limited by problem origin, organ system, or diagnosis. Primary care physicians are advocates for the patient in coordinating the use of the entire health care system to benefit the patient. Definition #4 - Non-Primary Care Physicians Providing Primary Care Services Physicians who are not trained in the primary care specialties of family medicine, general internal medicine, or general pediatrics may sometimes provide patient care services that are usually delivered by primary care physicians. These physicians may focus on specific patient care needs related to prevention, health maintenance, acute care, chronic care or rehabilitation. These physicians, however, do not offer these services within the context of comprehensive, first contact and continuing care. The contributions of physicians who deliver some services usually found within the scope of primary care practice may be important to specific patient needs. However, the absence of a full scope of training in primary care requires that these individuals work in close consultation with fully-trained, primary care physicians. An effective system of primary care may utilize these physicians as members of the health care team with a primary care physician maintaining responsibility for the function of the health care team and the comprehensive, ongoing health care of the patient. Definition #5 - Non-Physician Primary Care Providers There are providers of health care other than physicians who render some primary care services. Such providers may include nurse practitioners, physician assistants and some other health care providers. These providers of primary care may meet the needs of specific patients. They should provide these services in collaborative teams in which the ultimate responsibility for the patient resides with the primary care physician. *In this document, the term physician refers only to doctors of medicine (M.D.) and osteopathy (D.O.). Types of Primary Care Physicians Your primary care physician serves as the entry point for substantially all of your medical and health care needs. He or she is your advocate in coordinating the use of the entire health care system to benefit you and takes continuing responsibility for providing your care. Primary care includes health promotion, disease prevention, health maintenance, counseling, patient education, diagnosis and treatment of acute and chronic illnesses. By regularly seeing a primary care practitioner, you can identify and control health risk factors before they become problems. Your primary care practitioner encourages you to take charge of your health and is a trusted partner in an environment where you can feel comfortable and known. All doctors are not alike. Many different health care professionals with different types of education can provide health care. Adults in your family could see an internist. Children could go to a pediatrician. Or the whole family could see a family medicine doctor. You could have a family medicine doctor and an obstetrician/gynecologist, or an internist and a geriatrician. If it's right for you, it's the right choice. Here's a guide to the five kinds of primary care doctors available at Lehigh Valley Health Network. If a physician on your care team is board-certified, he or she chose to obtain an additional credential after medical school and residency training. Board-certified physicians have completed additional education and passed an examination to earn this credential. If one of your caregivers is fellowship-trained, the physician has had additional training in a particular area of interest. Family medicine doctors: Also called family practice doctors, they see people of all ages, including infants, children, teens and seniors. They are educated and board-certified in their knowledge of the body at all ages. Internal medicine doctors: Also called internists, they generally care for people age 14 and up (the starting age can vary by practice). They are educated and board-certified in the understanding of the internal organs of the adult body. Some internal medicine and family medicine physicians also can provide care that you might not expect, like routine gynecologic care, dermatology and sports medicine. Gynecologist or obstetrician: For many women, this physician is a key health resource. Through the reproductive years and afterward, your obstetrician or gynecologist has the knowledge and experience to promote your well-being. They recommend tests and exams necessary at different stages of your life. Geriatricians: They have special education to address the specific needs of adults over age 60. They provide routine primary care, as well as medication management, physical and mental assessments related to falls, memory issues and other aspects of aging. Lehigh Valley Hospital-Cedar Crest has been nationally ranked by U.S. News & World Report as one of "America's Best Hospitals" in geriatrics, and LVH-Muhlenberg is ranked as high-performing. Pediatricians: Every child needs to see a doctor – in fact, more often than adults. Pediatricians are specially educated to care for children, ranging from newborns through age 21. If your child needs special care, our pediatricians work closely with our specialists so your child can receive the best care. MD or DO? So you've narrowed down the type or primary care doctor you'd like to see. Now you may have questions about whether you'd prefer an MD or a DO. Here is some information to help you choose. MD stands for medical doctor, a doctor who trained at a medical school. DO stands for doctor of osteopathic medicine, who trained at a college of osteopathic medicine. They represent two branches of medicine that started out completely separate but have grown more alike over 125 years. Both types of physicians spend the same number of years training, must pass a licensing exam, and are licensed to provide all types of medical care, including surgery. Most people are familiar with how medical doctors are trained in understanding the body and treating disease. Osteopathic medicine was founded in 1874 based on a "whole person" approach that emphasizes preventive care and wellness. Osteopaths also receive ongoing education in the musculoskeletal system, and some but not all osteopaths perform osteopathic manipulative treatments. Because of this "whole person" approach, about two-thirds of osteopaths choose to become primary care doctors. Today, the two branches of medicine seem more alike than different. MDs emphasize preventive care and wellness, and a growing number of osteopaths are choosing to become specialists. Can so many residents be screened for so many medical conditions in one day by a few medical doctors? No, they cannot. How many residents should be assigned to a medical doctor for primary health care? One handred patients per medical doctor. What should a health care resource be able to provide in primary health care? Why You Need a Primary Care Physician Your Primary Care Physician: The Go-To Person for Good Health and Excellent Medical Care Choosing a primary care physician and maintaining the relationship with regular visits is an important step you can take to protect your health, at any age. When you get ill or injured, your primary care doctor is the person in charge of seeing that you get the medical care you need and he/she is also focused on keeping you well and healthy so that you can live life the way you want to. What Do Primary Care Doctors Do? Your primary care doctor's responsibilities are divided into three areas: •Preventive care to help you stay healthy: Your primary care physician offers advice on how to live a healthy lifestyle and makes sure you get screenings and immunizations when you need them. •Treating illnesses and injuries: Primary care doctors diagnose and treat common medical conditions, assess the severity of medical problems, refer patients to specialists when necessary, treat illnesses and help you manage chronic diseases, such as diabetes or hypertension (high blood pressure). •Coordinating all your medical care: Medical care can get complicated, particularly as you age and if you have one or more chronic medical conditions. Your primary care doctor keeps track of your health, including treatments and medications, makes sure you see the right doctors at the right times and communicates with them about what's going on with your health, and serves as the point person to make sure that your medical treatments and medications won't interact dangerously with one another. What Are The Benefits of Having a Primary Care Doctor? Today's health care environment is complex. As your go-to health care provider, your primary care physician protects you and represents your interests in a variety of ways, including: •Overseeing your care. In his/her role as coordinator of your care, your primary care doctor keeps all doctors informed of your health status and treatments so you don't undergo unnecessary tests or procedures or have treatments you don't want or don't need. •Lower medical costs. Keeping an up-to-date medical record of all your care, tests and treatments, your primary care physician ensures that you aren't paying for care you don't need. •Keeping you healthy, particularly as you age. Your primary care doctor monitors health changes and, seeing you year after year, may detect changes or signs of developing disease at the earliest, most treatable stages. Advising you on necessary health screenings is another important service your primary care physician can provide. When Do You Need A Primary Care Doctor? Even when you are in good health it is important to have a good relationship with your primary care physician. He/she will keep you healthy with physical examinations, immunizations and health education information. Your primary care doctor will let you know whether or not you need to get a flu shot and whether you need certain tests, such as heart screenings and cancer screenings. When you get injured or are feeling unwell, your primary care doctor can diagnose and treat your problem. An important advantage of having a primary care doctor is that you will always know that your care is being directed by a doctor who knows and understands all of your medical needs. He/she should be your first stop for all your medical concerns, including undiagnosed, non-emergencies, such as: •Colds vs. Flu. If you have a sore throat or chest cold symptoms, your primary care doctor will help determine whether you are suffering a common cold, a virus or the flu. •Infections. Primary care doctors can diagnose and treat ear infections, eye infections and other common complaints. •Stomach upset. Your primary care doctor can help determine whether your digestive upset is caused by a stomach flu, a food-borne illness, or may be something more serious or complicated that requires a visit to a specialist. •Injuries. If you fall or are injured during your normal activities or even while playing sports, your primary care physician can assess your condition and determine whether you need an x-ray or to see an orthopedic specialist. •Chronic disease management. Your primary care doctor will also help you manage chronic conditions, such as diabetes, hypertension and high cholesterol. •Care Coordination. If you need to see a medical specialist, your primary care doctor coordinates and manages your care, making sure that treatments you receive are appropriate for you, that the drugs you are prescribed work well together, and that all the doctors who care for you know about other medical problems you may be having. Here are further guidelines. |
Primary care diseases and conditions with treatment.
| Lung Disease Alphabetical Listing | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Breast Conditions | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Eye Disorders | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Infectious Diseases | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Orthopedic Disorders | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Skin Disorders | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Developmental Disorders | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Endocrine Diseases | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hypoxemia (low blood oxygen)… | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Minor Cuts, Scrapes, and Skin Wounds | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sports Injuries | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Stress | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Oral Conditions in Older Persons | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Substance Abuse | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Common Breast Conditions
Common Endocrine Diseases Minor Cuts, Scrapes, and Skin Wounds Listed in the directory below is some additional information about minor cuts, scrapes, and skin wounds, for which we have provided a brief overview. |
Respiratory poisons
Human medicolegal cases
|
Cell Respiration
Respiratory poisons A wide variety of different compounds act as respiratory poisons, and inhibit the oxidation of metabolic fuels linked to the phosphorylation of ADP to ATP. Cyanide and carbon monoxide, well known poisons. Sodium azide - another well-known poison Antimycin - one of a family of antibiotics produced by Streptomyces spp., some of which are used as fungicides against fungi that are parasitic on rice. Amytal (amobarbital) - a barbituric acid derivative widely used as a sedative or hypnotic drug. Rotenone - the main insecticidal compound in derris powder, extracted from the root of the leguminous plant Lonchocarpus nicou. Oligomycin - one of a family of antibiotics produced by Streptomyces spp., which is of little or no therapeutic use. Atractyloside - a toxic alkaloid from the rhizomes of the Mediterranean thistle Atractylis gummiferra. It competes with ADP for binding to the adenine nucleotide transporter. Bongkrekic acid - a toxic antibiotic formed by Pseudomonas cocovenans growing on coconut. It anchors the adenine nucleotide transporter at the inner face of the membrane, so that ATP cannot be transported out, nor ADP in. Cell Respiration Explained 1. How does the poison cyanide act upon the aerobic respiration? Cyanide is a poison that inhibits the last cytochrome of the respiratory chain, interrupting the ATP formation and thus leading the cell to death. 2. What is the compound that is phosphorylated for ATP formation? What is the resulting compound when ATP liberates energy? ATP, or adenosine triphosphate, is formed after the binding of one phosphate (phosphorylation) to one ADP (adenosine diphosphate) molecule. This is a process that stores energy into the produced ATP molecule. When ATP gives energy to the cellular metabolism it loses one of its phosphates and ADP reappears. ADP can also lose more phosphates and generate AMP (adenosine monophosphate) or even non-phosphorylated adenosine. Adenosine production from ATP is a solution used in tissues that need urgent oxygen supply, for example, in the heart during myocardial infarction (heart attack), since adenosine has a local vasodilator effect thus providing faster vasodilation than other physiological methods. 3. What are the types of cell respiration? There are two types of cell respiration: aerobic cell respiration, a reaction with participation of molecular oxygen (O2), and anaerobic cell respiration, without participation of molecular oxygen but with other inorganic molecules as oxidant. There are several varieties of anaerobic cell respiration, the main one is fermentation. 4. Under which conditions do aerobic cells carry out fermentation? Some cells that usually obtain energy from aerobic cellular respiration can carry out fermentation when oxygen is not available. There are bacteria and fungi that under absence of oxygen use their anaerobic metabolic capability for energetic supply. Muscle cells carry out fermentation too when oxygen is scarce. 5. What is the difference between aerobic and anaerobic beings? Aerobic organisms are those whose cells do not survive without oxygen since they depend on aerobic cell respiration to obtain energy for ATP production. Anaerobic organisms are those that live or can live under oxygen-lacking environments. 6. What is the difference between facultative anaerobic beings and obligate anaerobic beings? Facultative anaerobic beings, like the fungi Saccharomyces cerevisiae, a brewing yeast, can survive under oxygen-poor environments carrying out fermentation. However when oxygen is available these beings carry out aerobic respiration. Obligate anaerobic beings are those that cannot survive when oxygen is present. Some fungi, some bacteria (like the agent of botulism Clostridium botulinum, and the agent of tetanus, Clostridium tetani) and some protozoans are examples of obligate anaerobes. 7. What are the two types of fermentation? What are their chemical equations? The two main types of fermentation are alcoholic fermentation and lactic fermentation. In alcoholic fermentation pyruvic acid, an intermediate molecule, is converted into ethanol with liberation of carbon dioxide. The alcoholic fermentation equation is as follows: C6H12O6 + 2 ADP + P --> 2 C2H5OH + 2 CO2 + 2 ATP In lactic fermentation pyruvic acid is transformed into lactic acid and there is no production of carbon dioxide. The lactic fermentation equation is: C6H12O6 + 2 ADP + P --> 2 C3H5OOH + 2 ATP 8. In general what are the reagents and products of fermentation? In fermentation glucose (sugar) is degraded into pyruvic acid (each glucose molecule forms two pyruvic acid molecules). In this process two molecules of ATP are produced. According to the type of fermentation, pyruvic acid can produce ethanol and carbon dioxide (in alcoholic fermentation) or lactic acid (in lactic fermentation). There are other varieties of fermentation in which pyruvic acid can generate acetic acid (acetic fermentation), propionic acid, isopropanol (an alcohol too), etc. The type of fermentation depends on the species of the involved organisms. 9. Why in cake and bread manufacture are alcoholic fermenting organisms used and not lactic fermenting organisms? Fermentation has the function of making cakes and breads grow. This is accomplished by liberation of carbon dioxide in alcoholic fermentation as the gas passes through the dough and makes it grow. In lactic fermentation there is no liberation of carbon dioxide and the desired result would not be obtained. 10. To what substance is the acidic flavor of fermented milk due? Some bacteria ferment milk lactose by lactic fermentation producing lactic acid. This product is responsible for the acidic flavor of yogurts, curd and milk. 11. How can the knowledge about fermentation explain the origin of muscle cramps and pains after intense physical exertion? A typical fermentation process due to oxygen scarcity happens in the muscle tissue. Under intense use muscles demand too much energy (ATP) and consume much more oxygen to produce that energy. High consumption leads to oxygen scarcity and the muscle cells begin to make lactic fermentation trying to satisfy their energetic needs. In this situation muscle pain, cramps and fatigue are due to the lactic acid released by fermentation. 12. How many ATP molecules are produced for each glucose molecule used in fermentation? How many ATP molecules are produced for each glucose molecule used in aerobic respiration? In fermentation from one glucose molecule two ATP molecules are produced. In aerobic respiration, a much more productive process, from one glucose molecule 36 ATP molecules are made. 13. Which is the cell organelle that is specialized in aerobic respiration? The cell organelles that are specialized in aerobic respiration are the mitochondria. 14. Of which main compounds is the mitochondrion structure made? Mitochondria are organelles delimited by two lipid membranes. The inner membrane invaginates to the interior of the organelle forming cristae and delimiting an internal space known as the mitochondrial matrix. 15. What are the three phases into which the cell respiration is divided? The three phases of aerobic cell respiration are glycolysis, Krebs cycle and respiratory chain (also known as the electron transport chain). 16. What is glycolysis? What are the products of this process? Glycolysis, the first stage of the aerobic cell respiration, is a process in which glucose is degraded (broken) to form two pyruvic acid molecules along with the formation of two ATP and two NADH. Glycolysis is a complex reaction implying the formation of several intermediate molecules until pyruvic acid molecules are made. Although two ATP molecules are consumed in the reaction, there is also production of four molecules of ATP, thus a positive balance of two ATP molecules is obtained. Two NADH molecules are also produced. In glycolysis the 6-carbon structure of glucose is broken and two organic chains of three carbons each are made; these chains give birth to two pyruvic acid molecules. Cell Respiration Review - Image Diversity: glycolysis 17. Does glycolysis occur within the mitochondria? Glycolysis happens in the cytosol and not within the mitochondria. Pyruvic acid molecules later enter mitochondria to participate in the next phase of the aerobic cell respiration. 18. How many ATP molecules are made after glycolysis? Glycolysis is a process similar to glucose degradation in fermentation. It produces (final balance) two molecules of ATP for each broken glucose. 19. What is NAD? What is the role of the NAD molecule in glycolysis? NAD (nicotinamide adenine dinucleotide) is a hydrogen acceptor necessary as reductant (to receive hydrogen) in some reactions in which it is reduced and converted into NADH2. During glycolysis two NAD molecules retrieve hydrogens liberated after an intermediate reaction thus forming NADH2. 20. What happens during aerobic respiration to the pyruvic acid molecules made by glycolysis? What is the sequence of reactions that then follows? The pyruvic acid molecules made in cytosol by glycolysis enter into the mitochondria. Within the mitochondria each pyruvic acid molecule is converted into one molecule of acetyl-CoA (acetyl coenzyme A) with liberation of one carbon dioxide. The Krebs cycle (also known as citric acid cycle), the second stage of aerobic respiration, then begins. 21. What is the official name of pyruvic acid? Pyruvic acid is 2-oxopropanoic acid. It is thus a molecule made of three linearly bound carbons with one extremity forming the organic acid function (COOH) and the middle carbon binding to an oxygen atom by double bond. 22. Why can it be said that each glucose molecule runs the Krebs cycle twice? Each glucose molecule “cycles” the Krebs cycle twice because after glycolysis each used glucose has generated two pyruvic acid molecules and each pyruvic acid is converted in a 1:1 proportion into acetyl CoA. Each acetyl CoA then cycles the Krebs cycle once. 23. Why is the Krebs cycle also called the final common pathway of the degradation of organic compounds? The Krebs cycle is called the final common pathway of the degradation of organic compounds because it is also possible to generate acetyl CoA from the degradation of lipids and proteins. Since acetyl CoA is the substrate that triggers the Krebs cycle, this process is called the final common pathway for being activated by other organic molecules (lipids and proteins) and not only by glucose. The organism uses energetic reserves of fat and proteins to cycle the Krebs cycle when undergoing malnutrition or when there is no glucose available for the cells. 24. What are the final energetic products of each round of the Krebs cycle? Where is most part of the utile energy at the end of Krebs cycle found? After each round of the Krebs cycle two carbon dioxide molecules, eight protons (hydrogen ions) captured by NAD and FAD (a hydrogen acceptor too) and one ATP molecule are produced. During the Krebs cycle acetyl CoA is degraded. At the end the utile energy is incorporated into hydrogens transported by FADH2 and NADH2 molecules. 25. How many carbon dioxide molecules are liberated after each cycle of the Krebs cycle? For a single glucose how many carbon dioxide molecules were already liberated by the aerobic respiration at that point? Each round of the Krebs cycle liberates two carbon dioxide molecules. At the end of the cycle all carbon atoms from the original glucose molecule degraded in glycolysis are already liberated incorporated into carbon dioxide molecules. That occurs because for each glucose two pyruvic acid molecules were made by glycolysis. Each of these two pyruvic acids then is converted into acetyl CoA with liberation of one carbon dioxide molecule (two in total). Since each of the two produced acetyl CoA cycles the Krebs cycle once, from the initial glucose two rounds of the Krebs cycle is generated and so four other carbon dioxide molecules are made. All of the six carbons of the glucose molecule are then incorporated into six carbon dioxide molecules (two made during acetyl CoA formation and four during the two cycles of the Krebs cycle). 26. Where in mitochondria does the process called respiratory chain occur? Which are the products of the Krebs cycle used in that final phase of the aerobic respiration? Respiratory chain, or the electron transport chain, is performed by protein systems located in the inner membrane of the mitochondria. Energized electrons of hydrogen atoms transported by NADH2 and FADH2 are the products of the preceding phases used in the respiratory chain. Cell Respiration Review - Image Diversity: respiratory chain 27. What are cytochromes? Cytochromes are proteins of the internal mitochondrial membrane that are specialized in electron transfer and participate in the respiratory chain. Energized electrons liberated by the hydrogen donors NADH2 and FADH2 (then reconverted into NAD and FAD) pass through a sequence of cytochromes losing energy in each passage. The energy is then used in the synthesis of ATP. 28. How in the respiratory chain do electrons from FADH2 and NADH2 passing through cytochromes liberate energy for the ATP synthesis? What is this ATP synthesis called? FADH2 and NADH2 oxidate into FAD and NAD and liberate hydrogen ions and highly energized electrons in the beginning of the respiratory chain. The energy lost by electrons that pass through the cytochromes is used to pump protons (hydrogen ions) out of the inner mitochondrial membrane (to the region between the inner and the outer membranes of the mitochondrion). Hydrogen concentration gradient between the inner and the outer spaces delimited by the inner membrane forces protons (hydrogen ions) to return to the mitochondrial matrix (the region inside the inner membrane) however that return is only possible if hydrogen ions pass through an enzymatic complex called ATP synthetase embedded in the inner membrane. In that passage the ATP synthetase phosphorylates ADP and then ATP molecules are produced. Hydrogen liberated in the mitochondrion then combines with oxygen to form water. As a reaction that depends on oxygen this type of ATP synthesis is called oxidative phosphorylation. 29. Until the Krebs cycle, aerobic respiration can be described without mentioning oxygen, the chemical element after which the reaction gets its name. Where in the process does this chemical element take part? What is its importance? Oxygen enters the aerobic respiration in its final phase, the respiratory chain. It is of fundamental importance because it is responsible for the maintenance of the hydrogen concentration gradient between the spaces separated by the inner mitochondrial membrane. This gradient promotes the functioning of the ATP synthetase and thus the phosphorylation of ADP to form ATP. In the space inside the inner membrane oxygen binds to free hydrogens to form water and this hydrogen consumption keeps the hydrogen gradient and the proton traffic through the ATP synthetase. The entire aerobic respiration process has the intent to make the ATP synthetase work. Aerobic beings, for example, we humans, need to breathe oxygen to maintain that hydrogen concentration gradient and keep the ATP synthetase working. Cell Respiration Review - Image Diversity: ATP synthetase 30. How do cells obtain energy for their functioning? Cells obtain energy for their metabolic reactions from the breaking of organic molecules with high energetic content. This energy is mostly stored as ATP molecules. The process of obtaining energy in order to produce ATP molecules is named cellular respiration. 31. What is anoxia? Anoxia is a situation in which there is no available oxygen in the cell. Whitout oxygen the respiratory chain stops, there is no ATP production, the cell does not obtain energy and dies. Anoxia can be caused, for example, by pulmonary insufficiency (drowning, extensive pulmonary injuries, etc.), by obstructions, halts and deficiencies in tissue circulation (atherosclerosis of the coronary arteries that irrigate the myocardium, tourniquets, heart arrest), by hemolysis (lysis of red blood cell) or hemoglobin diseases (anemias, fetal erythroblastosis), etc. 32. How many ATP molecules are made after the aerobic respiration and what is the net energetic gain of the process? After aerobic respiration 38 ATP molecules are made with the consumption of one glucose molecule (but two of these ATP are consumed by glycolysis). The net gain of the process is then 36 ATP molecules per glucose molecule. 33. What is the general equation of the aerobic respiration (also representing ADP and phosphate)? The general equation of the aerobic respiration is: C6H12O6 + 6 O2 + 36 ADP + 36 P --> 6 CO2 + 6 H2O + 36 ATP 34. Why can the consumption of molecular oxygen indicate the metabolic rate of aerobic organisms? Molecular oxygen (O2) consumption has direct relation to the cell metabolic rate in aerobic cells and so to the metabolic rate of the organisms. Cells having higher metabolic activity demand more energy and such energy comes from ATP molecules. As there is need for ATP production, the intensity of aerobic cell respiration is also higher and then more oxygen is consumed. |
Dyspnea (Shortness of Breath)
|
What is dyspnea? •Dyspnea is a condition where you are experiencing shortness of breath, or breathlessness. •Dyspnea is also the uncomfortable sensation of breathing. Normally, our bodies will regulate the act of breathing without even having to think about it. •You may experience dyspnea at rest, or on exertion (when you perform any activity no matter how small), if you have certain conditions. List of causes of shortness of breath Many different conditions can lead to the feeling of dyspnea (shortness of breath). The most common cardiovascular causes are acute myocardial infarction and congestive heart failure while common pulmonary causes include: chronic obstructive pulmonary disease, asthma, pneumothorax, and pneumonia. Pulmonary
Common causes of dyspnea include: •Heart problems - including: •Irregular heart beats •Fluid accumulation around the heart due to certain forms of cancer (pericardial effusion) •A recent heart attack which may be blocking blood flow •Heart failure- when your heart is not working as well as it should •Lung problems - including: •A blockage by a foreign body in your upper or lower airway passages, by tumor, infection, or even may be caused by choking on a piece of food •People with cancer of the lymph nodes in your chest may get a blockage of blood flow through the blood large vessels. This is called superior vena cava (SVC) syndrome. People with Hodgkin's disease, lung or breast cancer are most susceptible. •Constriction of your lung passages caused by secretions are common in acute (happening suddenly), or chronic (occurs for a long time) bronchitis, asthma, and Chronic Obstructive Lung Disease (COLD). •Fluid accumulation in your lungs due to a tumor or infection (pleural effusion) •Pneumonia - caused by one of many types •Upper Respiratory Infection (URI) - either caused by a virus or bacteria •Pulmonary fibrosis - lung damage from radiation, chronic diseases, or chemotherapy •Pulmonary toxicity - lung damage from chemotherapy, radiation therapy, or chronic diseases •Pneumothorax - a collapsed lung from tumor or trauma (like a car accident, or a gun shot wound) •Blood clots in your lungs (pulmonary emboli) Other causes: •Anemia - Low blood hemoglobin (Hgb) counts that may occur with blood loss, if you are low in iron stores, or after chemotherapy •If you are hyperventilating, or breathing really fast due to fear, anxiety, or unknown causes •Things that may also put you at risk (called risk factors) for developing dyspnea may include: •Smoking cigarettes •Environmental irritants, such as pollution, chemicals and hair spray •If you are elderly, or have an altered immune system from chemotherapy, long-term steroid use, or chronic diseases •You may be treated with antibiotics if there are bacteria present in a sputum sample, or if your healthcare provider is concerned that bacteria caused your infection. •If your bronchitis, pneumonia or other cause of dyspnea are due to a virus, your symptoms may take 2 or more weeks to resolve, but antibiotics won't help. Treatment of a virus includes cough medications, drinking lots of fluids, and avoiding irritants. •Your dyspnea may be due to a chronic, or a long-term disease, such as pulmonary fibrosis, or chronic bronchitis. You may go through periods when you feel well, and then go through periods when you feel ill. •With some causes of dyspnea, such as chronic bronchitis, and pulmonary fibrosis, severe outbreaks of cough, shortness of breath and congestion (called exacerbations), may last for a few months at a time, and occur a few times a year. What are some symptoms to look for? •You may notice chest tightness, difficulty getting a good breath, feelings of breathlessness, or that you is hungry for air. •You may notice that you are wheezing, when you breathe. •You may have fever, chills, or a headache. •You may have pain in your muscles, or pain in your lungs when you take a deep breath, especially if you are coughing really hard, for long periods of time. •You may be overly tired, or very weak (fatigued). It may be hard for you to do any kind of your normal activities. •You may have sudden onset of coughing spellsor a long-term (chronic) cough. You may or may not be able to bring up any secretions (sputum), or you may bring up greenish-yellow, or rusty-colored sputum. •You may experience shortness of breath, either at rest or while performing any type of activity. This may include walking to the door, or climbing stairs. •You may have trouble lying flat in bed, and you may have to sleep on 2 or more pillows. Your shortness of breath may cause you to wake up in the middle of the night. •If your heart may not be working as well, your legs may be swollen, especially in your feet and ankles. You may gain "water" weight easily, or feel bloated. Things you can do: •Make sure you tell your doctor, as well as all healthcare providers, about any other medications you are taking (including over-the-counter, vitamins, or herbal remedies). •Remind your doctor or healthcare provider if you have a history of diabetes, liver, kidney, or heart disease. If you have a family history of heart disease, stroke, high blood cholesterol, or high blood pressure, in a first or second-degree relative, you may be at risk for certain problems. Notify your healthcare provider if you have any of these diseases in your family. •If you are smoking, you should quit. If you do not smoke, avoid smoke-filled rooms. Smoking first or second-hand can damage lung tissue, and make your dyspnea worse. Discuss with your healthcare provider techniques that can help you quit. •Avoid people who are sick. Wash your hands often, with soap and water, for at least 15 seconds at a time. Use tissues when you sneeze or cough. •Do not share eating or drinking utensils with anyone. •If you are over the age of 65 years, or have an altered immune system due to chemotherapy, chronic disease or steroid use, _______. •People with lung problems need to circulate air from the bottom of their lungs and out of your lungs (oxygenation), to prevent infection and pneumonia. Using an incentive spirometer for 15 minutes a day, twice a day, can help promote oxygenation. •Controlling secretions through coughing and deep breathing will help you to breathe easier. Remember, if you are dehydrated, your secretions will be thicker, and harder to bring up. Make sure to drink 2 to 3 liters of fluids (non-alcoholic, non-caffeinated) per day, to remain well hydrated. •Taking warm showers or baths, and using a vaporizer, may help to thin out your secretions. •Try to exercise, as tolerated, to promote air exchange (oxygenation), and to maintain your optimal level of functioning. Walking, swimming, or light aerobic activity may also help you to lose weight, and feel better. Make sure to exercise, under the supervision of your healthcare provider, and discuss with your healthcare provider how you can create a specific exercise program to suit your needs. •If you are experiencing heart failure, which may have caused your breathing problems, you may be told to reduce the amount of salt you are eating in a day. Many times, it may be restricted to about 2 grams of sodium per day. A diet lower in salt may decrease the amount of work that is placed on your heart. You should discuss this with your healthcare provider how you can specifically use your diet to control your symptoms. •Try to avoid "environmental allergens" (such as smoke, pollution, and common causes of seasonal allergies), as well as things that may cause allergies in your home (hair sprays, mold, dust mites, and pets). These may trigger an episode of coughing and dyspnea, and make your symptoms worse. •Keep a diary of your any abnormal symptoms, such as excessive fatigue, shortness of breath or chest pain, if these are occurring regularly. Write down the foods that you have eaten, the exercise or activity you were undergoing when the symptoms occurred, and how you felt before they occurred. This diary may be valuable in determining the cause of your symptoms, and help you to identify certain "triggers" of your symptoms. •Questions to ask yourself, may include: •Did my symptoms occur gradually, or did this episode come on all of a sudden? Was I feeling anxious? Did I perform any kind of activity, or was I resting? •Did I eat any different kinds of foods? Was I around any pets? Did I travel recently? What did I do differently? •With severe breathing problems, sleeping at night with your head of the bed elevated may make it easier to breathe. You may do this by sleeping on 2 or 3 extra pillows. This will help lung expansion (spreading out), as well as promote the drainage of secretions. •Use relaxation techniques to decrease the amount of anxiety you have. If you feel anxious, place yourself in a quiet environment, and close your eyes. Take slow, steady, deep breaths, and try to concentrate on things that have relaxed you in the past. •You should restrict the amount of alcohol you take in, or avoid it all together. Alcohol may adversely interact with many medications. •Participating in support groups may be helpful to discuss with others what you are going through. Ask your healthcare provider if he or she is aware of any support groups that would benefit you. •If you are ordered a medication to treat this disorder, do not stop taking any medication unless your healthcare provider tells you to. Take the medication exactly as directed. Do not share your pills with anyone. •If you miss a dose of your medication, discuss with your healthcare provider what you should do. •If you experience symptoms or side effects, especially if severe, be sure to discuss them with your health care team. They can prescribe medications and/or offer other suggestions that are effective in managing such problems. •Keep all your appointments for your treatments. Drugs that may be prescribed by your doctor: •Depending on your lung function, and your overall health status, your doctor may recommend that certain drugs be used to help your lungs function more effectively, and decrease symptoms. Some of the common drugs that are used to treat lung problems may include: •Antianxiety medications: If you are experiencing anxiety with your dyspnea, depending on the cause, your healthcare provider may prescribe an anti-anxiety medication, called an anxiolytic. These medications will help you to relax. These may include lorazepam (Ativan®), or alprazolam (Xanax®). It is important to take these medications only when you are feeling anxious. Do not operate heavy machinery, or drive an automobile while taking these. These medications must be used very cautiously if you have severe dyspnea. Discuss the risks and benefits of taking this medication with your doctor or healthcare provider. •Antibiotics - If your doctor or healthcare provider suspects that you have a lung infection, he or she may order antibiotic pills or intravenous (IV), depending on how severe your illness is, and your overall health status. Commonly prescribed antibiotics for bronchitis, pneumonia and respiratory (breathing) problems include azithromycin (Zithromax®), and levofloxacin (Levaquin®). If you are prescribed antibiotic pills, take the full prescription. Do not stop taking pills once you feel better. •Anticoagulants - These medications prevent your blood from clotting, or may be ordered by your healthcare provider if you have a blood clot. Each of them works in a variety of ways. Depending on your overall health status, the kind of ________ you are receiving, and the location of the blood clot, your healthcare provider may suggest warfarin sodium (Coumadin®), or enaxoparin (Lovenox®). •Anticholinergic agents - these drugs are given to persons with chronic bronchitis, emphysema, and chronic obstructive lung disease (COLD). Anticholinergic agents work in a complex manner by relaxing the lung muscles, which will help you to breathe easier. A commonly prescribed drug is ipatropium bromide (Atrovent®). •Bronchodilators - These drugs work by opening (or dilating) the lung passages, and offering relief of symptoms, including shortness of breath. These drugs, typically given by inhalation (aerosol), but are also available in pill form. •Beta-adrenergic receptor agonists (beta-agonists) - Beta-agonists can be considered bronchodilators, as these drugs relax airway smooth muscle, and block the release of substances that cause bronchoconstriction, or narrowing of your lungs, if you are having a lung "spasm." Drugs such as albuterol (Proventil®), or terbutaline (Brethine®), are commonly used. •Corticosteroids: Steroids work by decreasing inflammation and swelling, which may be present with certain lung disorders. People may benefit from steroids, either inhaled, by pill form, or in the vein (IV). •Beclomethasone (Beclovent®), an inhaled steroid, is useful in the treatment of chronic asthma and bronchitis. Inhaled steroids act directly on the lung tissue, so there are fewer long-term side effects, compared with a pill or IV form. •People who have an outbreak of severe shortness of breath and airway inflammation may be ordered a steroid pill, such as prednisone, for a short period of time. This is usually given with inhaled steroids. •Patients with severe asthma may require IV administration of another steroid, methylprednisolone (Solumedrol®). •Cough medications/Decongestants - may help you to be more comfortable if you are coughing a lot. Guaifenesin is an active ingredient in many cough medications, may be given alone, but is often combined with other drugs, such as codeine, to help your cough. Guaifenesin may also be combined with pseudoephedrine (Sudafed®) as a decongestant, or any one of many medications, depending on your symptoms. Another common medication you may receive is Hydrocodone Bitartrate-Homatropine Methylbromide (Hycodan®). This is a narcotic antitussive (anti-cough medication), which will help relieve your cough. •Diuretics - may be known as "water pills" as they work to prevent or treat lung congestion by making you urinate out extra fluid. Some examples of this medication may include furosemide (Lasix®), and Hydrochlorthiazide. You may receive this medication alone or in combination with other medications. •Oxygen therapy - If you are experiencing shortness of breath at rest, or on exertion, your healthcare provider may see if oxygen therapy is right for you. You may take oxygen when your symptoms are at their worst. For example, some people are only on oxygen at nighttime, and not during the day. Some take oxygen when they are performing activities, but not all the time. •Your healthcare provider will discuss with you which treatments are helpful to you. •Do not stop any medications abruptly, as serious side effects may occur. When to call your doctor or health care provider: •Fever of 100.5º F (38º C), chills, sore throat. •If you cough up blood •Shortness of breath, chest pain or discomfort; swelling of your lips or throat should be evaluated immediately •Feeling your heart beat rapidly, or have palpitations •Any new rashes on your skin •Any unusual swelling in your feet and legs •Weight gain of greater than 3 to 5 pounds in 1 week. •Any symptoms that worsen and do not improve Breathing & Respiratory System 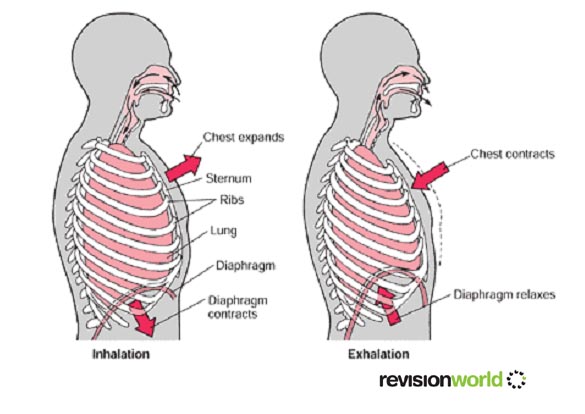
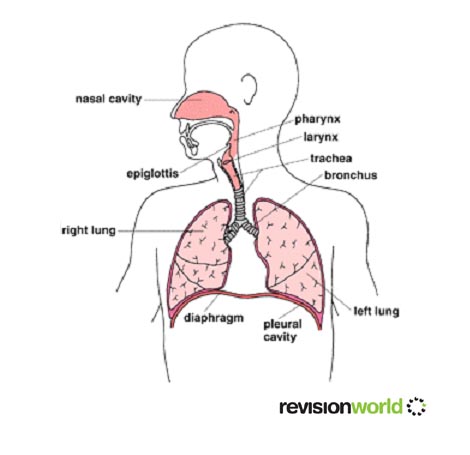
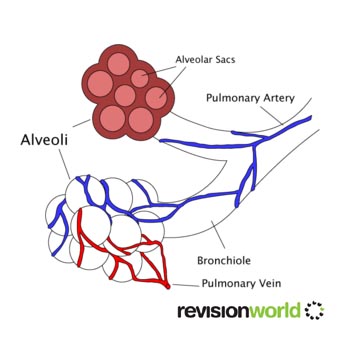
Breathing The Breathing Process - Questions and Answers Chest Cavity Exchanging Oxygen and Carbon Dioxide Control of Breathing Defense Mechanisms of the Respiratory System Effects of Aging on the Respiratory System When we breathe in and out we suck air into them then expel it again. Oxygen is absorbed from the lungs into the blood, and carbon dioxide is removed from the blood and breathed out from the lungs. This exchange is vital. Respiratory System Respiration is the release of energy from glucose or other organic substances. Energy is required for growth, repair, movement and other metabolic activities. There are two main types of respiration, aerobic and anaerobic. Alveoli Alveoli are the final branchings of the respiratory tree and act as the primary gas exchange units of the lung Used for exchanging gases: Deoxygenated enters lungs from body, oxygenated enters capillaries from lungs Advantages of alveoli •Moist •Large surface area •Good blood supply Aerobic Respiration Aerobic respiration takes place in the presence of oxygen. Aerobic respiration = glucose reacts with oxygen to release energy. Carbon dioxide and water are released as waste products. Glucose molecules react with oxygen molecules to form carbon dioxide and water molecules, with energy being released by the breaking of bonds in the glucose molecules. Our bodies require energy for the seven life processes This energy is obtained from respiration. glucose + oxygen > water + carbon dioxide + energy . We use the energy released from respiration for many processes. Respiration also gives off heat, which is used to maintain our high body temperature. Our rate of respiration can be estimated by measuring how much oxygen we use. During exercise, the body needs more energy and so the rate of respiration increases - The breathing rate increases to obtain extra oxygen and remove carbon dioxide from the body. The heart beats faster so that the blood can transport the oxygen and carbon dioxide faster. This is why our pulse rate increases. It is actually the build up of carbon dioxide that makes us breathe faster. Glucose comes from our food, oxygen and from breathing Water and carbon dioxide are exhaled Anaerobic respiration Anaerobic respiration occurs when oxygen is not available. When not enough oxygen is available, glucose can be broken down by anaerobic respiration. This may happen during hard exercise. Glucose is only partially broken down, and lactic acid is produced - together with a much smaller amount of energy. Energy can still be produced without oxygen Only a little bit of energy is obtained from respiration glucose > lactic acid + energy Anaerobic respiration occurs in humans when oxygen is not obtained quick enough (e.g. running fast) Only 1/20th energy amount is produced compared to aerobic respiration Lactic acid builds up, which causes muscle fatigue due to oxygen debt. This is overcome by deep breathing to oxidise the acid. After the exercise is finished, extra oxygen is needed by the liver to remove the lactic acid. Being able to respire without oxygen sounds a great idea. However, there are two problems: •Anaerobic respiration releases less than half the energy of that released by aerobic respiration. •Anaerobic respiration produces lactic acid. Lactic acid causes muscle fatigue and pain. |
Respiratory System Quiz
|
Where in the respiratory system would you find rings of cartilage? A. ? nose B. ? diaphragm C. ? alveoli D.YES trachea Correct: trachea The bronchi are connected to the alveoli via A. ? capillaries B. ? air sacs C.YES bronchioles D. ? the trachea Correct: bronchioles Which one of the following gases is required for respiration? A. ? Methane B. ? Oxygen C. ? Carbon dioxide D. ? Nitrogen Correct: Oxygen Where in the respiratory system would you find rings of cartilage? 0. ? nose0. ? diaphragm0. ? alveoli0.YES trachea The bronchi are connected to the alveoli via0. ? capillaries0. ? air sacs0.YES bronchioles0. ? the trachea Which one of the following gases is required for respiration?0. ? Methane0.YES Oxygen0. ? Carbon dioxide0. ? Nitrogen Air that was breathed out by a human was analysed for the gases present. Which of the following is most likely to be the result of the analysis? A. ? 78% nitrogen, 16% oxygen, 4% carbon dioxide and 2% water vapour B. ? 78% nitrogen, 21% oxygen, 0.5% carbon dioxide and 0.5% water vapour C. ? 70% nitrogen, 20% oxygen, 0.5% carbon dioxide and 9.5% water vapour D. ? 80% nitrogen, 60% oxygen, 4% carbon dioxide and 6% water vapour Correct:78% nitrogen, 16% oxygen, 4% carbon dioxide and 2% water vapour Which of the following is the correct order for air passing through the lungs? A. ? trachea, bronchus, bronchiole, alveoli B. ? bronchus, trachea, bronchioles, alveoli C. ? trachea, alveoli, bronchi, bronchioles D. ? bronchus, alveoli, trachea, bronchioles Correct:trachea, bronchus, bronchiole, alveoli Air contains nitrogen. What happens to the nitrogen in inhaled air? A. ? Its exhaled again without anything happening to it. B. ? It circulates through our bloodstream. C. ? Its absorbed into the digestive system and aids digestion. D. ? Its changed into nitrogen oxide. Correct:Its exhaled again without anything happening to it. Another name for the breathing system is the A. ? digestive system B. ? nervous system C. ? respiratory system D. ? circulatory system Correct:respiratory system Which one of the following pairs of items are both necessary for respiration to take place? A. ? sunlight and carbon dioxide B. ? glucose and sunlight C. ? glucose and carbon dioxide D. ? glucose and oxygen Correct:glucose and oxygen Which one of the following is NOT a disease of the respiratory system? A. ? pneumonia B. ? chicken pox C. ? asthma D. ? cancer Correct:chicken pox Which one of the following labelled parts in the diagram is known as the intercostal muscle? A. ? D B. ? C C. ? B D. ? A Correct:C muscle1c_jpg_pagespeed_ce_9G2_LbX0dY.jpg Which one of the following protects the lungs? A. ? diaphragm B. ? trachea C. ? alveoli D. ? rib cage Correct:rib cage Name the parts labelled in the diagram bronchial1_gif_pagespeed_ce_VTPr3yC-F5.gif A. A = trachea, B = bronchiole B. ? A = alveolus, B = bronchiole C. ? A = trachea, B = bronchus D. ? A = bronchiole, B = trachea A = trachea, B = bronchiole When would a human body be most likely to respire anaerobically? A. ? When eating B. ? When watching TV C. ? When running a marathon D. ? When asleep Correct:When running a marathon The function of hair in the nose is A. ? to help fight infection B. ? to cause us to sneeze C. ? to keep water out of the lungs D. ? to help gas exchange in the lungs Correct:to help fight infection Which one of the following takes place in the lungs? A. ? Food is stored B. ? Waste material is filtered from the blood C. ? Food is digested D. ? Gas exchange Correct:Gas exchange What happens to your lungs when you breath in? A. ? They expand B. ? They absorb carbon dioxide C. ? They manufacture glucose D. ? They push up the diaphragm Correct:They expand Inhaled air contains A. ? less carbon dioxide than exhaled air B. ? more nitrogen than exhaled air C. ? less nitrogen than exhaled air D. ? less oxygen than exhaled air Correct: less carbon dioxide than exhaled air The part of the respiratory system labelled Y in the diagram is the A. ? bronchiole B. ? wind-pipe C. ? alveolus D. ? bronchus bronchial2_gif_pagespeed_ce_1q8xofIV2D.gif Correct: bronchus Which one of the following effects is NOT associated with smoking? A. ? Decreased risk of acquiring pneumonia and bronchitis. B. ? Increased risk of developing 'smokers cough'. C. ? Increased risk of lung cancer. D. ? Decreased ability of the blood to transport oxygen. Correct: Decreased risk of acquiring pneumonia and bronchitis. Name the parts labelled in the diagramA. ? C = trachea, D = alveolus B. ? C = alveolus, D = larynx C. ? C = larynx, D = trachea D. ? C = larynx, D = bronchus Correct: C = larynx, D = bronchus bronchial3_gif_pagespeed_ce_-zNfB5w0gm.gif |
Reproductive System
The Human Reproductive System
|
1. What are the organs that are part of the male genital system?
The organs that comprise the male genital system are the testicles, the epididymides, the vas deferens, the seminal vesicles, the ejaculatory duct, the prostate, the bulbourethral glands, the urethra and the penis. 2. Concerning reproduction what is the function of the testicles? The testicles are the male gonads, i.e., the organs where the production of gametes takes place. In human beings the gametes are made by meiosis that occur in the testicles. 3. After passing the epididymides through which structures do sperm cells go until exteriorization? After leaving the epididymis in the testicle sperm cells enter the vas deferens, after that they receive secretions from the seminal vesicles and gather (from right and left sides) in the ejaculatory duct that passes inside the prostate. They also get secretions from the prostate and the bulbourethral glands and then go through the urethra, inside the penis, to the exterior. 4. What is the function of the secretions of the prostate, seminal vesicle and bulbourethral glands in reproduction? These secretions along with sperm cells from the testicles form the semen. The secretions have the function of nourishing the sperm cells and serving them as a fluid means of propagation. The basic pH of the seminal fluid also neutralizes the acid secretions of the vagina allowing the survival of sperm cells in the vaginal environment after copulation. 5. What are the endocrine glands that regulate sexual activity in males? How does this regulation work and what are the involved hormones? In males the sexual activity is regulated by the endocrine glands hypophysis (pituitary), adrenals and gonads (testicles). The FSH (follicle-stimulating hormone) secreted by the adenohypophysis acts upon the testicles stimulating the spermatogenesis. The LH (luteinizing hormone), another adenohypophyseal hormone, stimulates the production of testosterone by the testicles too. Testosterone, whose production intensifies after the beginning of puberty, acts in several organs of the body and it is responsible for the appearing of the male secondary sex characteristics (beard, body hair, deep voice, increase of the muscle and osseous mass, maturation of genitalia, etc.) Testosterone also stimulates spermatogenesis. 6. What are the organs that are part of the female reproductive system? The organs that constitute the female reproductive system are the ovaries, the Fallopian tubes (or uterine tubes), the uterus, the vagina and the vulva. 7. In which period of life does the formation of gametes begin in women? The meiosis that forms female gametes begins in the cells of the ovarian follicles before birth. After the beginning of puberty, under hormonal stimuli, during each menstrual cycle one of the cells is released on the surface of the ovary and meiosis resumes. The meiotic process is only concluded however if fecundation happens. 8. What is the organ that releases the female gamete under formation? How is this release triggered? What is the organ that collects the released gametes? The organ that liberates the female gamete is the ovary, the female gonad. The releasing of the oocyte is a response to hormonal stimuli. The immature egg cell (still an oocyte) falls into the abdominal cavity and is picked up by the Fallopian tube (uterine tube, or oviduct), a tubular structure that connects the ovary with the uterus. 9. What are the anatomical relationships between the organs of the female reproductive system from the external vulva to the ovaries? The external female genitalia is called the vulva. The vulva is the external opening of the vaginal canal, or vagina. The vagina is the copulation organ of the females and its posterior extremity communicates with the uterus through the uterine cervix. The uterus is divided into two portions: the cervix and the uterine cavity. The lateral walls of the uterine fundus communicate with the Fallopian tubes. The other extremity of each Fallopian tube ends in fimbria forming fringes in the abdominal cavity. Between the uterine tube and the ovary there is still intra-abdominal space. v 10. What is the menstrual cycle? The menstrual cycle is the periodic succession of interactions between hormones and the organs of the female reproductive system that, after the beginning of puberty, regulates the release of the female gametes and prepares the uterus for fecundation and pregnancy. 11. What are the endocrine glands involved in the menstrual cycle? What are the hormones in action? The endocrine glands that secrete hormones involved in the menstrual cycle are the hypophysis (pituitary) and the ovaries. The hormones from adenohypophysis are FSH (follicle-stimulating hormone) and LH (luteinizing hormone) and the hormones from the ovaries are estrogen and progesterone. 12. What event marks the beginning of the menstrual cycle? What is the blood concentration of FSH, LH, estrogen and progesterone in this phase of the cycle? By convention the menstrual cycle begins at the day that menses begins. (Menses is the endometrial hemorrhage excreted through the vaginal canal.) At these days the hormones FSH, LH, estrogens and progesterone are in low concentration. 13. After menses what is the hormone that influences the maturation of the ovarian follicles? The maturation of the ovarian follicles after menses is stimulated by the action of FSH (follicle-stimulating hormone). 14. What is the hormone secreted by the growing ovarian follicles? What is the action of that hormone upon the uterus? The follicles that are growing after menses secrete estrogen. These hormones act upon the uterus stimulating the thickening of the endometrium (the internal mucosa of the uterus). 15. What is the relationship between the estrogen level and the LH level in the menstrual cycle? What is the function of LH in the menstrual cycle and when does its blood concentration reach a peak? The increase in the blood concentration of estrogen with the growing of the ovarian follicle causes the hypophysis to secrete LH. In this phase LH acts together with FSH promoting the maturation of the follicle that at the 14th day ruptures releasing the female gamete (ovulation). After the release of the ovum LH acts stimulating the formation of the corpus luteum, a structure made from the remaining follicular mass. The LH concentration is at maximum at the 14th day of the cycle. 16. What are the hormones that promote the release of the female gamete from the follicle and at which day of the menstrual cycle does this phenomenon happen? What is this event called? The hormones that promote the release of the ovum from the follicle are FSH and LH, hormones found in maximum blood concentration around the 14th day of the cycle. The release of the female gamete from the ovary is called ovulation. Ovulation happens at (around) the 14th day of the menstrual cycle. 17. How does the female gamete move from the ovary to the uterus? The female gamete released from the ovary falls into the surrounding abdominal cavity and is collected by the Fallopian tube. The internal epithelium of the uterine tubes has ciliated cells that move the ovum or the fecundated egg cell towards the uterus. 18. How long after ovulation must fecundation occur to be effective? If fecundation does not occur approximately 24 hours after ovulation the released ovum often dies. 19. What is the structure into which the follicle is transformed after ovulation? What is the importance of that structure in the menstrual cycle? The follicle that released the ovum suffers the action of LH and is transformed into the corpus luteum. The corpus luteum is very important because it secretes estrogen and progesterone. These hormones prepare the uterine mucosa, also known as endometrium, for nidation (implantation of the zygote in the uterine wall) and embryonic development since they stimulate the thickening of the mucous tissue, increase its vascularity and make the appearing of uterine glycogen-producing glands. 20. What is the importance of the uterine glycogen-producing glands? The uterine glands produce glycogen that can be degraded into glucose to nourish the embryo before the complete development of the placenta. 21. How does the hypophysis-corpus luteum negative feedback work? What is the name given to the atrophied corpus luteum after this feedback process? After ovulation the estrogen and progesterone secretions from the corpus luteum inhibit the hypophyseal FSH and LH secretions (this happens by inhibition of GnRH, gonadotropin-releasing hormone, a hypothalamic hormone). The blood concentration of these adenohypophyseal hormones falls to basal levels again. As LH lowers the corpus luteum (luteum means “yellow”) becomes atrophic and turns into the corpus albicans (“white”). With the regression of the corpus luteum the production of estrogen and progesterone ceases. 22. In hormonal terms why does menses occur? Menses is the endometrial monthly desquamation that occurs as the estrogen and progesterone levels fall after the regression of the corpus luteum because these hormones, mainly progesterone, can no longer support and maintain the thickening of the endometrium. 23. What is the explanation for the bleeding that accompanies menses? The hemorrhage that accompanies menses occurs because the endometrium is a richly vascularized tissue. The rupture of blood vessels of the uterine mucosa during the menstrual desquamation causes the bleeding. 24. Which are the phases of the menstrual cycle? The menstrual cycle is divided into two main phases: the follicular (or menstrual) phase and the luteal (or secretory) phase. The menstrual phase begins at the first day of menses and lasts until ovulation (around the 14th day). The luteal phase begins after ovulation and ends when menses begins (around the 28th day). 25. Including main events and hormonal changes how can the menstrual cycle be described? One can imagine a cycle like an analog clock at which at 0 o’clock is the beginning and the end of the menstrual cycle and that 6 o’clock corresponds to the 14h day of the cycle. At 0 o’clock the menses and so the menstrual cycle begins and FSH blood level begins to increase. Around 2 o’clock the maturing follicles under FSH action are already secreting estrogen and the endometrium is thickening. Around 3 o’clock estrogen is intensely stimulating the increase of LH blood level. At 6 o’clock (the 14th day) LH is at its maximum concentration and FSH also at high levels to promote ovulation, LH then stimulates the formation of the corpus luteum. Around 7 o’clock the corpus luteum is already secreting a great amount of estrogen and progesterone and the endometrium thickens even more, concomitant lowering of FSH and LH occurs with the increasing of the ovarian hormones. Around 11 o’clock the reduced LH and FSH levels make the corpus luteum turn into the corpus albicans, the production of estrogen and progesterone ceases and the endometrium regresses. At 0 o’clock again (28th day) the endometrium desquamates and a new menstrual cycle begins. 26. In general what is the phase of the menstrual cycle when copulation may lead to fecundation? Although this is not a rule, to be effective fecundation in general must occur within about 24 hours after ovulation (that occurs around the 14th day of the menstrual cycle). Fecundation may occur even if copulation took place up to 3 days before ovulation since the male gametes remain viable for about 72 hours within the female reproductive system. The fertile period of the women however is considered the period from 7 days before ovulation to 7 days after ovulation. 27. What is the part of the female reproductive system where fecundation occurs? Fecundation generally occurs in the Fallopian tubes but it can also take place within the uterus. There are cases when fecundation may occur even before the ovum enters the uterine tube, a fact that may lead to a severe medical condition known as abdominal pregnancy. 28. How does the sexual arousal mechanism in women facilitate fecundation? During sexual arousal in women the vagina secretes substances to neutralize its acidity thus allowing the survival of sperm cells within it. During the female fertile period hormones make the mucus that covers the internal surface of the uterus less viscous to help the passage of sperm cells to the uterine tubes. During copulation the uterine cervix advances inside the vagina to facilitate the entering of male gametes through the cervical canal. 29. What is nidation? In which phase of the menstrual cycle does nidation occur? Nidation is the implantantion of the embryo in the uterus. Nidation occurs around the 7th day after fecundation, i.e., 7 to 8 days after ovulation (obviously, it occurs only if fecundation also occurs). Since it occurs in the luteal phase the progesterone level is high and the endometrium is in its best condition to receive the embryo. 30. What is tubal pregnancy? Many times fecundation takes place in the Fallopian tubes. Generally the newly formed zygote is taken to the uterus where nidation and the embryonic development occur. In some cases however the zygote cannot go down to the uterus and the embryo implants itself in the uterine tube tissue, characterizing the tubal pregnancy. Tubal pregnancy is a severe clinical condition since often the tube ruptures during gestation causing hemorrhage and even death of the woman. The most common treatment for tubal pregnancy has been surgery. 31. How do hormonal tests to detect pregnancy work? Laboratory tests to detect pregnancy commonly test for human chorionic gonadotropin (HCG) concentration in blood or urine samples. If the level of this hormone is abnormally high, pregnancy is likely. 32. Does the hypophysis-ovaries endocrine axis work in the same way during pregnancy as in non-pregnant women? If pregnancy does not occur how does another menstrual cycle begin? The functioning of the hypophysis is altered during pregnancy. Since estrogen and progesterone levels remain elevated during the gestational period the production of GnRH (gonadotropin-releasing hormone) from the hypothalamus is inhibited. The lack of GnRH thus inhibits the secretion of FSH and LH from the hypophysis and a new menstrual cycle does not begin. If pregnancy does not occur the lowering of estrogen and progesterone levels stimulates the production of GnRH by the hypothalamus. This hormone then hastens the adenohypophyseal secretion of FHS and LH that in their turn stimulate the maturation of follicles and the beginning of a new menstrual cycle. 33. What is the endocrine function of the placenta? The placenta besides being the organ through which the exchange of substances between the mother and the fetus is done also has the function of secreting estrogen and progesterone to keep a high level of these hormones during pregnancy. (The placenta still secretes other hormones like human placental lactogen, that act similarly to the hypophyseal hormones that regulate reproduction, and HCG, human chorionic gonadotropin.) 34. How do contraceptive pills generally work? Contraceptive pills generally contain the hormones estrogen and progesterone. If taken daily from the 4th day after menses the abnormal elevation of these hormones acts upon the hypophysis-hypothalamus endocrine axis inhibiting the FSH and LH secretions. Since these hormones then do not reach their normal high levels during the menstrual cycle ovulation does not occur. (Treatment with contraceptive pills must be initiated under medical supervision.) 35. What are the common contraindications of the contraceptive pills? There are medical reports associating the use of contraceptive pills with vomiting, nausea, vertigo, headaches, hypertension and other pathological conditions. Some research has attempted to relate the medical ingestion of estrogen and progesterone with increased propensity to cardiovascular diseases (like infarction, strokes and thrombosis) and to malignant neoplasias (cancers). Doctors must always be asked about the risks and benefits of the contraceptive pill prior to use. 36. What are the most common methods of male and female surgical sterilization? Vasectomy is the most common method of surgical sterilization in men. In vasectomy the vas deferens inside the scrotum are sectioned and closed at a section which will forbid the sperm cells to follow to the ejaculatory duct but still allowing the release of seminal fluid during ejaculation. Surgical sterilization of women is often done by bilateral tubal ligation. With tubal ligation the ovum does not pass to the uterus so the sperm cells cannot reach it. 37. How does the contraceptive diaphragm work? What are the limitations of this contraceptive method? The contraceptive diaphragm is an artifact made of latex or plastic that when placed on the vaginal fundus covers the uterine cervix forbidding the passage of sperm cells through the cervical canal. To be more effective the diaphragm needs to be used together with spermicide. This method however does not prevent sexually transmitted diseases (STDs). 38. Why is the use of condoms not just a contraceptive method but also a health protection behavior? The use of condoms besides being an efficient contraceptive method also helps the prevention of diseases caused by sexually transmitted agents (STDs), like syphilis, gonorrhea, HPV (human papilloma virus that may lead to genital cancers) infestation, HIV infection, etc. 39. What is the normal duration of the menstrual cycle? How does the calendar contraceptive method work? The normal duration of the menstrual cycle is 28 days but it can vary among different women or in different cycles of the same woman. In the calendar contraceptive method the date n-14 (n minus 14) is taken considering n the number of days of the normal menstrual cycle of the woman (generally n=28). The safety margin +3 or –3 refers to the days around n-14 that intercourse should be avoided to prevent pregnancy. (This method is not exempt from failures. A doctor must always be consulted before relying on any contraceptive method.) 40. How is the ovulation date estimated with the control of the woman's body temperature? One method to estimate the exact ovulation day is daily control of the body temperature taken always under same conditions. At the ovulation day the body temperature often increases about 0.5 degrees centigrade. 41. What is the contraceptive mechanism of the IUD? The IUD (intrauterine device) is a piece of plastic coated with copper that is inserted within the uterus by a doctor. Copper is then gradually released (IUD may last 5 to 10 years) and since it has a spermicidal action sperm cells are destroyed before fecundation. Besides this mechanism the movement of the IUD inside the uterus causes slight endometrial inflammation that helps to prevent nidation. 42. Generally how does a male animal realize that the female is receptive to copulation? In most vertebrate species with internal fecundation the females have reproductive cycles with fertile periods. During this period the female secretes pheromones (odoriferous substances that attract the male of the species) from the skin and mucosae. The presence of the male individual and his pheromones also stimulates the release of pheromones by the female. (Many animals also use pheromones for territorial demarcation and for signal transmission between individuals about the location of dangers and food.) 43. What is parthenogenesis? Parthenogenesis is the reproduction or formation of a new individual from the egg cell but without fecundation by the male gamete. According to the species, individuals born by parthenogenesis may be male or female, or of any sex. In bees the drone (the single male bee) is haploid and born by parthenogenesis while the females (queen and workers) are diploid. Here are further guidelines. Reproductive System |
Skeletal System
|
How many total human skeletal bones are there? 206 bones on both side of the body What are various examples? Arms (2) Cranial (8) Facial (14) Feet (52) Forearms (4) Hands (54) Legs (6) Middle ears (6) Pelvis (4) Shoulder girdle (4) Thighs (2) Thorax (25) Throat (1) Vertebral column (24) www.qureshiuniversity.com/listofbonesofthehumanskeleton.html Why is it essential to know about total human skeletal bones? Any human bone can have a fracture or injury. How many total adult teeth are there? 32 What is the Skeletal System? How does the Skeletal System help us? Who has more bones a baby or and adult? Are bones alive? What is a bone made of? How do bones break and heal? What is an X-ray? What's up with joints? Does each bone have a name? How do I keep my bones healthy? Are my teeth counted as bones? Here are further guidelines. Skeletal System |
|
The Musculoskeletal System
Learn Cartilages, Bones and Muscles
1. Which are the organs that are part of the musculoskeletal system? The main organs and tissues that are part of the musculoskeletal system in humans are the cartilages, the bones and the muscles. 2. What are the functions of the musculoskeletal system? The musculoskeletal system has the functions of supporting and protecting organs, maintenance of the body spatial conformation, motion of organs, limbs and bodily portions and nutrient storage (glycogen in muscles, calcium and phosphorus in bones). 3. Which type of tissue are the cartilaginous and the osseous tissue? The cartilaginous and the osseous tissues are considered connective tissues since they are tissues in which the cells are relatively distant from others with a great amount of extracellular matrix in the interstitial space. 4. What are the cells that form the cartilaginous tissue? The main cells of the cartilages are the chondrocytes, originated from the chondroblasts that secrete the intersticial matrix. There are also chondroclasts, cells with many lisosomes and responsible for the digestion and remodelation of the cartilaginous matrix. 5. What is the constitution of the cartilaginous matrix? The cartilaginous matrix is made of collagen fibers, mainly collagen type II, and of proteoglycans, proteins associated to glycosaminoglycans, chiefly hyaluronic acid. The proteoglycans provide the typical rigidity of the cartilages. 6. What are some functions of the cartilages in the human body? Cartilages are responsible for the structural support of the nose and ears. The trachea and the bronchi are also organs with cartilaginous structures that prevent the closing of these tubes. In joints there are cartilages that cover the bones providing a smooth surface to reduce the friction of the joint movement. In the formation of bones the cartilages act as a mold and they are gradually substituted by the osseous tissue. 7. What are the three main cell types that form the osseous tissue? What are their functions? The three main cell types of the osseous tissue are the osteoblasts, the osteocytes and the osteoclasts. Osteoblasts are known as bone-forming cells since they are the cells that secrete the proteinaceous part of the bone matrix (collagen, glycoproteins and proteoglycans). The bone matrix is the intercellular space where the mineral substances of the bones are deposited. Osteocytes are differentiated mature osteoblasts formed after these cells are completely surrounded by the bone matrix. Osteocytes have the function of supporting the tissue. Osteoclasts are the giant multinucleate cells that remodelate the osseous tissue. They are originated from monocytes and they contain many lisosomes. Osteoblasts secrete enzymes that digest the osseous matrix creating canals throughout the tissue. 8. What is the bone matrix? What are its main components? Bone matrix is the content that fills the intercellular space of the osseous tissue. The bone matrix is made of mineral substances (about 5%), mainly phosphorus and calcium salts, and organic substances (95%), mainly collagen, glycoproteins and proteoglycans. 9. What are the Haversian canals and the Volkmann’s canals of the bones? Is the osseous tissue vascularized? The Haversian canals are longitudinal canals present in the osseous tissue within which blood vessels and nerves pass. The osseous tissue distributes itself in a concentric manner around these canals. The Volkmann’s canals are communications between the Harvesian canals. The osseous tissue is highly vascularized in its interior. 10. What are the functions of the osseous tissue? The main functions of the osseous tissue are: to provide structural rigidity to the body and to delineate the spatial positioning of the other tissues and organs; to support the body weight; to serve as a site for mineral storage, mainly of calcium and phosphorus; to form protective structures for important organs like the brain, the spinal cord, the heart and the lungs; to work as a lever and support for the muscles, providing movement; to contain the bone marrow where hematopoiesis occurs. 11. What are the flat bones and the long bones? The main bones of the body may be classified as flat or long bones (there are bones not classified into these categories). Examples of flat bones are the skull, the ribs, the hipbones, the scapulae and the sternum. Examples of long bones are the humerus, the radius, the ulna, the femur, the tibia and the fibula. 12. What are the types of muscle tissues? What are the morphological features that differentiate those types? There are three types of muscle tissue: the skeletal striated muscle tissue, the cardiac striated muscle tissue and the smooth muscle tissue. The striated muscles present under microscopic view transversal stripes and their fibers (cells) are multinucleate (in the skeletal) or may have more than one nucleus (in the cardiac). The smooth muscle does not present transversal stripes and it has spindle-shaped fibers each with only one nucleus. 13. Which is the type of muscle tissue that moves the bones? The bones are moved by the skeletal striated muscles. These muscles are voluntary (controlled by volition). 14. Which is the type of muscle tissue that contracts and relaxes the heart chambers? The myocardium of the heart is made of cardiac striated muscle tissue. 15. Which is the type of muscle tissue that performs the peristaltic movements of the intestines? The smooth muscle tissue is responsible for the peristaltic movements of the intestines. The smooth muscles are not controlled by volition. 16. Which is the type of muscle tissue that helps to push the food down through the esophagus? The esophageal wall in its superior portion is made of skeletal striated muscle. The inferior portion is made of smooth muscle. In the intermediate portion there are skeletal striated and smooth muscles. All of these muscles are important to push the food down towards the stomach. 17. How is the striped pattern of the striated muscle cells formed? The functional units of the muscle fibers are the sarcomeres. Within the sarcomeres blocks of actin and myosin molecules are posed in organized manner. The sarcomeres align in sequence forming myofibrils that are longitudinally placed in the cytoplasm of the muscle fibers (cells). The grouping of consecutive blocks of actin and myosin in parallel filaments creates the striped pattern of the striated muscle tissue seen under the microscope. 18. What are sarcomeres? Sarcomeres are the contractile units of the muscle tissue formed of alternating actin blocks (thin filaments) and myosin blocks (thick filaments). Several sarcomeres placed in linear sequence form a myofibril. Therefore one muscle fiber (cell) has many myofibrils made of sacomeres. The compartments where myofibrils are inserted are delimited by an excitable membrane known as sarcolemma. The sarcolemma is the plasma membrane of the muscle cell. 19. What are the main proteins that constitute the sarcomere? What is the function of those molecules in the muscle cells? In the sarcomere there are organized actin and myosin blocks. Troponin and tropomyosin also appear associated to actin. The actin molecules when activated by calcium ions liberated in the proximities of the sarcomere are pulled by myosin molecules. This interaction between actin and myosin shortens the myofibrils originating the phenomenon of muscle contraction. 20. What are the positions of actin and myosin molecules in the sarcomere before and during the muscle contraction? Schematically actin filaments attached perpendicularly to both sarcomere extremities (longitudinal sides) make contact with myosin filaments positioned in the middle of the sarcomere and in parallel to the actin filaments. Before the contraction the sarcomeres are extended (relaxed) since the contact between actin and myosin filaments is only made by their extremities. During contraction actin filaments slide along the myosin filaments and the sarcomeres shorten. 21. How do calcium ions participate in muscle contraction? Why do both muscle contraction and muscle relaxation spend energy? In the muscle cells calcium ions are stored within the sarcoplasmic reticulum. When a motor neuron emits stimulus for the muscle contraction neurotransmitters called acetylcholine are released in the neuromuscular junction and the sarcolemma is excited. The excitation is conduced to the sarcoplasmic reticulum that then realeases calcium ions into the sarcomeres. In the sarcomeres the calcium ions bind to troponin molecules associated to actin activating myosin binding sites of actin. The myosin, then able to bind to actin, pulls this protein and the sarcomere shortens. The summation of simultaneous contraction of sarcomeres and myofibrils constitutes the muscle contraction. During muscle relaxation the calcium ions return back to the sarcoplasmic reticulum. For myosin to bind to actin, and thus for the contraction to occur, hydrolysis of one ATP molecule is necessary. During relaxation the return of calcium ions to the sarcoplasmic reticulum is an active process that spends ATP too. So both muscle contraction and relaxation are energy-spending processes. 22. What is myoglobin? What is the function of this molecule in the muscle tissue? Myoglobin is a pigment similar to hemoglobin and present in muscle fibers. Myoglobin has a great affinity for oxygen. It keeps oxygen bound and releases the gas under strenuous muscle work. So myoglobin acts as an oxygen reserve for the muscle cell. 23. How does phosphocreatine act in the muscle contraction and relaxation? Phosphocreatine is the main means of energy storage of the muscle cells. During relaxed periods ATP molecules made by the aerobic cellular respiration transfer highly energized phosphate groups to creatine forming phosphocreatine. In exercise periods phosphocreatine and ADP resynthesize ATP to dispose energy for the muscle contraction. 24. What happens when the oxygen supply is insufficient to maintain aerobic cellular respiration during muscle exercise? If oxygen from hemoglobin or myoglobin is not enough for the energy supply of the muscle cell the cell then begins to do lactic fermentation in an attempt to compensate the deficiency. The lactic fermentation releases lactic acid and this substance causes muscle fatigue and predisposes the muscles to cramps. 25. What is the neurotransmitter of the neuromuscular junction? How does the nervous system trigger muscle contraction? The nervous cells that trigger the muscle contraction are the motor neurons. The neurotransmitter of the motor neurons is acetylcholine. When a motor neuron is excited the depolarizing current flows along the membrane of its axon until reaching the synapse at the neuromuscular junction (the neural impulse passage zone between the axon extremity and the sarcolemma). Near the axonal extremity the depolarization allows the entrance of calcium ions into the axon (note that calcium also has a relevant role here). The calcium ions stimulate the neuron to release acetylcholine in the synapse. Acetylcholine then binds to special receptors in the outer surface of the sarcolemma, the permeability of this membrane is altered and an action potential is created. The depolarization is then conduced along the sarcolemma to the sarcoplasmic reticulum that thus releases calcium ions for the sarcomere contraction. 26. To increase the strength of the muscle work is the muscle contraction intensely increased? An increase in the strength of the muscle work is not achieved by increase in the intensity of the stimulation of each muscle fiber. The muscle fiber obeys an all-or-nothing rule, i.e., its contraction strength is only one and cannot be increased. When the body needs to increase the strength of the muscle work a phenomenon known as spatial summation occurs: new muscle fibers are recruited in addition to the fibers already in action. So the strength of the muscle contraction increases only when the number of active muscle cells increases. 27. What is the difference between spatial summation and temporal summation of muscle fibers? What is tetany? Spatial summation is the recruiting of new muscle fibers to increase the muscle strength. Temporal summation occurs when a muscle fiber is continuously stimulated to contract without being able to conclude relaxation. The permanence of a muscle fiber under a continuous state of contraction by temporal summation is known as tetany (e.g., the clinical condition of patients contaminated by the toxin of the tetanus bacteria). Tetany ends when all available energy for contraction is spent or when the stimulus ceases. |
Urinary system
| A List of Kidney Diseases |
| Human Biology: Excretory System |
|
Human Biology: Excretory System
The Excretory System The Excretory System - Get the Knowledge 1. Which are the organs of the excretory system? The excretory system is formed of kidneys (two), ureters (two), bladder and urethra. 2. What are nitrogen wastes? Nitrogen wastes are residuals derived from the degradation of proteins. They are made from chemical transformation of the amine group of amino acid molecules. 3. What are the three main types of nitrogen wastes excreted by living beings? The main nitrogen wastes excreted by living beings are ammonia, uric acid and urea. Living beings that secrete ammonia are known as ammoniotelic. Creatures that secrete uric acid are known as uricotelic. Organisms that secrete urea are called ureotelic. 4. Why are most ammoniotelic beings aquatic animals? Aquatic animals, like crustaceans, bony fishes and amphibian larvae, generally are ammoniotelic since ammonia diffuses more easily through membranes and it is more water-soluble than the other nitrogen wastes. Ammonia is still the most energetically economical nitrogen waste to be synthesized. 5. Why after the passage of animals from the aquatic to the terrestrial habitat does the abandonment of the ammoniotelic excretion occur? Ammonia is a highly toxic molecule if not diluted and quickly excreted out of the body. For this reason the ammoniotelic excretion was abandoned in terrestrial habitats because the availability of water for dilution is reduced in this medium and wastes cannot be excreted so promptly to the exterior. 6. Comparing toxicity and the need for dilution in water how different are the ureotelic and the uricotelic excretions? What are some examples of animals that present these respective types of excretion? Urea is more water-soluble than uric acid (an almost insoluble substance). Urea is also more toxic. Both however are less toxic than ammonia. Some invertebrates, chondrichthian fishes, adult amphibians and mammals are ureotelic. Reptiles, birds and most arthropods are uricotelic. 7. What is the nitrogen waste in amphibian larvae and in the adult animal? Since amphibian larvae are aquatic they excrete ammonia. The terrestrial adult excretes urea. 8. Why is the uricotelic excretion essential for avian and reptile embryos? In reptiles and birds the excretory system is uricotelic since uric acid is insoluble, less toxic and suitable to be stored within the eggs where their embryos develop. 9. How do embryos of placental mammals excrete nitrogen wastes? Placental animals, including embryos, excrete urea. In the adult placental mammal urea is excreted through the urine. In embryos the molecule passes to the mother’s blood through the placenta and it is excreted in the mother’s urine. 10. What is the main nitrogen waste of humans? Human beings excrete mainly urea eliminated with the urine. 11. How is urea formed in the human body? Urea is a product of the degradation of amino acids. In the process amino acids lose their amine group which is then transformed into ammonia. In the liver ammonia reacts with carbon dioxide to form urea and water, a process called ureogenesis. In the intermediary reactions of the ureogenesis a molecule of ornithine is consumed and another is produced. For this reason ureogenesis is also known as the ornithine cycle. 12. What is excretion? Excretion in Physiology is the process of elimination of metabolic wastes and other toxic substances from the body. 13. What are the vessels that carry blood to the kidneys? Is this blood arterial or venous? The arterial vessels that carry blood to be filtrated by the kidneys are the renal arteries. The renal arteries are ramifications of the aorta and so the blood filtered by the kidneys is arterial (oxygen-rich) blood. 14. Which are the vessels that drain filtered blood from the kidneys? The venous vessels that collect the blood filtered by the kidneys are the renal veins. The renal veins carry the blood that has been reabsorbed in the nephron tubules. 15. What is the functional unity of the kidneys? The functional (filtering) unity of the kidneys is the nephron. A nephron is made of afferent arteriole, efferent arteriole, glomerulus, Bowman's capsule, proximal tubule, loop of Henle, distal tubule and collecting duct. In each kidney there are about one million nephrons. 16. What are the three main renal processes that combined produce urine? Urine is made by the occurrence of three processes in the nephron: glomerular filtration, tubular resorption and tubular secretion. In the nephron the blood carried by the afferent arteriole enters the glomerular capillary network where it is filtered. The filtration implies that part of the blood returns to the circulation through the efferent arteriole and the other part, known as the glomerular filtrate, enters the proximal tubule of the nephron. In the nephron tubules (also known as convoluted tubules) substances of the glomerular filtrate like water, ions and small organic molecules are resorbed by the cells of the tubule wall and gain again the circulation. These cells also secrete other substances inside the tubules. The urine is formed of not resorbed filtered substances and of secreted (by the tubules) substances. Urine is drained by the collecting ducts to the ureter of each kidney, then it enters the bladder and later it is discharged through the urethra. The nephron tubules are surrounded by an extensive capillary network that collects resorbed substances and provides others to be secreted. 17. What is the main transformation presented by the glomerular filtrate in comparison to the blood? Glomerular filtrate is the name given to the plasma after it has passed the glomerulus and entered the Bowman’s capsule. The glomerular filtrate has a different composition compared to urine since the fluid has not yet undergone tubular resorption and secretion. The main difference between the blood and the glomerular filtrate is that in the latter the amount of proteins is at a minimum and there are no cells or blood platelets. 18. What is proteinuria? Why is proteinuria a sign of glomerular renal injury? Proteinuria means losing of proteins through urine. Under normal conditions proteins are too big to be filtered by the glomerulus and they are practically absent in the urine (the few filtered proteins may also be resorbed in the nephron tubules). Proteinuria is an indication that a more than expected amount of proteins is passing the glomerulus suggesting glomerular disease, e.g., in diabetic nephropathy. The glomerulus also blocks the passage of blood cells and platelets (hematuria is often a sign of urinary disease although less specific of kidneys since the blood may come from the lower parts of the excretory tract). 19. Where does most of the water resorbed after glomerular filtration go? What are the other substances resorbed by the nephron tubules? Only 0.5 to 1% of the glomerular filtrate is eliminated as urine. The remaining volume, containing mainly metabolic ions, glucose, amino acids and water, is resorbed through the nephron tubules (by means of active or passive transport) and gains the blood circulation again. The convolute tubules of the nephron are responsible for the resorption of substances. The Excretory System - Image Diversity: nephron tubules 20. Why do cells of the nephron tubules present a great amount of mitochondria? The cells of the tubule wall have high number of mitochondria because many substances are resorbed or secreted through them by means of active transport (a process that spends energy). Therefore many mitochondria are necessary for the energetic supply (ATP supply) of this type of transport. 21. What is tubular secretion? What are some examples of substances secreted through the renal tubules? Tubular secretion is the passage of substances from the blood capillaries that surround the nephron tubules to the tubular lumen for these substances to be excreted with urine. Ammonia, uric acid, potassium, bicarbonate and hydrogen ions, metabolic acids and bases, various ingested drugs (medicines) and other substances are secreted by the nephron tubules. 22. In which nephron portion does the regulation of acidity and alkalinity of the plasma occur? The regulation of the acid-basic equilibrium of the body is done by the kidneys and depends upon the tubular resorption and secretion. 23. How do kidneys participate in the regulation of the acid-basic equilibrium of the body? How are alkalosis and acidosis respectively corrected by the kidneys? Kidneys can regulate the acidity or alkalinity of the plasma varying the excretion of hydrogen and bicarbonate ions. In alkalosis (abnormally high level of the plasma pH) the kidneys excrete more bicarbonate and the equilibrium of formation of bicarbonate from water and carbon dioxide shifts towards formation of more hydrogen ions and bicarbonate and then the plasma pH is lowered. When the body undergoes acidosis (abnormal low level of the plasma pH) the kidneys excrete more hydrogen ions and retain more bicarbonate thus the equilibrium of formation of bicarbonate from water and carbon dioxide shifts towards more hydrogen consumption and the plasma pH is increased. 24. How do kidneys participate in the blood volume control? How is the blood volume of the body related to the arterial pressure? The kidneys and the hormones that act upon them are the main physiological regulators of the total blood volume of the body. As more water is resorbed in the nephron tubules the more the blood volume increases; as more water is excreted in urine the more the blood volume lowers. The blood volume in its turn has a direct relation to blood pressure. The blood pressure increases when the blood volume increases and it lowers when the blood volume lowers. That is the reason why one of the main groups of antihypertensive drugs is the diuretics. Doctors often prescribe diuretics for the hypertensive patients to excrete more water and thus lower their blood pressure. 25. Which are the three hormones that participate in the regulation of the renal function? Antidiuretic hormone (or ADH, or vasopressin), aldosterone and atrial natriuretic factor (or ANF) are hormones that participate in the regulation of the excretory system. 26. What is the function of the antidiuretic hormone? Where is it made and which are the stimuli that increase or reduce its secretion? The antidiuretic hormone is secreted by the hypophysis (also known as pituitary) and it acts in the nephron tubules increasing the resorption of water. When the body needs to retain water, for example, in cases of blood loss and abrupt blood pressure lowering or in cases of abnormally high blood osmolarity, there is stimulus for ADH secretion. When the body has an excess of water, as in cases of excessive ingestion or in abnormally low blood osmolarity, the secretion of ADH is blocked and the diuresis increases. ADH is also known as vasopressin since it increases the blood volume and thus heightens the blood pressure. 27. Why does the ingestion of alcohol increase diuresis? Alcohol inhibits the secretion of ADH (antidiuretic hormone) by the pituitary. That is why when it is drunk to excess the person urinates too much. 28. How does aldosterone act and where is it produced? Aldosterone is a hormone that acts upon the nephron tubules stimulating the resorption of sodium. Therefore it contributes to the increase of the blood osmolarity and consequently to the increase of the blood pressure. Aldosterone is made by the adrenals, glands located over the superior portion of the kidneys. 29. What is an evolutionary explanatory hypothesis for the secretion by the heart of a hormone that regulates the renal function? Which is that hormone? The renal regulator hormone secreted by the heart is the atrial natriuretic factor (or ANF). The ANF increases the excretion of sodium in the nephron tubules causing less resorption of water, more urinary volume, and thus lowering the blood pressure. The atrial natriuretic factor is secreted when there is an increase of the length of the heart muscle fibers in response to high blood pressure. The ANF is a natural antihypertensive substance. Since the health of the heart depends largely upon the stability of the normal blood pressure the evolution should have preserved the atrial natriuretic factor to allow information from the heart to be an additional mechanism for the renal control of the blood pressure. 30. What is hemodialysis? Hemodialysis is the artificial blood filtration made by specific machines in substitution of the kidneys. Hemodialysis may be necessary in patients suffering from diseases that cause renal failure, like diabetic renal complications, lupic renal complications and others. During hemodialysis the blood of the patient is deviated to the filtering machine and after the filtration it returns to the body. Hemodialysis is generally done two, three or more times a week in a process that takes several hours. Sometimes kidney transplantation is an alternative to hemodialysis. 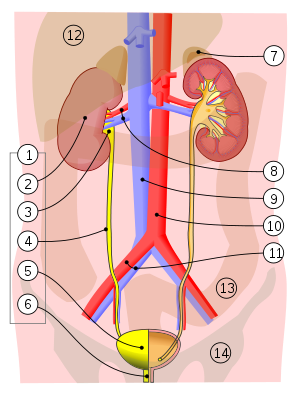
Urinary System 1. Human urinary system: 2. Kidney, 3. Renal pelvis, 4. Ureter, 5. Urinary bladder, 6. Urethra. (Left side with frontal section) 7. Adrenal gland Vessels: 8. Renal artery and vein, 9. Inferior vena cava, 10. Abdominal aorta, 11. Common iliac artery and vein With transparency: 12. Liver, 13. Large intestine, 14. Pelvis The order of impurities being excreted from the kidneys: Kidneys ? Ureters ? Urinary Bladder ? Urethra Lower urinary tract symptoms Filling or irritative symptoms Increased frequency of urination Increased urgency of urination Painful urination Excessive passage of urine at night Voiding or obstructive symptoms Poor stream Hesitancy Terminal dribbling Incomplete voiding Overflow incontinence (occurs in chronic retention) Causes Benign prostatic hyperplasia (BPH) with obstruction Detrusor muscle weakness and/or instability Urinary Tract Infection (UTI) Chronic prostatitis Urinary stone Malignancy: prostate or bladder Neurological disease, e.g. multiple sclerosis, spinal cord injury, cauda equina syndrome Symptoms of Chronic Kidney Disease Most people do not have any severe symptoms until their kidney disease gets worse. However you may: Have muscle cramps at night Have swollen feet and ankles Have puffiness around your eyes, especially in the morning Feel more tired Have less energy Have trouble thinking clearly Have a poor appetite Have trouble sleeping Have dry, itchy skin Need to urinate more often, especially at night. A List of Kidney Diseases
|
Issues Primary Care Physician on Duty Has to Manage
What issues does the primary care physician on duty have to manage?
|
|
What is needs assessment? Human rights have to be the main focus of needs assessment. Needs assessment can be at an individual level and/or a community level. A needs assessment is a systematic process for determining and addressing needs, or "gaps" between current conditions and desired conditions. Needs assessment has to be done in all human healthcare settings. How do you proceed with a needs assessment? Gather data to define needs. Identify concerns. Identify and analyze the causes. List consequences if the cause is not removed. Enter a rating (low, medium, high) of the difficulty of correcting the problem. Decide on priorities. Identify possible solutions and/or remedies. Prepare a plan. In what situations are needs assessments required?
Yes. What is the difference between needs assessment and survival needs assessment? Needs assessment is a big entity. Within needs assessment is survival needs assessment. Take a look at this. http://www.qureshiuniversity.com/survivalneeds.html These are the questions to be answered in survival needs assessment. Take a look at this. http://www.qureshiuniversity.com/needsassessment.html These are the questions to be answered in detailed needs assessment. No competent primary care physicians exist in the community. This is a need of an individual. This may not be an emergency; however, need of an individual is a need. What do I feel needs to be included in needs assessment? Needs assessment has to be done under the supervision of a physician. A care coordinator, physician assistant, counselor, or nurse can do a needs assessment under supervision of a physician. What aspects of a needs assessment are important to its success? Relevant questions and truthful answers. What steps are involved in conducting a needs assessment? Questions to be asked in needs assessment. What questions should be asked in needs assessment? What are your needs? -------------------------------------- What is the name of individual whose needs assessment has to be done? -------------------------------------- What is the date of birth of the individual whose needs assessment is to be done? -------------------------------------- What is the profile of the individual? -------------------------------------- Your profile. Your social support network. Your health care provider’s profile. Activities of everyday living assessment. Your survival needs details. How does a profile look? Here are further guidelines. Are these survival needs or nonsurvival needs? -------------------------------------- Do you think these are emergency or nonemergency needs? -------------------------------------- What department in the state has a duty to resolve these issues? -------------------------------------- What needs to be done immediately? -------------------------------------- What can be done later? -------------------------------------- |
Advice relevant to remaining healthy.
|
What advice is there for an individual to maintain good health? Consume a balanced diet every day. Do not take tea or coffee (weight loss occurs). Do not consume over the counter medication even if freely available, for example ibuprofen. Do not consume fish that has a bone that is difficult to remove. Do not consume frozen meat like liver that has been there for months or years. Do not smoke or consume alcohol. Exercise every day. Maintain a healthy relationship. Maintain a healthy environment. Stress can harm an individual. Decrease stress. Tea Do not consume tea every day. Consuming tea everyday leads to weight loss. In what situations tea should be consumed? If you have a sore throat, tea helps. Consume hot tea for sore throat with sugar or salt, Lipton or Namkeen tea, for at least an hour 2-4 cups slowly for 2-4 days during sore throat. Consume tea if you have constipation. Normally, consume tea after every 4 months. |
Mental health and role of primary care physician.
|
What should a primary care physician know about mental health? A primary care physician should know everything about mental health. A primary care physician should rarely refer a case that is a diagnostic puzzle. Questions you need to answer in the referral. What complaints, issues, and problems did the individual present to you that need referral? What complaints, issues, and problems do not need a referral? If an individual feels stressed, this does not need referral from primary care physician to another physician of different abilities. Here are further guidelines. http://www.qureshiuniversity.com/psychiatryworld.html |
Community health center
What staff is usually at a community health center?
It should be mandatory that an area have at least one doctor, one nurse, and one counselor for every 300 individuals at a community health center. (Community health center) What are other names for a community health center? Dispensary Managed Care Integrated Care Program (ICP) Primary care providers (or PCPs) Primary Care Case Management (PCCM) Voluntary Managed Care (VMC) What services are usually provided by a community health center?
|
Program Director
Program Director for this primary care physician training program.
|
What is a program director? A program director researches, plans, develops, implements, and circulates one or more of the professional training programs or professional services. What types of training programs can a program director offer? Here are various examples. I have training programs for 611 professions. This includes training programs for physicians, teachers, lawyers, and engineers. I have guidelines for 43 departments in the state and outside the state. Who is the program director of this primary care physician training program? Doctor Asif Qureshi. What other programs does Doctor Asif Qureshi guide? I have training programs for 611 professions. This includes training programs for physicians, teachers, lawyers, and engineers. I have guidelines for 43 government departments in the state and outside the state. This all is available up to various extents publicly. Improvements of this program. Primary care physician training program. What suggestions do you have to improve this program? |
STDs (Sexually Transmitted Diseases)
|
What are sexually transmitted diseases (STDs)?
Chlamydia Chancroid Ectoparasitic Infections Genital herpes Gonorrhea Hepatitis B Hepatitis C Human papilloma virus/Genital warts Syphilis How Can I Protect Myself From STDs? Here are some basic steps that you can take to protect yourself from STDs: •Consider that not having sex or sexual relations (abstinence) is the only sure way to prevent STDs. •Use a latex condom every time you have sex. (If you use a lubricant, make sure it is water-based.) •Limit your number of sexual partners. The more partners you have, the more likely you are to catch an STD. •Practice monogamy. This means having sex with only one person. That person must also have sex with only you to reduce your risk. •Choose your sex partners with care. Don't have sex with someone whom you suspect may have an STD. And keep in mind that you can't always tell by looking if your partner has an STD. •Get checked for STDs. Don't risk giving the infection to someone else. •Don't use alcohol or drugs before you have sex. You may be less likely to use a condom if you are drunk or high. •Know the signs and symptoms of STDs. Look for them in yourself and your sex partners. •Learn about STDs. The more you know, the better you can protect yourself. Here are further guidelines. |
Symptoms and complaints relevant to human health.
|
What best describes symptoms or complaints relevant to human health? Nonemergency medical symptoms or complaints. Emergency medical symptoms or complaints. Why should a physician know everything about symptoms or complaints relevant to human health? Correct diagnosis and treatment is based on proper analysis of symptoms or complaints relevant to human health in various healthcare setting. What can be symptoms or complaints relevant to the human brain and central nervous system? What can be symptoms or complaints relevant to the human circulatory system? What can be symptoms or complaints relevant to the human digestive system? What can be symptoms or complaints relevant to the human endocrine system? What can be symptoms or complaints relevant to the human integumentary system? What can be symptoms or complaints relevant to the human lymphatic system? What can be symptoms or complaints relevant to the human muscular system? What can be symptoms or complaints relevant to the human reproductive system? What can be symptoms or complaints relevant to the human respiratory system? What can be symptoms or complaints relevant to the human skeletal system? What can be symptoms or complaints relevant to the human urinary system? What can be symptoms or complaints relevant to human environmental harms issues? Survival needs issues Abuse issues Trauma issues Other harms. Fever or pain that is recurrent or new can be symptoms or complaints relevant to any human body system. Here are further facts. Nonemergency medical symptoms or complaints. Brain & Nervous System
Duchenne muscular dystrophy Signs and symptoms typically appear between the ages of 2 and 3, and may include: Frequent falls Here are further guidelines. http://www.qureshiuniversity.com/emergencymedicalservices.html |
Value and benefits of these services to others.
|
What should you know about value and benefits of these services to others? Compare these services to others services with cost of other service and you will realize the value and benefits of these services. Value of these services to existing physician, new physician and healthcare systems. Up to April 21, 2015, there were hardly any such programs publicly available on the Internet and free to existing physicians, new physicians and healthcare systems. Value of these services to patient, relatives, and well-wishers of patient. Here are various examples. Why is there need to elaborate on these issues? On April 5, 2015, on Argyl and Winthrop in Chicago, Illinois 60640, a local resource physician was asking for $60 for one sore throat consultation. On March 29, 2015, on Broadway and Argyl in Chicago, Illinois 60640, a local resource dentist was asking for $200 for one consultation of tooth pain. Take a look at this. A simple consultation is approximately $800. A comprehensive consultation is almost always less than $1,500. Who has displayed these types of consultations? Gateway Psychiatric Services 548 Market St # 18351 San Francisco, CA 94104-5401 On March 10, 2014, at 3.20 PM, this was verified. Take a look at this. http://www.qureshiuniversity.com/psychiatryworld.html Have you look at this resource to verify if your questions and concerns have been answered? If you go through this resource, you will realize there is no need for $800 consultation or $1,500 comprehensive psychiatric consultation. Are you ready to get started, or do you have other questions about the Internet consultation? Have you read the facts about the services you are getting? Everything is displayed publicly. There is no hidden agenda. There is no professional damages for these services through www.qureshiuniversity due to the fact that everything is displayed publicly for scrutiny by any professional. If any individual or professional feels any professional abilities need to be added, he or she can forward recommendations. How is this resource – www.qureshiuniversity.com – better than other resources? At this resource, all advice services are free to public. At the same time, the resource should get grants from the system in the state or outside the state. |
Low or high medical lab results
|
Guidelines on Professional Training. Guidelines on Continuous Professional Training. What should a physician do if low or high medical lab results are reported? Do not panic. Analyze and interpret results in a reasonable scientific manner. Correlate with medical history and clinical findings. Start with normal value ranges. Consider blood collection error, storage error, lab error, life style changes like diet and exercise, medications, and other reasons. Last of all, interpret low to high value medical lab results with any specific diagnosis after evaluating all of the above reasons. Answer relevant questions. What standard of human blood serum chemistry normal values do you follow? What standard of human blood serum chemistry normal values do I follow? http://www.qureshiuniversity.com/BloodSerumChemistryNormalValues.pdf What are the sources of these human blood serum chemistry normal values? Food and Drug Administration 10903 New Hampshire Avenue Silver Spring, MD 20993 Primary care physician training program What is the difference between a primary care physician training program and a primary care physician on duty at a location? Establishing a training program for primary care physicians and working at a specific location 9-5 as a primary care physician are two different services. Medical Records Technician Training http://www.qureshiuniversity.com/medicalrecordsandhealthInformationtechnician.html Medical Assistant http://www.qureshiuniversity.com/medicalassistant.html Medical Laboratory Technician http://www.qureshiuniversity.com/medicallaboratorytechnician.html Biochemistry lab errors verification What are the most common reasons lab values of biochemistry result are low or high? Improperly collected blood samples. Improper tube in which human blood was collected. Improper storage of blood samples. Wrong machine analysis or sample. Transient low or high values caused by lifestyle, like diet, exercise, medication, other reasons. At the end, you should consider other medical reasons. How do you collect samples for human blood chemistry analysis? How many tubes and types of tubes do you utilize in collecting samples for biochemistry analysis? How do you verify that the biochemistry lab is not giving any errors? Where do you forward the blood samples for biochemistry analysis? What types of machines in biochemistry do analysis of human blood samples? Low or high medical lab results Here are further guidelines. |
Prescriptions and recommendations by a primary care physician differ.
|
Is there a difference between a prescription and a written recommendation by a primary care physician? Yes. What is the difference between a prescription and a written recommendation by a primary care physician? A prescription is a piece of paper or document that a doctor gives you that says what type of medication you need dispensed by a pharmacist. A written recommendation by a primary care physician need not be presented to a pharmacist. Required medication can be obtained over the counter. Must a prescription by a primary care physician always be dispensed by a pharmacist? No. What is the proof that a prescription by a primary care physician does not always have to be dispensed by a pharmacist? Problems, Issues: Cough, pain in the throat when swallowing. Diagnosis: Upper respiratory infection. Prescription for Treatment: Your current medication list: 600 mg of Ibuprofen, 1 by mouth every 6 hours as needed and 500 mg of Amoxicillin, 1 by mouth 3 times a day Pharmacy: For example, Osco Pharmacy, 5343 North Broadway, Chicago, Illinois 60640 Telephone: (773) 784-1922 Six days without any improvement. This is prescription medication. Written recommendations by a primary care physician do not need to be presented to a pharmacist. Medication and other required products can be obtained over the counter. Improvement within 2 hours of medication. This is over-the-counter medication. Assured Multi-Symptom Day & Night Cold Formula, 12-ct. Active ingredients in cough and cold medicines. How is this medication better than other medications for cough, cold, and pain? Improvement occurs in 2 to 4 hours. Nighttime formula Acetaminophen 325mg acetaminophen (pain reliever/fever reducer) Chlorpheniramine maleate (antihistamine) 2mg chlorpheniramine maleate (antihistamine) Dextromethorphan 10mg dextromethorphan HBr (cough suppressant) Phenylephrine 5mg phenylephrine HCI (nasal decongestant) per caplet Non-drowsy daytime formula Acetaminophen 325mg acetaminophen (pain reliever/fever reducer) Dextromethorphan 10mg dextromethorphan HBr (cough suppressant) Phenylephrine 5mg phenylephrine HCI (nasal decongestant) per caplet Assured Multi-Symptom Day & Night Cold Formula, 12-ct.
|
Primary care physician or guide is not feeling well.
|
Can a primary care physician need a consultation with another primary care physician? Yes. Can a guide for a primary care physician need a consultation with another primary care physician? Yes. When does a guide to a primary care physician or a primary care physician need a consultation with another primary care physician? Problem issues can range from any problem that does not get relieved like an upper respiratory infection to any required referral. |
Emergency and nonemergency human healthcare complaints.
|
How does a primary care physician or the medical emergency room or other types of physicians know if this is an emergency or a nonemergency human healthcare complaint? You have to learn and gain experience. A–Z alphabetical listing of human health emergency symptoms and signs. http://www.qureshiuniversity.org/medicalemergencysymptoms.html All human symptoms and signs. http://www.qureshiuniversity.org/symptoms.html Nonemergency human healthcare complaints. www.qureshiuniversity.com/ |
Medical biochemistry
Human Healthcare
|
Debate questions for existing medical doctors (MDs) What is the range of normal human biochemistry laboratory values? What range of normal human biochemistry laboratory values do I follow? Food and Drug Administration (FDA) 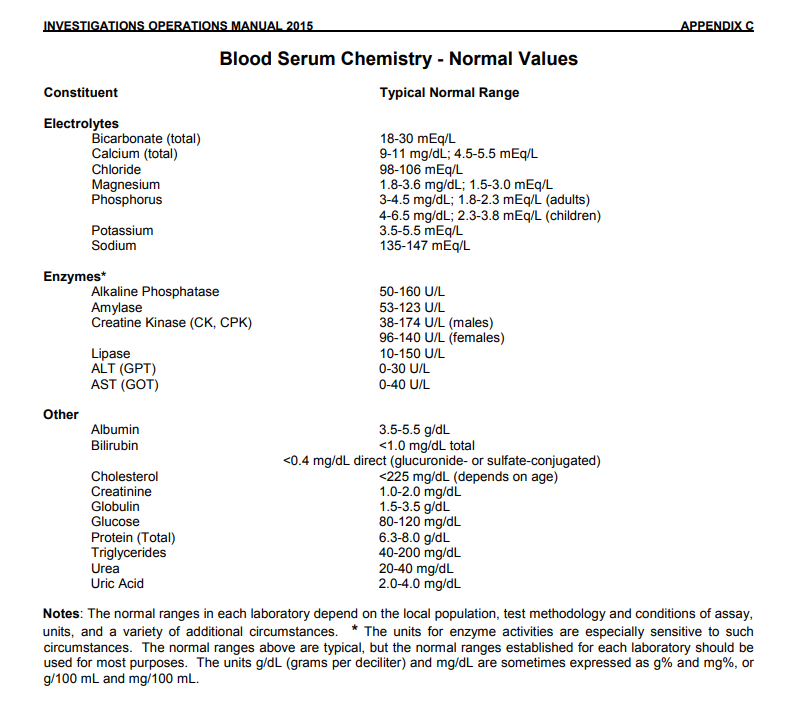 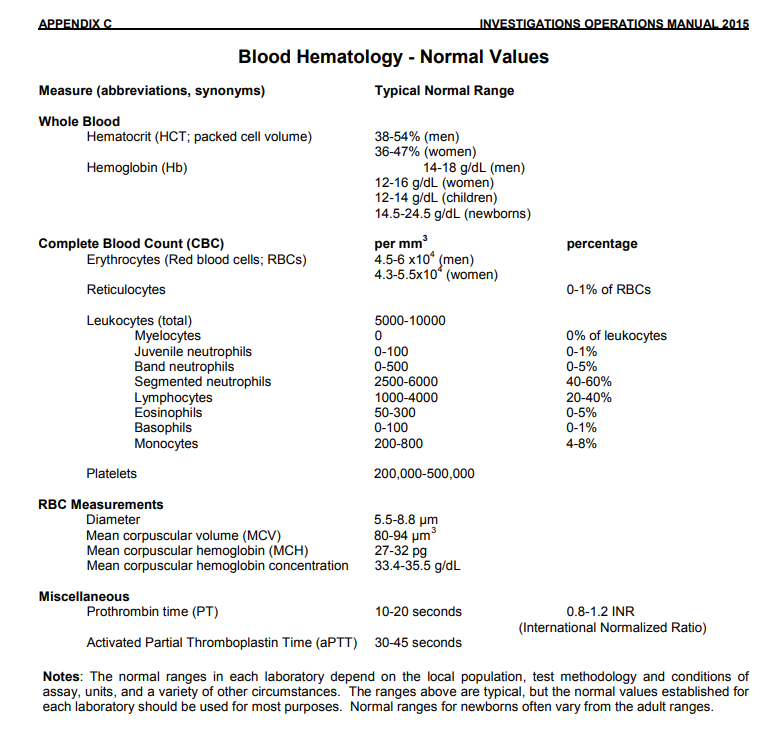 What ranges of normal human biochemistry values do you follow? What is the proof that you are following accurate normal human biochemistry laboratory value ranges? What is the proof that your laboratory is not giving error values? Why is it required to be able to walk into biochemistry laboratories in every community where biochemistry tests can be done at least once a year without a physician’s order? Due to discrepancies in test results, the independent verification of normal ranges is always required. For example, in the 60640 zip code in Chicago, Illinois, an independent biochemistry lab is required where individuals can walk in once a year to get biochemistry testing without any physician’s order. LabCorp has failed to answer relevant questions, including the normal range, presented to it with reference to the Food and Drug Administration. The quality of physicians in America is worsening. How is new method of Internet medical education for aspiring, in training, and existing medical doctors (for example, www.qureshiuniversity.com/health.html) better than previous old methods? How do you become a medical doctor through the new method of online training of aspiring and in training medical doctors? Take a look at this. Www.qureshiuniversity.org/physicians.html Everything is displayed at these resources. Grants are required to enhance the educational resources at Qureshi University (www.qureshiuniversity.org). What range of normal human biochemistry laboratory values do I follow? www.qureshiuniversity.com/health.html What do you have to do? If your human biochemistry laboratory value ranges are different, you need to consult the head of the laboratory. Update them about actual facts from the Food and Drug Administration so that the standardization of normal values goes ahead as per the values displayed in the Food and Drug Administration’s document. Here are further guidelines. https://qureshiuniversity.com/health.html#Medical biochemistry laboratory |
Counseling services.
|
Why should counseling be done under the supervision of a competent medical doctor? Counseling is part of a treatment. If there is no correct diagnosis, adding this part of the treatment can be harmful. What will happen if counseling is done without the supervision of a competent medical doctor? Counseling without supervision of a competent medical doctor can be harmful. All counseling without supervision of competent medical doctors should be banned. Here is a case scenario of counseling. What seems to be the complaint or problem? I feel stressed. I feel angry. I feel restless. What causes it? The answer to this question is essential to fix the underlying cause. Fix the underlying cause. There are more than 180 life stressors. All causes of stress do not need medication or hospitalization. Some of these issues can be fixed via Internet. Counseling helps in stress-related issues. Counseling can be done via Internet, telephone, fax, postal mail, or face-to-face sessions. What do you think causes it? What do I think causes it? A medical doctor with a counselor will ask relevant questions and answer this question. What questions should a medical doctor be able to answer in the context of recommendations for counseling? The medical doctor has to answer these questions. How long should the counseling last? How many sessions should there be per week and what should be the duration of sessions? What is the diagnosis? How did the doctor reach this diagnosis? What type of counseling does this person need? | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Counseling
Before starting counseling, a counselor should be able to answer the following questions. Q: Who needs counseling? Q: Why does he/she need counseling? Q: What should be the end result? Q: What kind of counseling will you need? | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Counseling Skills
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Counseling guidelines for counselors | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Community counseling centers | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Counseling Resources |
Statistics relevant to primary care physicians in various states.
|
What are the statistics for primary care physicians by state? State of Illinois had 19,841 primary care physicians on March 11, 2016. State of California had 48,852 primary care physicians on March 11, 2016. State of New Jersey had 13,393 primary care physicians on March 11, 2016. Many more primary care physicians are required in every state. |
|
Do you know any other program better than this program? How is any other program better than this program? |